Cystic Lymphangioma: A Rare Cause of Haemorrhagic Ascites
Swanit Hemant Deshpande1, Vishal Narkhede2, Sunny Agarwal3, Satish Balkrishna Dharap4
1 Senior Registrar, Department of General Surgery, BYL Nair Charitable Hospital and TN Medical College, Mumbai, Maharashtra, India.
2 Assistant Professor, Department of General Surgery, BYL Nair Charitable Hospital and TN Medical College, Mumbai, Maharashtra, India.
3 Associate Professor, Department of General Surgery, BYL Nair Charitable Hospital and TN Medical College, Mumbai, Maharashtra, India.
4 Head, Department of General Surgery, BYL Nair Charitable Hospital and TN Medical College, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Swanit Hemant Deshpande, 1101, Bhavya Supreme, Parel Village, Parel East-400012, Mumbai, Maharashtra, India.
E-mail: Swanitdesh@gmail.com
Lymphangiomas are congenital malformations of the lymphatic system. Multiple intra-abdominal cystic lymphangiomas are rare in adults. Author present a case of a 39-year-old male, presenting with recurrent episodes of haemorrhagic ascites. Laparoscopic biopsy and imaging investigations revealed multiple intra-abdominal cystic lymphangiomas involving the spleen, the liver and the retro-peritoneum. Surgical excision including splenectomy, excision of retroperitoneal and mesenteric lesions was done. The patient has been asymptomatic for 2 years on follow-up.
Ascitic fluid, Excision, Pneumococci, Splencectomy
Case Report
A 39-year-old male was referred from a peripheral district hospital to the General Surgery Outpatient Department of our tertiary care center. The patient had multiple episodes of abdominal distension due to haemorrhagic ascites since the past year. He did not have any associated gastrointestinal symptoms. There was no history of alcoholism or jaundice.
