According to American Diabetes Association, diabetes is classified as type I diabetes due to an absolute deficiency of insulin secretion and type 2 diabetes due to a combination of resistance to insulin action and an inadequate compensatory insulin secretory response [1].
In 1977, Irvine WJ et al., showed that 11% of individuals initially diagnosed with T2DM have antibodies against the insulin producing β-cells, which is a characteristic of type 1 diabetes and indicative of an autoimmune pathogenesis [2]. Tuomi T et al., introduced the term LADA in the year 1993 to describe above subgroup of patients who shared phenotypical features with type 2 diabetes and immunological features with type 1 Diabetes [3].
Thus, apart from type 1 and type 2 DM there is another form of diabetes known as LADA. It is also called as Hybrid forms of diabetes, slowly evolving immune mediated diabetes of adults, 1.5DM [4] “Slowly Progressive Insulin-Dependent type 1 Diabetes” (SPIDDM) [5]. LADA remains poorly understood at both a clinical and research level, and usually misdiagnosed as T2DM and treated with OHA [5,6], this might lead to accelerated β-cell destruction leading to insulin-dependency quickly. Early insulinisation helps to preserve residual β-cells [7].
Patients with LADA usually exhibit low stimulated C-peptide indicating reduced β-cell function [8]. C-peptide is a measure of pancreatic β-cell function and it is a surrogate measure of endogenous insulin production [9]. Measurement of C-peptide is preferred over insulin because; it has longer half-life of ≈35 minutes [10]. C-peptide is mostly undetectable in classical T1DM and normal or high in patients with newly diagnosed T2DM, whereas individuals with LADA tend to have low but still detectable C-peptide values at the time of diagnosis [11]. Significant lower levels of C-peptide are seen in patients affected by LADA than in those affected by T2DM [8]. Hence, it can be used to assess the residual β-cell function among LADA population and to differentiate LADA from type 1and T2DM [12].
In addition to low C-peptide levels, presence of diabetes related autoantibodies like GADA Insulin autoantibodies; protein tyrosine phosphatase IA-2 (IA-2A) and islet-specific zinc transporter isoform 8 (ZnT8) autoantibodies, helps to differentiate LADA from other types of DM. But diagnosis of LADA still remains a great challenge to the clinicians because of elevated costs of these autoantibodies.
GADA is the most common antibody present in LADA patients. There are two isoforms of GADA. One isoform has a molecular size of 65kDa and is termed GAD65, while the second one, of 67kDa size, is termed GAD67. Only GAD65 is antigenic and human islets express only GAD65 but not GAD67 [13]. Antibodies to GAD65 are valuable major serological markers for preclinical and overt IDDM [14] and also a major immune marker for the diagnosis of LADA, many studies have confirmed its predictive value for the failure of β-cell function among LADA population [13,15]. GAD antibody in combination with ICA will improve the diagnostic accuracy for LADA.
There are no uniform criteria or guidelines for the selection of LADA patients. Fourlanos S et al., considered below mentioned five-point LADA clinical risk score to find out potential LADA population [16]:
This criterion has 90% sensitivity and 71% specificity for detecting LADA with at least two distinguishing clinical features at diagnosis with negative predictive value of 99% for LADA if the clinical risks score ≤1[16].
Literature search has shown that there is paucity of data regarding the utility and effectiveness of this score in Indian settings. Studies have been done using IDS guidelines for identifying high risk/potential LADA subjects.
According to the Immunology of Diabetes Society (IDS) following three main criteria: (1) adult age of onset (>30 years); (2) presence of any islet cell autoantibody and (3) absence of insulin requirement for at least six months after diagnosis [17] are considered for identification of LADA population.
To date there are no specific guidelines existing for the diagnosis and for the management of LADA. Individuals at increased risk of developing this type of diabetes can often be identified by serological evidence of an autoimmune pathologic process occurring in the pancreatic islets and by genetic markers.
Not much work has been done in India and especially in Karnataka on the prevalence, characteristics, and immunological bases for LADA, hence this study has been carried out.
The aim of study was to screen clinically diagnosed T2DM subjects for potential LADA population based on 5-point LADA clinical risk score; and also to estimate random blood glucose (to confirm them as diabetics), C-peptide, GAD and IC Antibodies in potential LADA subjects and to confirm LADA based on GAD and IC Antibodies.
