Breast abscesses are a common complication of mastitis that are common during breast feeding in women of reproductive age group [1]. These lactational breast abscesses constitute the majority of breast abscesses but it can be non-lactational. The non-lactational breast abscesses are usually seen in premenopausal older women who have duct ectasia and are result of periductal mastitis. Smoking, diabetes or obesity are the common risk factors associated with these non-lactational abscesses [2].
It has been observed that 2-3% of lactating women have mastitis and of these 5-11% patients may develop an abscess [3-5]. A breast ultrasound is usually performed to differentiate mastitis from abscess [6]. An abscess is seen as a hypoechoic lesion, which can be well circumscribed, irregular, or ill-defined with possible septa. Needle aspiration showing pus confirms diagnosis and aspirated fluid is sent for microbiological analysis. Presence of leucocytosis may indicate systemic infection.
Various treatment modalities have been described for the management of breast abscess. The standard surgical approach is incision and drainage followed by gauze packing as described by Haagensen CD [7]. Smaller abscesses (<3 cm) can be managed with percutaneous aspiration along with antibiotic therapy [8]. However, for larger abscesses aspiration needs to be repeated and there are chances of recurrence [9]. Ultrasound guided drain placement is an alternative but disadvantages include recurrence and incomplete drainage [10]. Incision and drainage have lower recurrence rates, but it is more invasive than needle aspiration, needs multiple dressings change, may lead to scarring and possible poor cosmetic result. Incision and drainage with primary closure with negative suction drain placement is another option which can be used that has lower recurrence, hospital stay but needs general anaesthesia.
Because of the heterogeneity in management of breast abscess and paucity of data it cannot be stated if open drainage with primary closure and negative suction drain placement is a better option than standard incision and drainage for management of breast abscess. However, some studies such as Surana K et al., indicate that for large breast abscesses incision drainage with primary suturing is better procedure and it reduced patient morbidity and discomfort [11]. Kale A et al., inferred that incision drainage with primary closure over negative suction drain was a better treatment modality for breast abscesses [12]. Hence, there was a need for further studies for definite conclusions.
This randomised trial aimed to compare conventional incision and drainage versus drainage with primary closure over negative suction drain placement.
Materials and Methods
The present study was a randomised controlled study conducted in the Department of General Surgery, Vardhaman Mahavir Medical College and Safdarjung Hospital, New Delhi, India from October 2018 to April 2020. The Ethical clearance was obtained before commencement of the study (S No. IEC/VMMC/SJH/Thesis/October/2018-171).
Inclusion criteria: Women aged more than 15 years with clinical diagnosis of breast abscess and abscess cavity size greater than 3 cm on ultrasonography and gave informed consent were included in the study.
Exclusion criteria: Breast abscess with skin necrosis, burst open abscess, multiple abscesses, recurrent abscess with previous surgical drainage and those with antibioma formation were excluded from the study. Patients with co-morbid conditions such as coagulopathies, Diabetes Mellitus (DM), Human Immunodeficiency Virus (HIV), Hepatitis B and C were also excluded.
Sample size calculation: The sample size calculation was based on mean number of dressings required in two groups. A previous study using a similar protocol [13] indicated that the mean number of dressings in open group would be 14.52. Thus, sample size of 30 patients per group provided with an effect size of 0.84 at 90% power for detecting a 30% difference between the groups at an alpha level of 0.05.