A month prior to this visit he underwent a diagnostic laparoscopy at the peripheral center. A liver biopsy was taken from a cystic lesion in the liver during the diagnostic laparoscopy. The histopathology analysis of the liver biopsy was reported as benign cystic lymphangioma. The surrounding liver parenchyma was normal. The peripheral center referred the case to our tertiary care center for further management. On clinical examination, the patient had pallor. He was vitally stable. The abdomen was distended and presence of ascitic fluid was noted with shifting dullness.
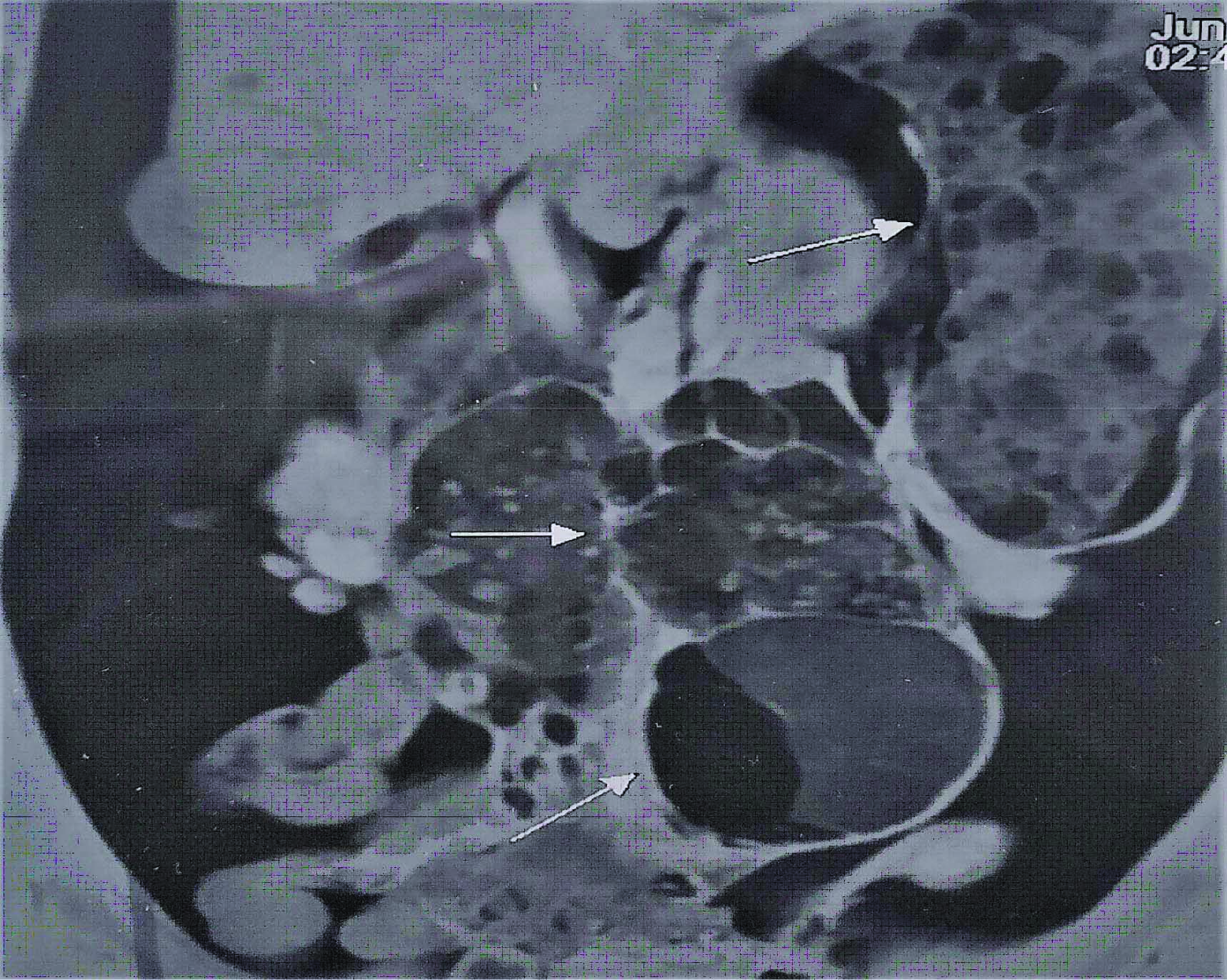
Investigations: Laboratory investigations were normal except for haemoglobin which was 8 mg/dL. The ascitic fluid analysis revealed haemorrhagic exudative fluid. The ascitic fluid analysis was negative for malignant cytology. Imaging investigations included Ultrasonography (USG) and Magnetic Resonance Imaging (MRI). [Table/Fig-1] revealing multiple cystic lesions in the liver, retro-peritoneum and the spleen. The spleen was grossly enlarged in size (15×11×8 cm). Computed Tomography (CT) angiogram was done to look for any active hemorrhagic source. CT angiogram did not reveal any active contrast leak.
MRI Abdomen showing multiple splenic, mesenteric and retro-peritoneal cysts (White Arrows).
Treatment: The patient was posted for elective exploratory laparotomy, excision of multiple cystic lesions and splenectomy. Preoperative vaccination for pneumococci, meningococci and H. influenzae infections was carried out two weeks before surgery.
