A Randomised Blinded Comparison of Epidural Infusion of Ropivacaine and Ropivacaine with Fentanyl for PONV and Sedation in Elective Lower Abdominal Oncosurgeries
SS Srihari1, KS Henjarappa2, BH Arathi3, NR Rashmi4, VB Gowda5, Namrata Ranganath6, Jeevanthy P Upadhya7
1 Assistant Professor, Department of Anaesthesiology, Subbaiah Institute of Medical Sciences, Shivamogga, Karnataka, India.
2 Associate Professor, Department of Anaesthesiology and Pain Relief, Kidwai Memorial Institute of Oncology, Bengaluru, Karnataka, India.
3 Associate Professor, Department of Anaesthesiology and Pain Relief, Kidwai Memorial Institute of Oncology, Bengaluru, Karnataka, India.
4 Associate Professor, Department of Anaesthesiology and Pain Relief, Kidwai Memorial Institute of Oncology, Bengaluru, Karnataka, India.
5 Professor, Department of Anaesthesiology and Pain Relief, Kidwai Memorial Institute of Oncology, Bengaluru, Karnataka, India.
6 Professor and Head, Department of Anaesthesiology and Pain Relief, Kidwai Memorial Institute of Oncology, Bengaluru, Karnataka, India.
7 Senior Resident, Department of Obstetrics and Gynaecology, Shimoga Institute of Medical Sciences, Shivamogga, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. NR Rashmi, Associate Professor, Department of Anaesthesiology and Pain Relief, Kidwai Memorial Institute of Oncology, Dr. MH Marigowda Road, Bengaluru-560029, Karnataka, India.
E-mail: itsmedrshree@gmail.com
Introduction
Epidural analgesia is one of the preferred and convenient mode of perioperative management. Neuraxial opioids augment local anaesthetic effect, thus reducing their requirement for analgesia. The addition of fentanyl may cause side-effects like Postoperative Nausea and Vomiting (PONV), sedation which results in patient discomfort, thus effecting postoperative recovery.
Aim
To estimate the incidence, compare the requirement of rescue antiemetics for PONV and Ramsay Sedation Scores within first 24 hours of postoperative period in patients undergoing elective lower abdominal oncological sugeries.
Materials and Methods
The present study was a randomised study which was carried out from September 2016 to May 2018, in 70 patients of American Society of Anaesthesiologist (ASA) I and II, scheduled for elective lower abdominal oncological surgeries. The study population was divided into group R, comprising of patients receiving epidural infusion of 0.2% ropivacaine and group RF with patients receiving epidural infusion of 0.2% ropivacaine with 2 μg/mL fentanyl. The incidence of PONV, rescue antiemetics for PONV and the incidence of sedation using Ramsay sedation score were evaluated in each group and compared. All data was statistically analysed and compared using Student’s t-test, Chi-square. The p-value <0.05 was considered to be statistically significant.
Results
Groups were comparable with regard to demographic data. The incidence of PONV in group R was 37.1% and in group RF was 28.6%. The requirement of rescue antiemetic for PONV were comparable in the study groups. However, this was not statistically significant. Patients in group RF had higher mean Ramsay sedation scores at 0, 1, 2, 4, 6, 12, 18 and 24 hours but the observed difference in both the groups was statistically significant p<0.05 except at 0 and 2 hours which were not statistically significant (p>0.05).
Conclusion
This study concludes that the patients receiving epidural infusion of ropivacaine with fentanyl should be given prophylactic antiemetic to minimise discomfort. Also, these patients when compared to patients receiving epidural infusion of ropivacaine alone require monitoring for sedation during the postoperative period.
Opioid, Ramsay sedation score, Rescue antiemetic
Introduction
The PONV is a frequent complication of surgery, with considerable medical and economic impact, and is associated with high levels of patient discomfort and dissatisfaction [1]. The PONV is a distressing event to many patients, often feared more than the postoperative pain [1,2]. The incidence of PONV is about 25-30% in all patients and up to 80% in patients having multiple high risk factors [3,4].