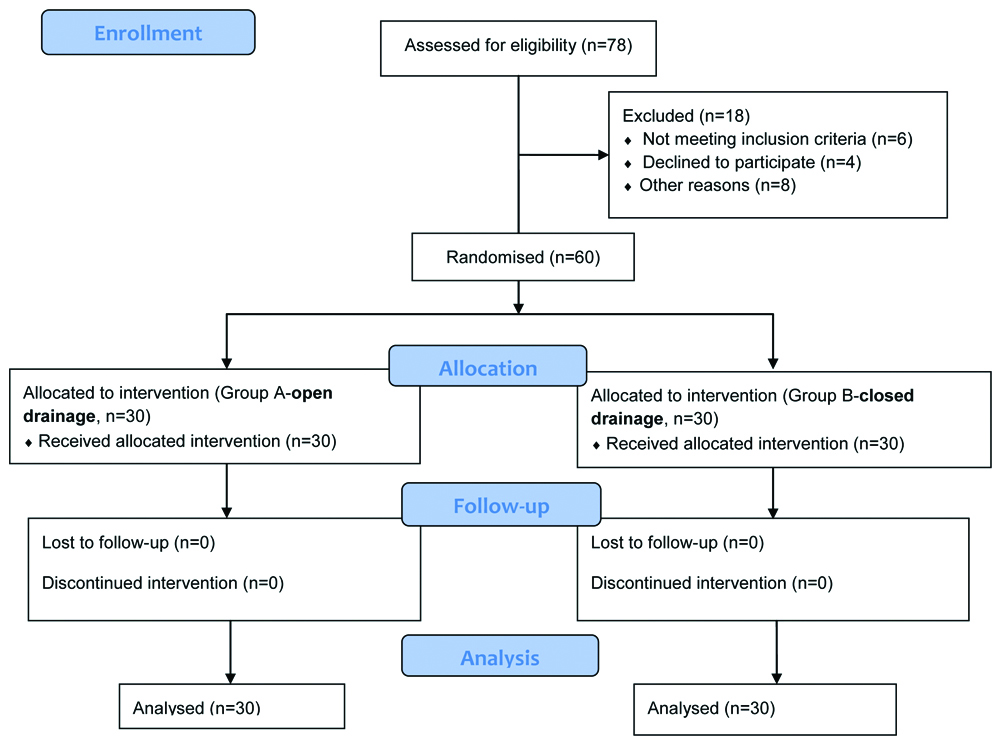
There were 30 patients in group A undergoing open drainage with primary closure and negative suction drain placement (referred subsequently as primary closure group) and 30 patients in group B undergoing open drainage. Randomisation was done by means of closed envelop technique (a method of sealed, numbered envelopes opened in sequence). All surgeries were performed under general anaesthesia. Pre-operatively, all patients were given loading dose of Intravenous (IV) antibiotics (amoxicillin+clavulanic acid 1.2 gm) and were kept nil orally for 5 to 6 hours before surgery [Table/Fig-1].
Surgical Procedure
A stab incision was made over most prominent and dependent part of the abscess cavity. A pair of artery forceps or sinus forceps were thrust into abscess cavity, blades were gradually opened and pus drained. Pus was collected using a sterile swab or a syringe for isolating the type of microorganism for culture and sensitivity. The loculi were broken by swiping a gloved finger for free drainage of all purulent material aided by external pressure, suction or irrigation. Using a curette, the wall of the cavity was scraped as thoroughly as possible to remove unhealthy granulation tissue. The cavity was irrigated with hydrogen peroxide solution followed by copious amount of warm saline.
In the standard incision and drainage method, the abscess cavity was packed with sterile gauze and in the primary closure group, a negative suction drain no. 16 (Romovac) was placed inside the cavity and wound was closed either with interrupted vertical mattress suture or subcuticular sutures using nylon. The wound was inspected 24 to 48 hours after the procedure for evidence of inflammation, pus at stitch line, wound dehiscence etc. Drain output was monitored daily. Postoperatively both groups of patients received Inj. amoxicillin and clavulanic acid 1.2 gm intravenously. Postoperatively analgesics were given based on Visual Analog Scale (VAS) for pain score of 2 or more and analgesics were stopped at VAS less than 2. The duration of analgesic requirement was calculated by noting number of days analgesics were taken.
Dressing was done after first 48 hours in both groups and in primary closure group subsequent dressings were done only if there was any soakage of the dressing and in open drainage group dressing was done daily until healthy granulation tissue was noticed [Table/Fig-2,3].
Operative photograph of primary closure with negative suction drain.

Final appearance after 10 days postoperatively.

Suction drain was removed once drain output ceased and the subcuticular stitches were removed after two weeks. Patients were observed specially for the following clinical outcomes on day 1, day 2, day 4, day 7 and then weekly for six weeks for the following parameters:
Primary outcomes
Number of dressings required- till wound healing in primary closure group and appearance of healthy granulation tissue using photographic wound assessment tool in standard incision and drainage group
Mean duration of analgesia given- analgesics were prescribed based on VAS
Mean duration of hospital stay.
Secondary outcomes
Recurrence-defined as abscess developing again after six weeks.
Statistical Analysis
The data collected were analysed with SPSS version 17.0. Continuous variables were presented as mean±Standard Deviation (SD). Categorical variables were expressed as frequencies and percentages. Nominal categorical data between the groups were compared using Chi-square test or student’s t-test as appropriate. For all statistical tests, a p-value <0.05 were considered significant.
Results
Demographic Characteristics of the Patients
Breast abscesses were more common on right side than the left and occurred more in lactating women than those who were non-lactating. The most common age group was 21-30 years (not shown in table) [Table/Fig-4].