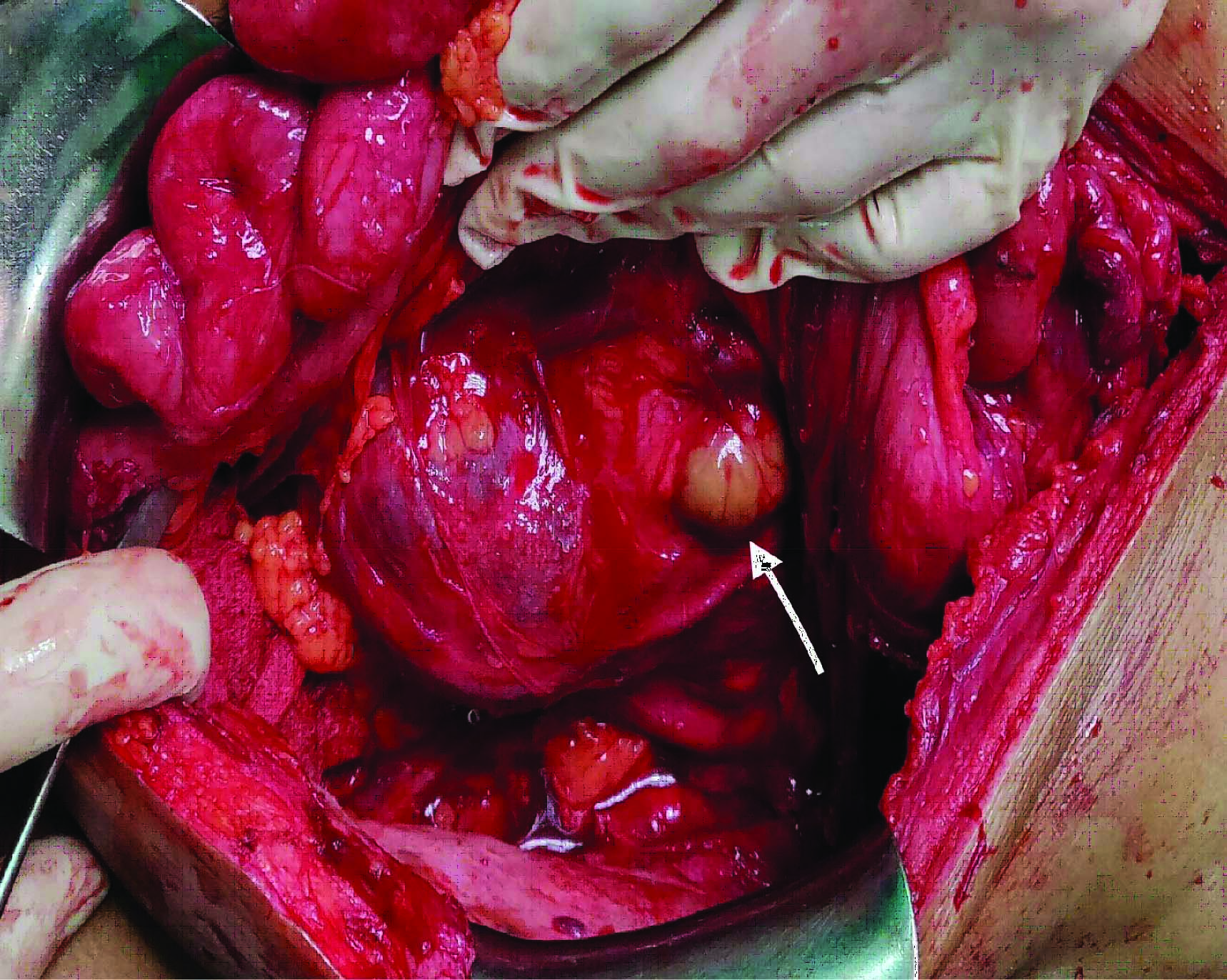
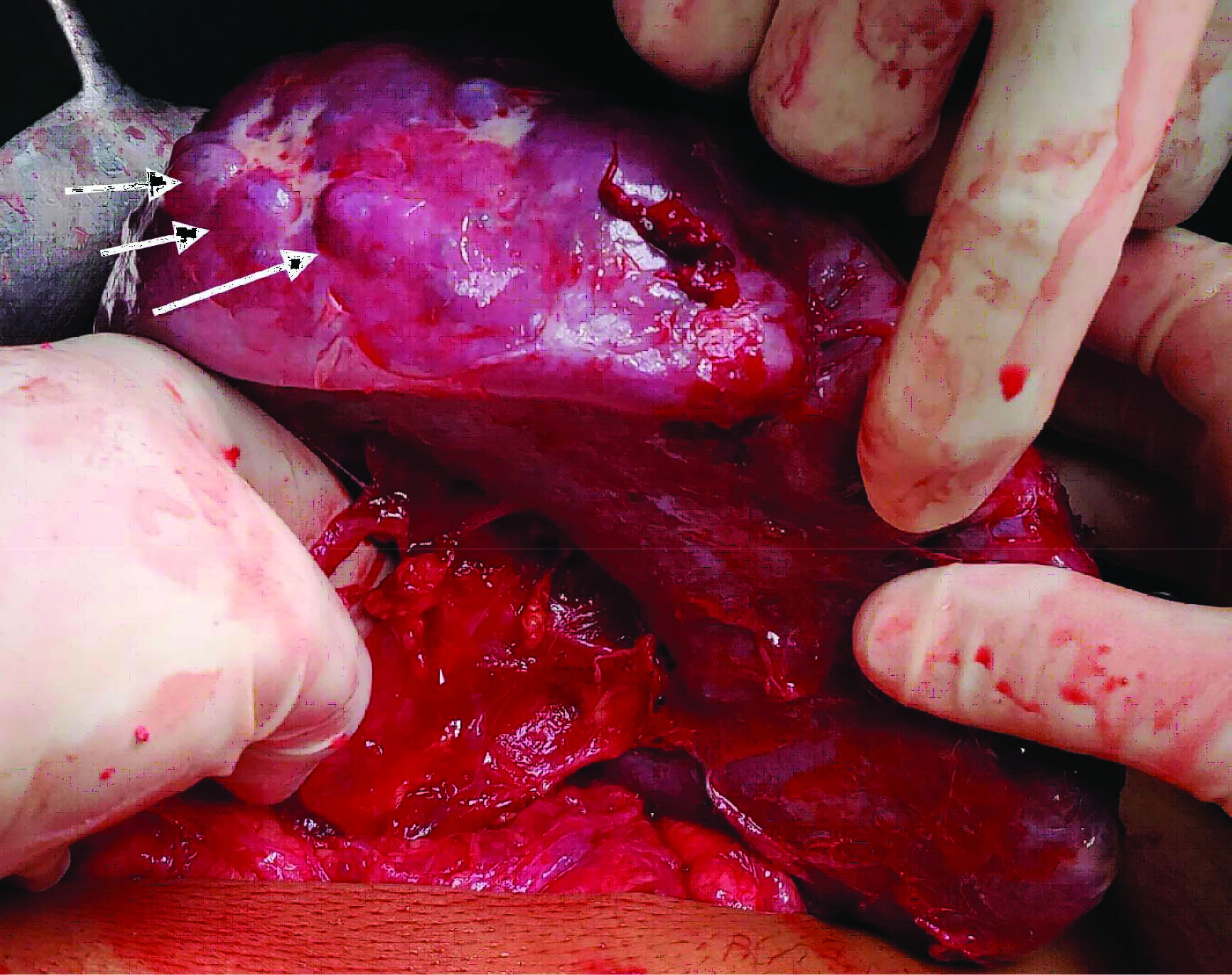
Intraoperatively, after midline abdominal incision, the peritoneal cavity was exposed. Left-sided retroperitoneal cysts with omental adhesions were observed [Table/Fig-2]. The spleen was enlarged with cystic parenchymal lesions [Table/Fig-3]. Splenic hilum was dissected and splenectomy was done. Then the retroperitoneal cyst and mesenteric cyst were excised. The excision was curtailed due to excessive retroperitoneal bleeding secondary to inadvertent injury to the lumbar vein. Haemorrhage was controlled by pressure and local haemostatic agents and over-sewing of the bleeders. The surgery achieved significant debulking of cystic lesions [Table/Fig-4]. Only the lesions in the liver and intact cystic lesions on the right-side of the mesocolon were not removed due to the unexpected significant intraoperative haemorrhage. Abdominal closure was done and intra-peritoneal drain was kept.
