Shoulder joint is a highly mobile joint but this mobility comes at the cost of stability. It is prone for rotator cuff injuries and dislocations. Rotator cuff injuries will result in joint pain and restricted mobility. Dislocations will result in labral, bony injuries and shoulder instability. Rotator cuff interval lesions like biceps pulley lesions can lead to biceps tendon instability and glenohumeral microinstability [1-3]. It is necessary to accurately diagnose rotator cuff and labral injuries so that appropriate plan of action for treatment can be taken. MRI can be used to diagnose and describe the extent of rotator cuff tendon and labral injuries and any secondary rotator cuff muscle abnormalities. MRI of shoulder joint gives us the required information in detail without actually subjecting the patients to ionising radiation [1-3].
The rotator cuff tendons consist of supraspinatus, infraspinatus, teres minor and subscapularis tendons. MRI can identify rotator cuff tears and provide information about the rotator cuff tears such as tear dimensions, tear depth or thickness, tendon retraction, and tear shape that can influence treatment selection and help determine the prognosis. The tear extension to adjacent structures, amount of muscle atrophy, size of muscle cross-sectional area, and degree of fatty degeneration have implications for the treatment. Rotator cuff also helps in maintaining the stability of the glenohumeral joint. Tears of the supraspinatus tendon extending into infraspinatus and subscapularis tendons can result in shoulder instability due to loss of balance between anterior and posterior cuff muscles [1,2].
The biceps pulley complex is located within the rotator interval between the anterior border of the supraspinatus tendon and superior border of the subscapularis tendon. The biceps pulley complex consists of Superior Glenohumeral Ligament (SGHL), the Coracohumeral Ligament (CHL), and the distal attachment of the subscapularis tendon. Rotator cuff interval lesions are one of the frequent causes of shoulder pain. It is difficult to clinically and arthroscopically assess the rotator cuff interval. Lesions of the biceps pulley are frequently overlooked or inaccurately assessed on imaging, and if left untreated can result in persistent shoulder pain [4].
On reviewing the literature, authors found many studies that correlated the MRI features of rotator cuff injuries with arthroscopy. However, most of these studies only classified the rotator cuff tears into partial or complete tears and further subclassified the partial tears based on location into articular surface, interstitial or bursal surface tears. To the best of our knowledge, there were very few studies on Indian population grading the severity of tendinosis and partial tendon tears and assessment of the size of the complete tendon tears. There were few studies on Indian population assessing the biceps pulley lesions leading to microinstability and internal impingement. Hence, authors felt the need for a study on Indian population to assess and grade the severity of rotator cuff injuries, assess the rotator cuff interval lesions causing microinstability and internal impingement, evaluate the labral, rotator cuff and bony injuries in shoulder instability.
The purpose of this study was to study the demographic profile of patients presenting with shoulder pain and instability, identify the various rotator cuff injuries causing shoulder pain, identify the rotator cuff interval lesions causing microinstability, identify the various labral and bony pathologies in instability, describe the MRI features of the rotator cuff, rotator cuff interval, labral and bony injuries.
Materials and Methods
This was a cross-sectional study of patients with symptoms of either shoulder pain or instability who underwent MRI evaluation of the shoulder in the Department of Radiodiagnosis, Rajarajeswari Medical College and Hospital, Bengaluru, Karnataka, India, from July 2018 to December 2020. The requirement for informed consent from the study subjects was waived by the Institutional Ethics Committee because this study was a retrospective review of the cases. Institutional Ethics Committee clearance (RRMCH-IEC/07/2021-22) was obtained for the study.
Sample size calculation: The sample size was estimated using the formula: n=Z2P(1-P)/d2; where n is the sample size, Z is the level of confidence (95%), d is precision, and P is the expected prevalence [5]. In the pilot study, that was conducted with a sample size of 10 cases the prevalence of positive cases was 70%. So, using the above formula with a precision (d) of 0.13, the estimated sample size for this study was 48 cases.
The preliminary or initial study population consisted of 70 patients. Sixteen patients with negative MRI, incomplete or suboptimal scan images were excluded. So, the final study population consisted of 54 cases which were more than the estimated sample size. The study population consisted of 54 patients with either shoulder pain or instability who underwent MRI of shoulder.
Inclusion and Exclusion criteria: All patients referred to the Department of Radiodiagnosis for MRI shoulder with history of either shoulder pain or dislocations were included in the study. The exclusion criteria were patients with negative MRI, joint disease like rheumatoid arthritis, glenohumeral degenerative joint disease, previous shoulder surgery and other general contraindications to MRI.
All MRI scans of the shoulder in this study were performed using 1.5 Tesla Siemens Magnetom Avanto (Tim 76x18) MR machine using a flex coil. The patient was placed in supine position with the shoulder and arm placed alongside and parallel to the body. The arm was placed in neutral to mild external rotation position. Internal rotation of the arm was avoided.