The PONV, alone or combined with pain, is one of the leading causes for delayed discharge following surgery [5-7]. It can occur during the day after a surgical procedure or beyond [8]. In the first 24 hours postoperatively, the highest incidence of emetic sequelae is observed in patients undergoing gynaecologic oncological surgery after receiving general anaesthesia [9,10]. Abdominal surgery is also a risk factor for PONV, with an increased incidence up to 50% [1]. The overall incidence of PONV after general anaesthesia has been reported to be 37%, although several factors, including sex, age, history of PONV, and opiate administration, influence the risk [11].
The addition of opioids to local anaesthetics as adjuvants to epidural infusion has become increasingly popular as a part of multimodal analgesia in the postoperative period [12]. Ropivacaine is a long-acting regional anaesthetic that is structurally related to bupivacaine. It is a pure S(-)enantiomer, unlike bupivacaine, which is a racemate, developed for the purpose of reducing potential toxicity and improving relative sensory and motor block profile [13]. Fentanyl citrate is a synthetic phenyl piperidine opioid analgesic and chemical congener of the reversed ester of pethidine [14]. Intrathecal opioids are associated with a wide variety of side-effects such as nausea, vomiting, pruritus and sedation [15]. A 5-hydroxy tryptamine 3 (5-HT3) receptor antagonist is used for prevention and treatment of PONV and pruritus. It has good efficacy and minimal side-effects [16].
Neuraxial opioids supplement analgesic effect of local anaesthetics, thereby reducing their requirement. The addition of fentanyl may cause side-effects like PONV, sedation which results in patient discomfort, thus effecting postoperative recovery. In a prospective study it was found that addition of fentanyl to epidural ropivacaine in patients undergoing laparoscopic gynaecological surgeries, increased the incidence of PONV [17].
In a retrospective study, the incidence of PONV was found to be 30% and thus, suggested prospective studies to overcome limitations of their study [18]. In another retrospective study conducted by Ukai T et al., 155 patients who underwent total hip arthroplasty after receiving epidural levobupivacaine or ropivacaine with fentanyl as an adjuvant were evaluated for PONV. They concluded that alternatives to epidural fentanyl should be considered to minimise the incidence of PONV [19].
A randomised double blinded study by Sawhney KY et al., which compared combinations of bupivacaine, ropivacaine with and without fentanyl for postoperative pain relief in lower limb surgeries showed no significant difference of mean Ramsay sedation scores after addition of fentanyl to epidural infusion [20,21].
Considering the limited prospective studies available in literature, this study was designed to estimate the incidence, to compare the requirement of rescue antiemetics for PONV in patients undergoing elective lower abdominal oncological surgeries which was the primary outcome measured. Secondary outcome measured was to compare the incidence of sedation using Ramsay sedation score.
Materials and Methods
This randomised clinical trial was conducted from September 2016 to May 2018 in the Department of Anaesthesiology in Kidwai Cancer Institute, Bengaluru, Karnataka, India. Ethical committee approval was obtained from Institutional Ethics Committee (Ref.no:KMIO/MEC/019/23.March.2017).
Inclusion criteria: Patients of ASA grade I and II of age group between 18-70 years with BMI between 18-30 kg/m2 and who gave informed consent were included in the study.
Exclusion criteria: Patients with coagulopathy, localised infection at the proposed site, known allergy to drugs used, opioid dependence, renal, hepatic or cardiorespiratory impairment or any neurological disorder were excluded from the study.