Intraoperative picture showing the retro-peritoneal cysts (Arrow).
Intraoperative picture showing multiple splenic parenchymal cysts (Arrow).
Resected specimen of the retro-peritoneal cysts, mesenteric cysts and the spleen.
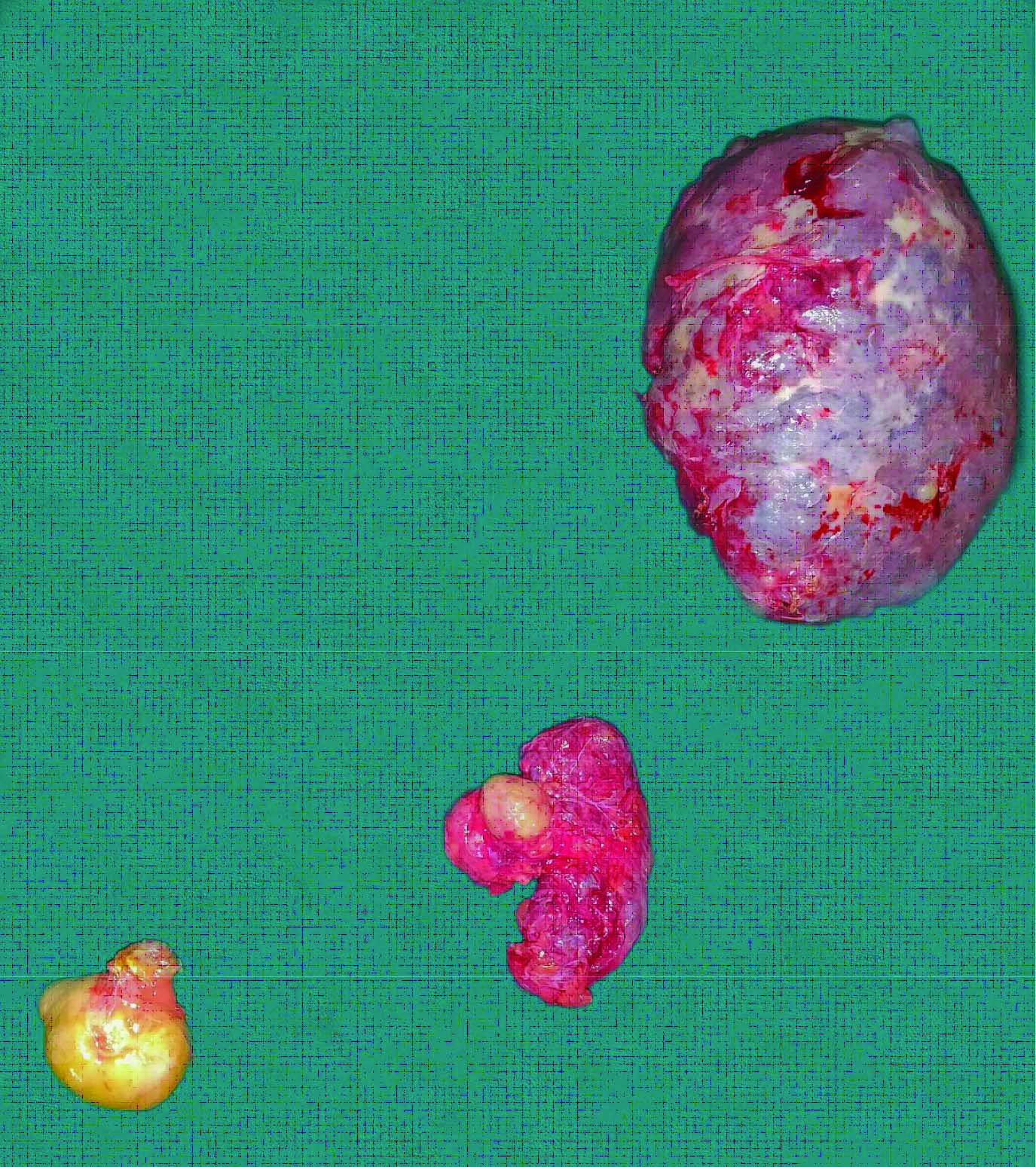
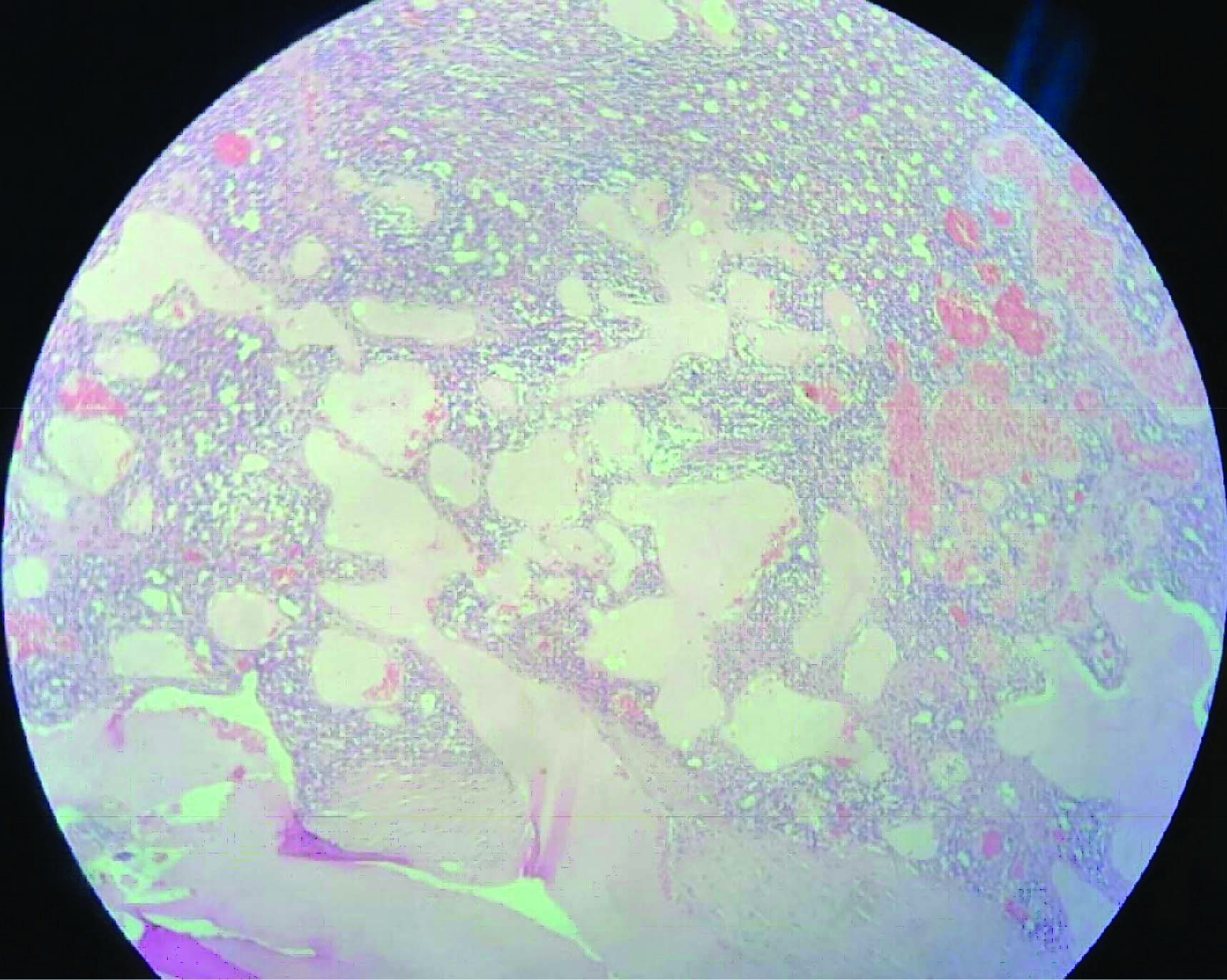
Patient’s had an uneventful recovery. The intra-abdominal drain was removed on the postoperative day 5. Histopathology analysis reported benign cystic lymphangiectasia in the resected specimen of the spleen, mesenteric cyst and retroperitoneal cysts [Table/Fig-5]. The patient was discharged on 10th postoperative day was asked to follow-up after 3 months.