Materials and Methods
This cross-sectional study was carried out in Rajarajeswari Medical College and Hospital, Bangaluru, Karnataka, India for a period of two years from March 2017 to May 2019. As per the study protocol approved by the Institutional Ethical Committee (dated 08-07-2016), 945 subjects, visiting a medicine OPD diagnosed as T2DM (maximum of five years duration) and age group ranging from 30-50 years, were selected.
Sample size
The sample size was calculated based on the number of T2DM patients visiting the hospital per day.
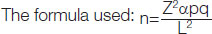
Where, Z α=Standard normal deviate at a desired confidence level (95% or 99%)
P=30%
q=100-p
L= allowable error 5%, 10% or 20% of p
These subjects were screened using 5-point LADA clinical risk scores. Subjects satisfying a minimum of two criteria were considered as potential LADA population and tested for C-Peptide level (to assess residual β cell function) and GAD and IC antibodies to confirm LADA. Type 1 DM Patients, Type 2 DM Patients on Insulin therapy were excluded from the study.
A clinical questionnaire containing age, sex, personal history, family history of diabetes (first degree relatives), height and weight to calculate BMI, duration of diabetes was taken.
Subjects were informed about the study and consent taken. A 5 mL of venous blood samples was collected in Fluoride EDTA, potassium EDTA for the estimation of blood glucose (RBS), HbA1c respectively and Red capped n-Vac tubes containing clot activator for the estimation of C-peptide, GADA and ICA Antibodies. Blood Glucose and HbA1c were estimated on the same day of sample collection. For the estimation of special investigations, C-Peptide, GADA and IC antibodies, serum was separated within one hour and stored at -20°C until further use. (According to Manufacturer guidelines serum can be stored at -20°C for 3 months). GADA and C-Peptide were estimated by ELISA method and IC antibodies were determined by Indirect immunofluorescence method. Blood glucose was estimated by Glucose-oxidase-Peroxidase method in Beckman Coulter AU 480 Autoanalyser and HbA1c by HPLC method using BIORAD-D10 instrument.
Estimation of C-Peptide: C-Peptide levels was estimated for potential LADA population using DIA metra ELISA kit is a solid phase enzyme amplified sensitivity immunoassay performed on a microplate. The method allows the quantitative determination of C-peptide from 0.2-10.0 ng/mL (Sensitivity) [18].
Estimation of GADA: GADA is estimated using TULIP ELISA auto analyser using kits supplied by DLD Diagnostika GMBH [19].
Clinical sensitivity and Specificity: In the DASP 2005 study the kit achieved 98%(n=100) specificity and 92% (n=50) sensitivity.
Expected values: A 99% of healthy blood donor sera give values of less than 5 units per ml in the assay suggesting that values of 5 U/mL or greater can be considered positive for GAD autoantibodies. However, a provisional cut-off for positivity of 10 Units per mL is recommended until individual laboratories have established their own cut-off values using appropriate control sera.
ICA was determined by indirect immunoflorescence test using kits manufactured by PerkinElmer Germany Diagnostics. The level of fluorescence intensity values can range from zero (no specific fluorescence) to five (extremely strong).
Statistical Analysis
The data collected has been analysed using Descriptive Statistics (percentage, mean and Standard deviation) and Statistical Package for the Social Sciences (SPSS) version 20.0. Chi-square and T-test were applied for statistical analysis.
Results
A total of 945 clinically diagnosed Type 2DM patients in the age group of 30-50 years were screened using 5 point LADA clinical risk score to identify potential LADA subjects [Table/Fig-1, 2]. A total of 757 subjects were considered as T2DM because they did not satisfy minimum two LADA clinical risk score. 188 subjects were considered as potential LADA subjects.