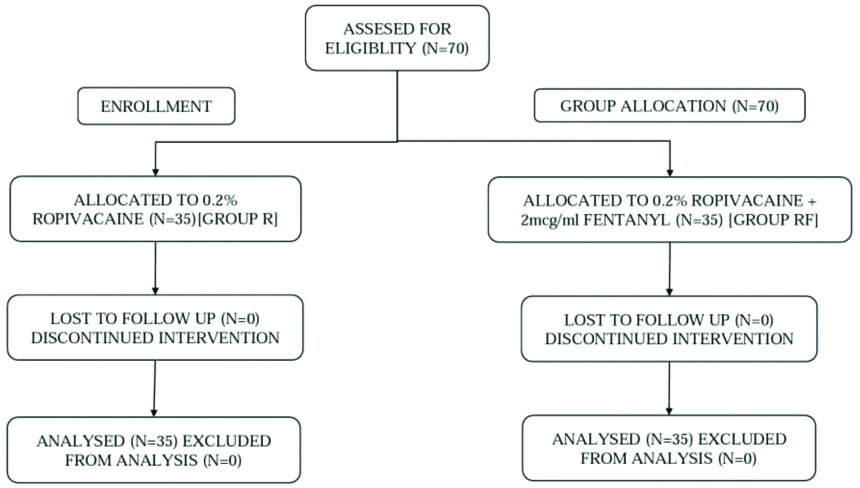
Sample size calculation: The sample size was calculated keeping the power of study at 80%, confidence interval of 95% and an alpha error of 0.05. Accordingly, total sample size calculated was 70. A random number table for 70 patients was divided into two groups (35 each) based on computer generated randomisation table [Table/Fig-1]. The incidence of PONV with rescue antiemetic drug along with Ramsay sedation score were recorded in the first 24 hours of postoperative period.
The two groups were as follows: Group R: Patients who received 0.2% ropivacaine at 5 mL/hour as epidural infusion in postoperative period. Group RF: Patients who received 0.2% ropivacaine with 2 μg/cc fentanyl at 5 mL/hour as epidural infusion in postoperative period.
Study Procedure
A detailed history, comprehensive general and systemic examination were carried out and documented. Epidural catheter was secured at T12-L1/L1-L2 prior to administration of general anaesthesia. General anaesthesia was administered as per institutional protocol. Before surgical incision, the patients were administered epidural 8 mL of either 0.2% ropivacaine or 0.2% ropivacaine with fentanyl 2 μg/mL according to the randomisation table. If the surgery lasted for more than two hours, patients were given additional 4 mL of the study drug epidurally. Upon arrival in Surgical Intensive Care Unit (SICU), patients were started on epidural infusion with study drug group that they belonged to at a rate of 5 mL/hr.
The PONV were recorded as either present or absent by direct observation or by spontaneous complaint from the patient in the first 24 hours of postoperative period. Rescue medications for nausea or vomiting included injection Ondansetron 4 mg Intravenous (IV) immediately. The sedation was documented based on Ramsay sedation score at 0, 1, 2, 4, 6, 12, 18 and 24 hours of postoperative period. Ramsay sedation score was recorded as follows: Anxious or restless or both-1; Cooperative, oriented-2; Responds to verbal commands, drowsy-3; Brisk response to stimulus asleep-4; Sluggish response to stimulus, asleep-5 and No response to stimulus-6.
Statistical Analysis
Descriptive and Inferential statistical analysis was carried out in the present study. Significance was assessed at 5% level of significance. Student’s t-test (two-tailed, independent), Chi-square were used according to the group variables. The p-value <0.05 was considered to be significant. The Statistical software Statistical Package for the Social Sciences (SPSS) 18.0 and R environment version 3.2.2 were used for the data analysis.
Results
The study population comprised of 70 patients posted for elective lower abdominal oncosurgeries and was allocated into two groups of 35 patients each as shown in [Table/Fig-1]. The two groups were similar with regard to demographic characteristics like age, BMI, and ASA physical grade [Table/Fig-2].
Demographic characteristics and operative data.
| Characteristics | Group R | Group RF | p-value |
|---|
| Age (Years) (Mean±SD) | 50.91±10.94 | 47.34±10.72 | 0.172# |
| BMI (kg/m2) (Mean±SD) | 21.86±1.48 | 22.23±2.35 | 0.424# |
| ASA (I,II) | 6,29 | 10,25 | 0.255$ |
BMI: Body mass index; SD: Standard deviation; ASA: American society of anaesthesiologists; #Student’s t-test, $Chi-square
Thirteen patients in Group R and 10 in Group RF had an episode of PONV and were administered rescue antiemetic injection Ondansetron 4 mg IV. The total incidence of PONV in the study population was 33%. However, the difference between the study groups was not statistically significant (p-value=0.445) [Table/Fig-3].