Photograph depicting variable dilated cystic spaces filled with both acellular fluid and red blood cells in Hematoxylin and Eosin stain under 40x magnification.
Outcome and follow-up: The patient was followed-up every three months with clinical examination and USG of the abdomen. The patient has remained asymptomatic for two years. The serial USG abdomen scanning has not reported any intra-abdominal collection.
Discussion
Lymphangiomas are congenital malformations of the lymphatic system. They are usually observed in children and are rarely seen in adults. These benign tumours are generally located in the neck (75%) and the axilla (20%) [1]. Their obstruction or agenesis leads to lymphangiectasia. This failure of normal communication between adjacent lymph ducts leads to cyst formation [1,2]. Lymphangiomas can be isolated or could be diffuse. Diffuse involvement is termed as systemic cystic angiomatosis.
Isolated abdominal multi-visceral involvement in is rarely reported. There have been eight cases reported in the recent literature of isolated abdominal multiple-visceral lymphangiomatosis. [Table/Fig-6] describes the current case in discussion in comparison with the previously reported cases [4-6].
Comparing the reported cases of isolated abdominal multi-visceral lymphangiomatosis [4-6].
| Author, years | Number of patients | Age (in years) and sex | Symptoms | Diagnosis | Abdominal involvement | Treatment | Recurrence |
|---|
| Case series By Allen JG et al., 2006 [6] | 6 | Mean age 50All females | Mostly symptomatic(Gastrointestinal symptoms- constipation most common) | CT scan and biopsy | Multi-visceral | Surgical resection in all | One patient |
| Case report by Rana SS et al., 2016 [4] | 1 | 43/Male | Abdominal distension | CT scan and EUS guided FNAC | Multi-visceral | - | - |
| Case report by Lin RY 2014 [5] | 1 | 38/Female | Intestinal bleeding and protein loosing enteropathy | CT scan and biopsy | Multi-visceral | Surgical resection | - |
| Current Case Report | 1 | 39/Male | Abdominal distension | CT scan and biopsy | Multi-visceral | Surgical resection | - |
CT: Computer tomography; EUS: Endoscopic ultrasound; FNAC: Fine needle aspiration cytology
Usually hepatic lymphangiomas are considered as a subset of multi-visceral abdominal lymphangiomas [3]. Splenic lymphangiomas can be isolated or can be associated with multi-visceral involvement [4,5]. Cystic lymphangiomas in the abdomen are usually asymptomatic. The presentation largely depends upon the location of cysts. Patients with splenic lymphangioma may present with upper left quadrant pain along with fever, nausea, vomiting and weight loss. Haemorrhagic ascites is rarely a presenting symptom.
Diagnosis is largely based on biopsy and histopathological analysis of the cyst. Lymphangiomas can be characterised pathologically by a flat epithelial endothelium and a wall containing alternatively lymphoid tissue, small lymphatic spaces, smooth muscle, and foam cells. Kochman ML et al., suggested that asymptomatic lymphangiomas should most likely be left alone [7]. However, when they cause significant mortality because of their large size, their critical locations and the possibility of becoming secondarily infected, almost all lesions require surgical treatment. In a reported case series of abdominal cystic lymphangiomas in children and adults by Goh BK et al., most of the cases were successfully treated with surgical resection [2].