Initial three plane localisers were obtained. Axial images were obtained perpendicular to the glenohumeral joint. The axial plane images were used for subsequent coronal oblique and sagittal oblique image planning. Coronal oblique images were obtained parallel to the supraspinatus tendon. Sagittal oblique images were obtained perpendicular to the supraspinatus tendon. Henceforth, the use of the terms coronal and sagittal mean coronal oblique and sagittal oblique respectively. The sequences used in performing the MR scans were T1 sagittal; T2 coronal and axial; Proton Density (PD) Fat Suppressed (FS) sagittal and axial; and Short Tau Inversion Recovery (STIR) coronal. The slice thickness was 3.5 mm. No contrast agent was given.
MR images were read in consensus by the first (7 years of Radiology reporting experience) and second (5 years of Radiology reporting experience) authors at a Siemens syngo.via MR workstation with assistance from the third (final year trainee radiologist) and fourth (final year trainee radiologist) authors.
Evaluation of the Rotator Cuff Tendons
The rotator cuff tendons were primarily assessed in the coronal oblique plane with sagittal oblique and axial planes used for secondary confirmation of pathology. The rotator cuff tendons were considered normal when they demonstrated low signal intensity on STIR, FS PD, T2 and T1 Fast Spin Echo (FSE) sequences without any discontinuity of the fibres. The rotator cuff tendon injuries were classified into tendinosis, partial or partial-thickness tears and full-thickness or complete tears. Tendinosis was diagnosed when the tendon demonstrated high signal intensity (but less than fluid signal intensity) on STIR, FS PD, T2 and T1 FSE sequences without any discontinuity of the fibres. Tendinosis was graded as grade 1 or mild (mild focal increase in tendon signal), grade 2 or moderate (moderate focal increase in tendon signal) or grade 3 or severe (marked generalised increase in tendon signal) [6].
Tears were diagnosed when the tendon demonstrated fluid signal intensity on STIR, FS PD, T2 and T1 FSE sequences with disruption of the fibres. The tears were described based on the type, size and location of the tear, number of tendons involved, the amount of tendon retraction, any muscle atrophy and fatty infiltration of the muscles.
Partial thickness tendon tears were subclassified based on the location of the tear into articular surface, interstitial or intrasubstance, or bursal surface tears. The severity of the partial tears were graded based on the depth of the tendon fibre involvement into small (<3 mm), medium (3-6 mm or <50% thickness) or large (>6 mm or >50% thickness) tears [7].
Complete or full-thickness rotator cuff tears were classified based on the size of the tear in the greatest dimension into small (<1 cm), medium (1 to 3 cm), large (3 to 5 cm) or massive (>5 cm) tears [8]. The amount of tendon retraction was described as near the humeral insertion, at the level of the humeral dome or at the level of the glenoid. The muscle atrophy was assessed on the medial sagittal plane using the tangent sign and graded into mild (even with the line), moderate (concave upper border) or severe (barely visible) atrophy [9]. The amount of fatty infiltration was assessed on T1 sagittal images and graded into minimal (few fatty streaks), mild (some fatty streaks; muscle>fat), moderate (equal amounts of muscle and fat) or advanced (predominance of fat) fatty infiltration [10].
Evaluation of the Rotator Cuff Interval
The rotator cuff interval was primarily assessed in the sagittal oblique and axial planes with coronal oblique plane used for secondary confirmation of pathology. The Long Head of the Biceps Tendon (LHBT) injuries were classified into subluxations, dislocations, tendinosis, partial tears and tenosynovitis. Biceps Labral Complex (BLC) was assessed in the coronal plane and classified into either type 1, 2 or 3. Biceps pulley lesions and anterosuperior impingement were identified in cases with LHBT instability.
Evaluation of Shoulder Instability
Shoulder instability was classified into anterior or posterior instability. Labral injuries in instability were classified as soft tissue bankart, bony bankart, perthes or reverse bankart lesion. Humeral head was assessed at or above the level of the coracoid process for Hill-Sachs or reverse Hill-Sachs lesion. The bones were also assessed for contusions and fractures.
Evaluation of the Labrum
The labrum was primarily assessed in the axial and coronal oblique planes with sagittal oblique plane used for secondary confirmation of pathology. Labral variants were classified into sublabral foramen or hole, sublabral recess, absent anterosuperior labrum and Buford’s complex (absent anterosuperior labrum with thickened middle glenohumeral ligament). Labral tears were identified and classified into different types of Superior Labrum Anterior and Posterior (SLAP) tears [11].