Number of rescue drugs for PONV.
| No. of rescue drugs for PONV | Group R | Group RF | p-value |
|---|
| 0 | 22 (62.9%) | 25 (71.4%) | 0.445 |
| 1 | 13 (37.1%) | 10 (28.6%) |
| Total | 35 (100%) | 35 (100%) |
(Chi-square test used)
The mean Ramsay sedation scores were higher in group RF compared to group R at 0, 1, 2, 4, 6, 12, 18 and 24 hours but the observed difference in both the groups was statistically significant (p<0.05) except at 0 and 2 postoperative hour [Table/Fig-4].
| Posbottomerative duration (hours) | Ramsay sedation score | p-value* |
|---|
| Group R | Group RF | Total |
|---|
| 0 | 2.69±0.72 | 2.94±0.91 | 2.81±0.82 | 0.193 |
| 1 | 2.37±0.81 | 3.06±0.87 | 2.71±0.90 | 0.001 |
| 2 | 2.71±0.86 | 2.86±0.91 | 2.79±0.88 | 0.502 |
| 4 | 2.43±0.70 | 3.29±0.96 | 2.86±0.94 | <0.001 |
| 6 | 2.54±0.82 | 3.20±0.90 | 2.87±0.92 | 0.002 |
| 12 | 2.40±0.65 | 3.54±0.85 | 2.97±0.95 | <0.001 |
| 18 | 2.51±0.74 | 3.23±1.00 | 2.87±0.95 | 0.001 |
| 24 | 2.31±0.47 | 2.97±0.92 | 2.64±0.80 | <0.001 |
*Student’s t-test (two tailed, Independent)
Discussion
Recently, multimodal analgesic techniques, including epidural infusions of local anaesthetic agents with adjuvants like fentanyl, have been used to manage postoperative analgesia in patients undergoing lower abdominal oncological surgeries [22]. Although addition of fentanyl to local anaesthetic provides acceptable postoperative analgesia, they result in undesirable side-effects like PONV and sedation. The incidence of PONV in group R was 37.1% and in group RF was found to be 28.6%. These findings were significantly less compared to study conducted by Apfel CC, which was 50% [1]. The addition of 2 μg/mL fentanyl to 0.2% ropivacaine did not result in significant increase in the incidence of PONV. In this study, patients in the groups R and RF required single dose of rescue antiemetic (Injection Ondansetron) for PONV during the study period. However, this difference was not statistically significant further confirming the findings. These findings may be attributable to lower dose of fentanyl (2 μg/mL) used in this study. These findings differed significantly when compared to study conducted by Kawai K et al., where they used 5 μg/mL fentanyl in addition to 0.2% ropivacaine for gynaecological laparoscopic surgeries. Use of higher concentrations of fentanyl may have resulted in higher incidence of PONV and subsequent requirements of rescue drugs in their study population [17].
Addition of Neuraxial opioids may result in sedation [23]. In this study, mean Ramsay sedation scores were higher in the group RF compared to group R. These findings were similar to randomised, double blinded study conducted by Sawhney KY et al., comparing epidural infusion of bupivacaine, ropivacaine, bupivacaine-fentanyl, ropivacaine-fentanyl for postoperative pain relief in lower limb surgeries which showed no significant difference in sedation scores in their study population [20]. The practice guidelines for the prevention, detection and management of respiratory depression associated with neuraxial opioid administration proposed by the ASA Task Force on neuraxial opioids and the American Society of Regional Anaesthesia and Pain Medicine recommends that the lowest efficacious dose of neuraxial opioids should be administered to minimise the risk of respiratory depression and sedation [23]. Randomised controlled trial reported equivocal findings for respiratory depression, and another trial reported equivocal findings for sedation when higher doses of continuous infusion of epidural fentanyl were compared with lower doses [24,25]. Considering the outcome of this study it is advisable to monitor patients receiving epidural fentanyl for sedation and respiratory depression in the postoperative period.
Limitation(s)
This study was not double blinded. Study was limited only to ASA I and II grade patients undergoing elective surgeries.
Conclusion(s)
This study concludes that prophylactic antiemetic should be administered in patients receiving epidural opioids like fentanyl to minimise patient discomfort. Also, these patients should be monitored for sedation during the postoperative period.