Age, lactation status and side of occurrence.
| Groups | Age (years) | Lactation (%) | Side (%) |
|---|
| Mean±SD | No | Yes | Left | Right |
|---|
| Group A | 27.80±7.89 | 7 (23.3%) | 23 (76.7%) | 11 (36.7%) | 19 (63.3%) |
| Group B | 28.03±8.62 | 7 (23.3%) | 23 (76.7%) | 8 (26.7%) | 22 (73.3%) |
| p-value | 0.913 (student’s t-test) | 1 (Chi-square test) | 0.58 (Chi-square test) |
The primary closure group fared better with less incidence of postoperative pain, reduced hospital stay and less dressings requirement compared to open drainage which were statistically significant.
In the primary closure group the time to drain removal was 3.223±0.97 days. Mean follow-up period was three months for all cases. Recurrent breast abscess was seen in two patients of open drainage group. It occurred at 8 weeks in one patient and 11 weeks after treatment in the other patient. Only one patient in primary closure group presented with recurrence at 10 weeks. All these cases of recurrence were treated with standard incision and drainage [Table/Fig-5].
Comparison of clinical outcome in both groups.
| Groups | Number of dressings | Duration of analgesic requirement | Duration of hospital stay | Recurrence |
|---|
| Mean±SD | Mean±SD | Mean±SD | Yes | No |
|---|
| Group A | 2.33±0.92 | 2.40±0.81 | 3.63±1.16 | 1 (3.3%) | 29 (96.7%) |
| Group B | 12.27±2.57 | 5.43±1.04 | 6.67±1.30 | 2 (6.7%) | 28 (93.3%) |
| p-value | <0.001 (student’s t-test) | <0.001 (student’s t-test) | <0.001 (student’s t-test) | 1 (Chi-square test) |
p-value <0.05 considered significant
Discussion
In the present era, breast abscesses are usually treated by repeated percutaneous aspiration or ultrasound guided drain placement. However, a significant number of patients still require surgical drainage. In this study, the aim was to compare the outcome of breast abscess drainage by standard incision and drainage method versus open drainage followed by primary closure with negative suction drain placement.
It was observed that patients in the primary closure group had a better outcome in terms of healing as it required less dressing compared to the open drainage group. Finding from this study was similar to studies done by Edino ST et al., Ajao OG and Ajao AO; Khanna YK et al., [14-16]. These studies have measured the healing time from time of incision to obliteration of abscess cavity whereas in this study the number of dressings required were used as an indicator to healing. The primarily closed wounds heals by primary intention and it is faster than healing in open wounds which heals by secondary intention. The postoperative pain was evaluated by measuring the duration of analgesic requirement. In the primary closure group, the duration of analgesic required was significantly less compared to standard incision and drainage group. This was similar to the findings observed by Parakh AM and Diwakar MK where the difference of mean duration of analgesia given was 5.7 days in favour of the primary closure group [13]. Raju SRH in their study also reported a better outcome in the primary suturing group as mean duration of postoperative pain was 2.16 days in the primary closure group whereas 4.36 days in the open drainage group [17]. This difference can be ascribed to a smaller number of dressings required in primary closure group and absence of an open wound which is associated with pain and discomfort with longer healing time.
It was also observed that the mean duration of hospital stay was considerably lower in primary closure group. Similar observation was also made in study conducted by Kale A et al., where the duration of hospitalisation was 11.98 days in the primary closure group versus 17.46 days in open drainage group [12]. Same observation was also made in study conducted by Abraham N et al., they found that hospital stay was reduced by 40-60%, thus indicating less morbidity in the primary closure group [18].
Recurrence was also lower in primary closure group though it was not found to be statistically significant. Recurrence rates after incision and drainage, ranges from 13.3-24% [19,20]. Lower recurrence was also observed in study by Kale A et al., where recurrence was three times more in cases of conventional incision and drainage as compared to closed drainage group [12]. Lower recurrence rate observed can be explained by the negative suction drain which ensures removal of all purulent fluid.
Limitation(s)
In this study, the sample size was small and in the open drainage group authors had taken appearance of healthy granulation tissue as an end point rather than the scar formation.
Conclusion(s)
Open drainage followed by primary closure with negative suction drain placement can be considered as a safe and better alternative to the standard incision and drainage as there is less postoperative pain, reduced hospital stay and dressings requirement was also considerably less.
p-value <0.05 considered significant