Evaluation of the Bones
Acromion shape was assessed on the sagittal plane and classified into four types: type 1 (flat), type 2 (curved downward), type 3 (hooked downward anteriorly) and type 4 (curved upward) [12,13]. Any obvious impingement of the rotator cuff was noted. Acromioclavicular joint was assessed for degenerative changes and impingement on the musculotendinous unit.
Statistical Analysis
All the data was expressed in numbers and percentages.
Results
As shown in [Table/Fig-1], the study population consisted of 54 patients comprising of 38 males and 16 females. The age of the patients ranged from 20-77 years. Majority of the patients were older than 50 years constituting about 33.33% of the total study population. As shown in [Table/Fig-2], the right shoulder was affected in 33 patients and the left shoulder in 21 patients. As shown in [Table/Fig-3], rotator cuff injury was the most common followed by rotator cuff interval and LHBT pathologies and glenohumeral joint instability.
Age and sex distribution of patients.
| Age (years) | Male | Female | Total | Percentage (%) |
|---|
| <20 | 1 | 0 | 1 | 1.86 |
| 21-30 | 12 | 1 | 13 | 24.07 |
| 31-40 | 7 | 2 | 9 | 16.67 |
| 41-50 | 8 | 5 | 13 | 24.07 |
| >50 | 10 | 8 | 18 | 33.33 |
| Total | 38 (70.37%) | 16 (29.63%) | 54 | 100% |
| Affected shoulder | Number of cases (54 cases) | Percentage (%) |
|---|
| Right | 33 | 61.11 |
| Left | 21 | 38.89 |
Distribution of the pathologies.
| MRI findings | Number of cases (54) | Percentage (%) |
|---|
| Rotator cuff injuries | 46 | 85.18 |
| Rotator cuff interval and LHBT pathologies | 15 | 27.77 |
| Glenohumeral joint instability | 13 | 24.07 |
| Labral (SLAP) tears | 4 | 7.40 |
LHBT: Long head of the biceps tendon; SLAP: Superior labrum anterior and posterior
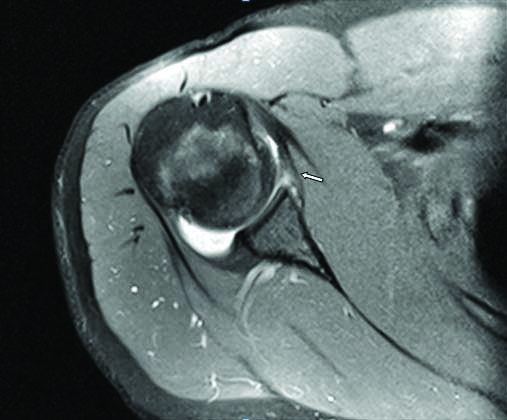
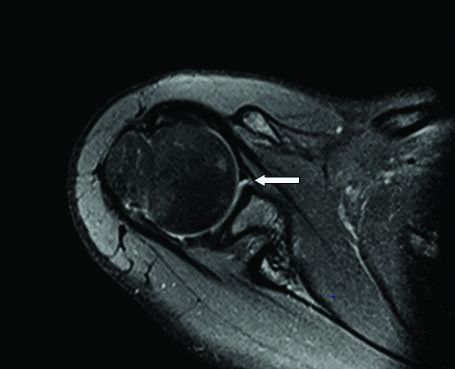
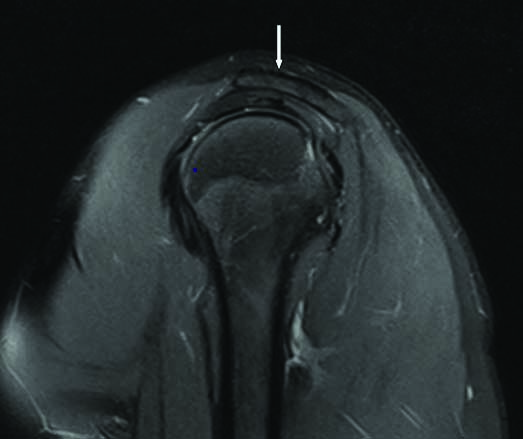
As shown in [Table/Fig-4], the most common type of rotator cuff injury was tendinosis, followed by partial-thickness and full-thickness tendon tears. Supraspinatus tendon [Table/Fig-5] was the most commonly affected tendon followed by subscapularis [Table/Fig-6] and infraspinatus [Table/Fig-7] tendons. Teres minor tendon was normal in all the cases. The most common grade of tendinosis was mild or grade 1 as shown in [Table/Fig-8]. Most of the supraspinatus and infraspinatus tendinosis were associated with subacromial-subdeltoid bursitis.