BMI: Body mass index; SD: Standard deviation; ASA: American society of anaesthesiologists; #Student’s t-test, $Chi-square
(Chi-square test used)
*Student’s t-test (two tailed, Independent)
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 13, 2021
Manual Googling: Mar 31, 2021
iThenticate Software: Apr 01, 2021 (25%)
[1]. Apfel CC, Postoperative Nausea and Vomiting. In Miller’s Anaesthesia. 7th edition. Edited by Miller RD, Eriksson LI, Fleisher LA, et al 2009 PhiladelphiaChurchill Livingstone Elsevier:2729-55.10.1016/B978-0-443-06959-8.00086-8 [Google Scholar] [CrossRef]
[2]. Macario A, Weinger M, Carney S, Kim A, Which clinical anaesthesia outcomes are important to avoid? The perspective of patientsAnaesth Analg 1999 89:652-58.10.1213/00000539-199909000-00022 [Google Scholar] [CrossRef]
[3]. Kovac AL, Prevention and treatment of postoperative nausea and vomitingDrugs 2000 59(2):213-43.10.2165/00003495-200059020-0000510730546 [Google Scholar] [CrossRef] [PubMed]
[4]. Apfel CC, Laara E, Koivuranta M, Greim CA, Roewer N, A simplified risk score for predicting postoperative nausea and vomiting: Conclusions from cross-validations between two centersAnaesthesiology 1999 91:693-700.10.1097/00000542-199909000-0002210485781 [Google Scholar] [CrossRef] [PubMed]
[5]. Carroll NV, Miederhoff P, Cox FM, Hirsch JD, Postoperative nausea and vomiting after discharge from outpatient surgery centersAnaesth Analg 1995 80:903-09.10.1213/00000539-199505000-00009 [Google Scholar] [CrossRef]
[6]. Hedayati B, Fear S, Hospital admission after day-case gynaecological laparoscopyBr J Anaesth 1999 83:776-79.10.1093/bja/83.5.77610690142 [Google Scholar] [CrossRef] [PubMed]
[7]. Junger A, Klasen J, Benson M, Sciuk G, Hartmann B, Sticher J, Factors determining length of stay of surgical day-case patientsEur J Anaesthesiol 2001 18:314-21.10.1097/00003643-200105000-0000611350474 [Google Scholar] [CrossRef] [PubMed]
[8]. Odom-Forren J, Jalota L, Moser DK, Lennie TA, Hall LA, Holtman J, Incidence and predictors of post discharge nausea and vomiting in a 7-day populationJ Clin Anaesth 2013 25:551-59.10.1016/j.jclinane.2013.05.00823988801 [Google Scholar] [CrossRef] [PubMed]
[9]. Sniadach MS, Alberts MS, A comparison of the prophylactic antiemetic effect of ondansetron and droperidol on patients undergoing gynaecologic laparoscopyAnaesth Analg 1997 85:797-800.10.1213/00000539-199710000-00015 [Google Scholar] [CrossRef]
[10]. Koivuranta M, Laara E, Snare L, Alahuhta S, A survey of postoperative nausea and vomitingAnaesthesia 1997 52:443-49.10.1111/j.1365-2044.1997.117-az0113.x9165963 [Google Scholar] [CrossRef] [PubMed]
[11]. Apfel CC, Philip BK, Cakmakkaya OS, Shilling A, Shi YY, Leslie JB, Who is at risk for post discharge nausea and vomiting after ambulatory surgery?Anaesthesiology 2012 117:475-86.10.1097/ALN.0b013e318267ef3122846680 [Google Scholar] [CrossRef] [PubMed]
[12]. Angst MS, Ramaswamy B, Riley ET, Stanski DR, Lumbar epidural morphine in humans and supraspinal analgesia to experimental heat painAnaesthesiology 2000 92:312-24.10.1097/00000542-200002000-0001110691216 [Google Scholar] [CrossRef] [PubMed]
[13]. Kuthiala G, Chaudhary G, Ropivacaine: A review of its pharmacology and clinical useIndian J Anaesth 2011 55(2):104-10.10.4103/0019-5049.7987521712863 [Google Scholar] [CrossRef] [PubMed]