Percentage and Gender Distribution of type 2 DM and LADA subjects. Result shows that there is statistically significant male predominance of 62% (n-116) and female were 38% (n=72) with a p-value of <0.001 in LADA population.
| Category of patients (n=945) | Number of patients | Males | Females | Average Age±SD (years) |
|---|
| Count | % | Count | % | Count | % |
|---|
| Type 2 DM | 757 | 80% | 546 | 72% | 211 | 28% | 47±2 |
| LADA population | 188 | 20% | 116 | 62% | 72 | 38% | 42±6 |
Baseline data of type 2 DM and potential LADA.
| Parameters | Type 2 DM (n=757) | Potential LADA (n=188) | p-value |
|---|
| Age (years) | 47±2 | 42±6 | <0.0001 |
| BMI (kg/m2) | 35±2 | 22±3 | <0.0001 |
| HbA1c% | 8.5±0.5 | 8.6±0.3 | 0.0088 |
| % Prevalence | 80% | 20% | <0.00001 |
| Male | 56% | 62% | <0.00001 |
| Female | 44% | 38% | <0.00001 |
| Acute symptoms | 0 | 8% | - |
| Family history | 25% (FH of Type 2 DM) | 6% FH of Autoimmune DM | - |
| Personal history | NIL | 1% | - |
[Table/Fig-3] shows Majority of the LADA subjects (85%) satisfied two criteria of age and BMI. An 8% satisfied three criteria of age, BMI and acute symptoms, 6% satisfied four criteria of Age, BMI, Acute symptoms and family History of Type I DM and only 1 percent satisfied all the five criteria, where the subject had both personal and family history of Hypothyroidism in addition to other criteria.
Distribution of potential LADA subjects on various LADA criteria.
| Potential LADA subjects | n=188 |
|---|
| Subjects satisfying two criteria of LADA clinical Risk score AGE and BMI | 159 (84.6%) |
| Subjects satisfying three criteria of age, BMI and acute symptoms | 15 (7.9%) |
| Subjects satisfying four criteria AGE, BMI and acute symptoms family history of Type I DM | 12 (6.4%) |
| Subjects satisfying five criteria Age, BMI, acute symptoms family history of Type I DM and Personal and family history of Auto immune disease) | 2 (1.0%) |
[Table/Fig-4] shows the levels of GADA titre in potential LADA subjects with Low and normal C Peptide level.
Table depicting the results of C-peptide and GADA titer of LADA subjects.
| C-Peptide | C-peptide <0.7 ng/mL | C-peptide Within normal range (0.7-1.9 ng/mL) |
|---|
| LADA subjects n=188 | 68 (36%) | 120 (64%) |
| GADA titer |
| High (>10 U/mL) | 4 (6 %) | - |
| Low (<10 U/mL) | 3 (4%) | - |
| Negative | 61 (90%) | 120 (100%) |
A 6% (n=4) of potential LADA population had low C-peptide and high GAD titre are confirmed as LADA subjects. Three (4%) subjects had low GADA titer. Remaining 90% (n=61) were antibodies negative. A 100% (n=120) of potential LADA population with normal C-peptide were GADA negative and may be considered as type 2 DM.
Discussion
The LADA, an adult-onset form of autoimmune diabetes, shares clinical, metabolic and immunogenetic characteristics with either type 1 diabetes or type 2 diabetes at variable severity. There is wide variation in the prevalence of LADA globally, as there are no uniform criteria or guidelines for the selection of LADA subjects [20]. An ideal diagnostic approach would aim on obtaining a proper diagnosis and management.
In the present study, we screened of 945 phenotypic type 2 diabetic subjects based on the 5-point LADA clinical risk score identified 20% (n=188) of the population as potential LADA subjects. The remaining 80% (n=757) were considered as T2DM. All of the 188 potential LADA subjects were in the age group of 30-50 years and BMI of less than or equal to 25. An 8% of these potential LADA subjects satisfied three criteria, 6% satisfied four criteria and only 1 percent satisfied all the five criteria [Table/Fig-3].
The average age of a patient plays a very crucial role in the diagnosis and classification of diabetes and also for the treatment regime. The result of the present study showed the average age of presentation of LADA subjects was 42±6 years. According to reported data, one of the important identifying characteristics of LADA is adult age at onset, generally older than 30 years [21]. A retrospective study done in LADA subjects by Fourlanos S et al., has shown a mean age of 46 years [17].
We found the Prevalence of LADA was significantly more in males (62%) than in females (38%) with the (p=0.00001) Babura S et al., in their study found that LADA was more prevalent among males than in females 15 (71%):6 (29%) [22]. This could be because the prevalence of Diabetes is higher in men than in women [23].