Symptomatic splenic lymphangiomas usually require splenectomy because of the high risk of rupture, even with minor blunt trauma. If a definitive intraoperative diagnosis is made, complete resection should be attempted, but excision should be as conservative as possible [8]. Alternative forms of treatment such as injection sclerotherapy have been attempted for macro cystic lesions over the limbs and head [9]. Use of injection sclerotherapy for abdominal lymphangiomas has not been reported.
Asymptomatic abdominal lymphangiomas might be left alone and symptomatic abdominal lymphangiomas can be surgically resected. Our patient underwent successful surgical resection and has been completely asymptomatic for 2 years.
Conclusion(s)
Lymphangiomas are congenital malformations of the lymphatic system. Cystic lymphangiomas of the abdomen in an adult presenting with haemorrhagic ascites and anaemia is a rare clinical presentation. High suspicion is needed specially in cases with multi-cystic disease of the abdomen. Successful surgical resection is an effective treatment in symptomatic cases.
CT: Computer tomography; EUS: Endoscopic ultrasound; FNAC: Fine needle aspiration cytology
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 03, 2021
Manual Googling: Jan 20, 2021
iThenticate Software: Mar 22, 2021 (11%)
[1]. Yang F, Chen WX, Splenic lymphangioma that manifested as a solid-cystic mass: A case reportWorld J Gastroenterol 2013 19(5):78110.3748/wjg.v19.i5.78123429434 [Google Scholar] [CrossRef] [PubMed]
[2]. Goh BK, Tan YM, Ong HS, Chui CH, Ooi LL, Chow PK, Intraabdominal and retroperitoneal lymphangiomas in pediatric and adult patientsWorld J Surg 2005 29(7):83710.1007/s00268-005-7794-015951926 [Google Scholar] [CrossRef] [PubMed]
[3]. Stavropoulos M, Vagianos C, Scopa CD, Dragotis C, Androulakis J, Solitary hepatic lymphangioma. A rare benign tumour: A case reportHPB Surg 1994 8:33-36.10.1155/1994/636387993862 [Google Scholar] [CrossRef] [PubMed]
[4]. Rana SS, Chhabra P, Sharma V, Pervez N, Sharma R, Srinivasan R, Disseminated lymphangiomatosis presenting as chylous ascites and diagnosed with endoscopic ultrasoundEndosc Ultrasound 2016 5(3):210-11.10.4103/2303-9027.18397427386481 [Google Scholar] [CrossRef] [PubMed]
[5]. Lin RY, Zou H, Chen TZ, Wu W, Wang JH, Chen XL, Abdominal lymphangiomatosis in a 38-year-old female: Case report and literature reviewWorld J Gastroenterol 2014 20(25):8320-24.10.3748/wjg.v20.i25.832025009412 [Google Scholar] [CrossRef] [PubMed]
[6]. Allen JG, Riall TS, Cameron JL, Askin FB, Hruban RH, Campbell KA, Abdominal lymphangiomas in adultsJ Gastrointest Surg 2006 10(5):746-51.10.1016/j.gassur.2005.10.01516713549 [Google Scholar] [CrossRef] [PubMed]
[7]. Kochman ML, Wiersema MJ, Hawes RH, Canal D, Wiersema L, Preoperative diagnosis of cystic lymphangioma of the colon by endoscopic ultrasoundGastrointest Endosc 1997 45:204-06.10.1016/S0016-5107(97)70253-0 [Google Scholar] [CrossRef]
[8]. Casadei R, Minni F, Selva S, Marrano N, Marrano D, Cystic lymphangioma of the pancreas: Anatomoclinical, diagnostic and therapeutic considerations regarding three personal observations and review of the literatureHepatogastroenterology 2003 50:1681-86. [Google Scholar]
[9]. Jones’ Jones’ Clinical Paediatric Surgery 2015 Seventh edSussex UKWILEY Blackwell:306Part IX: Skin and Soft Tissues [Google Scholar]