[14]. Gourlay GK, Murphy TM, Plummer JL, Kowalski SR, Cherry DA, Cousins MJ, Pharmacokinetics of fentanyl in lumbar epidural and intravenous administrationPain 1989 39:253-59.10.1016/0304-3959(89)90210-8 [Google Scholar] [CrossRef]
[15]. Gozal Y, Shapira SC, Gozal D, Magora F, Bupivacaine wound infiltration in thyroid surgery reduces postoperative pain and opioid demandActa Anaesthesiol Scand 1994 38:813-15.10.1111/j.1399-6576.1994.tb04010.x7887103 [Google Scholar] [CrossRef] [PubMed]
[16]. Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA, Consensus guidelines for the management of postoperative nausea and vomitingAnaesth Analg 2014 118:85-113.10.1213/ANE.000000000000000224356162 [Google Scholar] [CrossRef] [PubMed]
[17]. Kawai K, Sanuki M, Kinoshita H, Postoperative nausea and vomiting caused by epidural infusion following gynaecological laparoscopic surgery: Fentanyl and ropivacaine versus ropivacaine aloneMasui 2004 53(12):1381-85. [Google Scholar]
[18]. Wu HY, Gong CA, Lin SP, Chang KY, Tsou MY, Ting CK, Predicting postoperative vomiting among orthopedic patients receiving patient-controlled epidural analgesia using SVM and LRSci Rep 2016 6:2704110.1038/srep2704127247165 [Google Scholar] [CrossRef] [PubMed]
[19]. Ukai T, Ebihara G, Watanabe M, Opioid administration via epidural catheter is a risk factor for postoperative nausea and vomiting in total hip arthroplasty: A retrospective studyJ Orthop Sci 2018 23(6):973-76.10.1016/j.jos.2018.06.01130431008 [Google Scholar] [CrossRef] [PubMed]
[20]. Sawhney KY, Kundra S, Grewal A, Katyal S, Singh G, Kaur A, A randomised double blinded comparison of epidural infusion of bupivacaine, ropivacaine, bupivacaine-fentanyl, ropivacaine-fentanyl for postoperative pain relief in lower limb surgeriesJ Clin Diagn Res 2015 9(9):UC19-23.10.7860/JCDR/2015/15157.645926500984 [Google Scholar] [CrossRef] [PubMed]
[21]. Ramsay MA, Savege TM, Simpson BR, Goodwin R, Controlled sedation with alphaxalone-alphadoloneBMJ 1974 2:656-59.10.1136/bmj.2.5920.6564835444 [Google Scholar] [CrossRef] [PubMed]
[22]. Seki H, Furumoto K, Sato M, Kagoya A, Hashimoto H, Sekiguchi Y, Effects of epidural anaesthesia on postoperative nausea and vomiting in laparoscopic gynaecological surgery: A randomised controlled trialJ Anaesth 2018 32(4):608-15.10.1007/s00540-018-2525-529936600 [Google Scholar] [CrossRef] [PubMed]
[23]. Practice Guidelines for the Prevention, Detection, and Management of Respiratory Depression Associated with Neuraxial Opioid Administration: An Updated Report by the American Society of Anaesthesiologists Task Force on Neuraxial Opioids and the American Society of Regional Anaesthesia and Pain MedicineAnaesthesiology 2016 124:535-52. [Google Scholar]
[24]. Sjöström S, Bläss J, Postoperative analgesia with epidural bupivacaine and low-dose fentanyl-A comparison of two concentrationsActa Anaesthesiol Scand 1998 42:776-82.10.1111/j.1399-6576.1998.tb05321.x9698952 [Google Scholar] [CrossRef] [PubMed]
[25]. Thomson CA, Becker DR, Messick JM Jr, de Castro MA, Pairolero PC, Trastek VF, Analgesia after thoracotomy: Effects of epidural fentanyl concentration/infusion rateAnaesth Analg 1995 81:973-81.10.1097/00000539-199511000-000147486087 [Google Scholar] [CrossRef] [PubMed]