LADA subjects are usually lean at diagnosis like type 1 DM patients with BMI ≤25 kg/m2 [24]. BMI was categorised as: normal weight <25 kg/m2, overweight 25-29.9 kg/m2 and obese ≥30 kg/m2 (WHO). The mean BMI of the potential LADA subjects in our study was 23±2 kg/m2. A study by Priyanka P et al., has shown a mean BMI value of 22±0.55 kg/m2 which is slightly lesser compared to our subjects [25]. LADA china study 3 has reported that BMI of their subjects varied based on GADA titer. The BMI of LADA subjects with low GADA titer was higher (25±2.5 kg/m2) compared to LADA subjects with high GADA titre (23.5±2.6 kg/m2) [26].
Acute symptoms of diabetes mellitus were seen only in 8% of our potential LADA subjects. This is in contrast to the retrospective study by Fourlanos S et al., [16,17] who have observed acute symptoms in more than 99% of the LADA population. This difference could be due to inaccurate reporting of acute symptoms by the patients and lack of awareness of family medical history.
Results of studies by Carlsson S et al., demonstrate that FHD is a strong risk factor for LADA with the same magnitude as for type 2 diabetes, and indicates a genetic background [27]. On the contrary, Hjort R et al., in their study showed that the risk of LADA is increased six-fold in individuals with family history of type 1 diabetes compared to 2-fold in those with family history of type 2 diabetes [28]. Impact of family history may be mediated as nonmodifiable risk factors through a heritable reduction of insulin secretion.
In the present study, out of 945 T2DM patients, 757 (80%) subjects were considered phenotypically as type 2 DM and did not satisfy minimum two LADA clinical risk scores. Their mean age in years was 47±2 which is higher compared to potential LADA subjects and was statistically significant (p=0.0001). Mean BMI of T2 DM subject was significantly higher than the potential LADA subjects (35±4 kg/m2 Vs 22±3 kg/m2 (p=0.0001). Fourlanos S et al., in their study observed a significant difference (p=0.0034) in the BMI of Type 2 DM (Median 30.8 kg/m2) compared to LADA subjects (27.9 kg/m2) [16,17]. Reason for high BMI inT2DM- obesity and insulin resistance whereas LADA subjects will be lean at diagnosis hence will have low BMI.
Family History of T2DM was present in 25% of second-degree relatives of T2DM subjects in our study. On the contrary, Priyanka P et al., in their study have reported that 57% of their study subjects had FHD of T2DM [23]. One more study by Mahadeb YP et al., in their study showed that FHD was present in 49% of their study population [29]. FHD is a strong risk factor for the development of DM.
Glycaemic control of our study subject was assessed by measuring HbA1c, with 8.5±0.5% for T2DM and 8.6±0.3 for potential LADA population with the p-value=0.0088. The potential LADA subjects were misdiagnosed as T2DM and were put on OHAs; hence they did not have good Glycaemic control which is reflected as high HBA1C.
Testing for C-peptide is a relatively inexpensive and most sensitive method to assessing residual beta cells in the LADA population; low C-peptide level implies either insulitis or autoimmune destruction of beta cells [30].
In the present study, random C-peptide as a marker of beta cell reserve was tested for all 188 potential LADA subjects. Among them 36% (n=68) had low C peptide levels of less than (0.7 ng/mL) and remaining 64% (n=120) had C-peptide levels within the reference range. The most sensitive marker for diagnosis of LADA is GAD antibodies however screening LADA population by measuring Peptide followed by GAD antibody testing if required will reduce the economic burden of the patients. The rational for using C-peptide as screening tool in the present study.
Many studies by Zampetti S and others (Non-Insulin Requiring Autoimmune Diabetes Study Group) (NIRD study 7) and Action LADA 9 have observed low C-peptide levels in confirmed LADA population compared to the T2DM, indicating insulin resistance in T2DM and residual beta cells in LADA population [7,31].
GAD and IC antibodies belong to a group of diabetes-associated antibodies that destroy the insulin producing pancreatic β-cells through an autoimmune process. GADA is the best single marker for screening and confirming LADA [20] and remarkably stable. GADA along with ICA improves the diagnostic sensitivity of LADA. Diversity in the study design and variation in selecting the patients for antibody testing may lead to a difference in the prevalence of antibody positivity worldwide among LADA.
As the next step to confirm LADA, GAD-Ab and Islet cell antibodies, as markers of autoimmunity, were tested in all 188 potential LADA subjects.
Out of 36% (n=68) who had low C-peptide levels, we observed, one subgroup comprising 4 subjects (6%) had high GADA titre (>10 U/mL) and 3 subjects (4%) had low GADA titres (<10 U/mL). Similarly, Buzzetti R et al., in their study have also observed a bimodal distribution of GADA titer in their LADA subjects [7], the remaining 61 subjects with low C-peptide and 120 subjects with normal C-peptide did not show antibody positivity.
High GADA titer is a strong predictor of autoimmunity and Buzzetti R et al., and others in their 7 years follow-up study found that high GADA titer subjects progress faster for insulinisation [7]. Studies have also shown that low insulin dose will be sufficient if the insulinisation starts early for high GADA subjects [31]. In our study, the subgroup with 4 subjects (6%) with high GADA titers are ideal candidates for early insulinisation. Rosário PW et al., proved that GADA titer should be used to identify LADA and early insulinisation for high GADA subjects will help to preserve residual beta cell function [32].
Low GADA titers probably indicate a more slowly developing β-cell insufficiency reflecting less aggressive form of autoimmunity [33] and it’s an unstable state with limited degree of autoimmunity. Rosário PW et al., in their study showed 20% of the low GADA titer become negative for GADA titer with is 3 years [34]. Liu L et al., in their study, showed that 74.4% of low-GADA titer patients became GADA negative versus only 8.3% of high-GADA titer patients becoming negative for GADA titer [35]. A three year prospective study (LADA china study 3) has demonstrated that the characteristics of LADA subjects with low GADA titer were clinically and metabolically similar to that of T2DM thus implying that GADA titer is associated with heterogeneity in clinical feature and varying degree of beta cell function [26]. In our study, we observed the low GADA tier among 4% of the potential LADA subjects.
Detection of autoantibodies in the plasma helps to diagnose autoimmune diabetes in adults but antibody positivity seems to be an epiphenomenon rather than pathogenic factors in β-cells destruction. Presence of activated mononuclear cells in the pancreas suggesting insulitis which causes β-cell destruction without antibody positivity [30].
In the current study, 61 (90%) of the subjects who had low C-peptide levels, did not show any antibody positivity, they may be positive for other diabetes associated antibodies which we have not tested in our study or they may be in antibody negative insulitis stage.
In the present study only one out of 188 potential LADA subjects exhibited ICA positivity and was GADA positive with high titers. Coexistence of two different antibodies (GADA and ICA) was found in 5.4% of the study population of Jasem MA et al., [36]. It has been reported that combination of antibody testing is the best to confirm LADA. All potential LADA subjects 64% (n=120) who had C-peptide levels within the reference range were negative for GAD antibodies and were also ICA negative. These subjects have been presently classified as T2DM subjects.
Limitation(s)
Random C-peptide estimation has been done in the study to assess the residual beta cell function instead of fasting C-peptide which is a better marker.
Conclusion(s)
Based on 5-point LADA clinical risk score as a screening tool present study, identified 188 (20%) potential LADA subjects out of 945 T2DM subjects. To confirm them as LADA random C-peptide, GAD, IC antibody testing was done, and found that 68 subjects (36%) were found to have low C-peptide. Among them 4 (6%) of the subjects had high GADA titer and 3 subjects (4%) had low GADA titer. Four (6%) subjects who had low C-peptide with high GADA titer are confirmed cases of LADA who may benefit from early insulinisation. High GADA titer indicates severe autoimmunity against beta cells causing destruction of the beta cells, which is reflected as low C-peptide. It was conclude that C-peptide determination can be a cheaper and a cost-effective screening tool for identifying potential LADA population among newly diagnosed T2DM subjects. The more expensive and confirmatory GAD antibody testing should be reserved for those with low C peptide levels.
This is also suggested to include estimation of fasting C-Peptide and diabetic related antibodies to avoid the misdiagnosis of LADA as Type 2 DM.