| Type of tendon injury | Supraspinatus (54 cases) | Infraspinatus (54 cases) | Subscapularis (54 cases) |
|---|
| Tendinosis | 19 (35.18%) | 4 (7.4%) | 14 (25.92%) |
| Partial thickness tear | 13 (24%) | 0 | 5 (9.25%) |
| Full thickness tear | 12 (22.22%) | 1 (3.7%) | 3 (5.55%) |
Note: Teres minor tendon was normal in all 54 cases
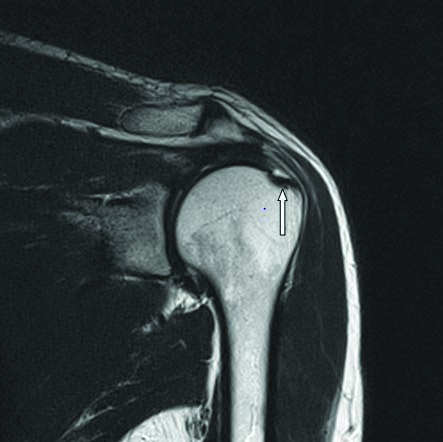
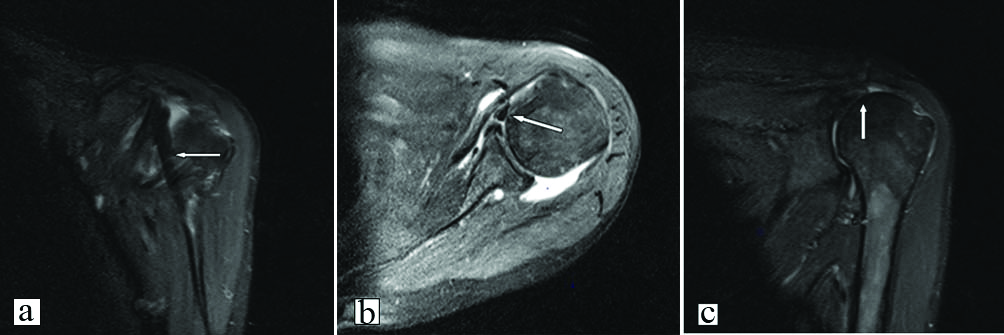
Mild supraspinatus tendinosis: Coronal oblique STIR image demonstrates focal thickening and hyperintensity (arrow) of the supraspinatus tendon.
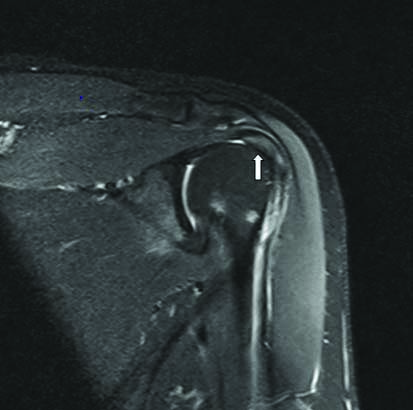
Mild subscapularis tendinosis: Axial FS PD FSE image demonstrates mild subscapularis tendinosis (arrow).
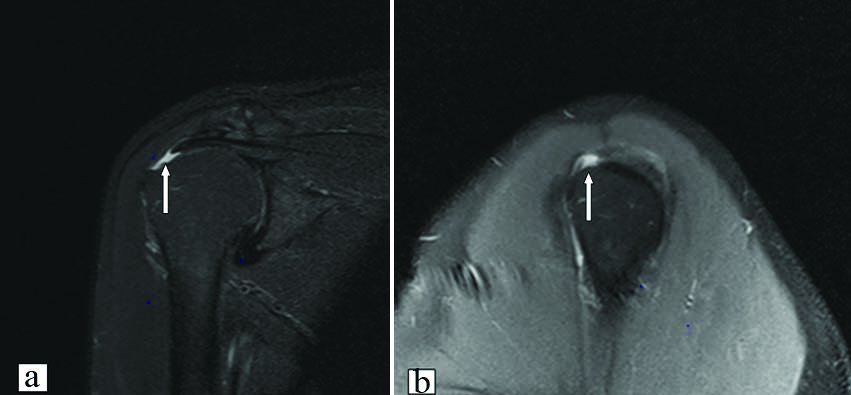
(a-b) Mild infraspinatus tendinosis: Axial and sagittal FS PD FSE images demonstrate mild infraspinatus tendinosis (arrow).
Grading of the tendinosis.
| Tendinosis grade | Supraspinatus (n) | Infraspinatus (n) | Subscapularis (n) | Total (n) |
|---|
| Mild or Grade 1 | 13 | 2 | 8 | 23 |
| Moderate or Grade 2 | 6 | 1 | 5 | 12 |
| Severe or Grade 3 | 0 | 1 | 1 | 2 |
| Total | 19 | 4 | 14 | 37 |
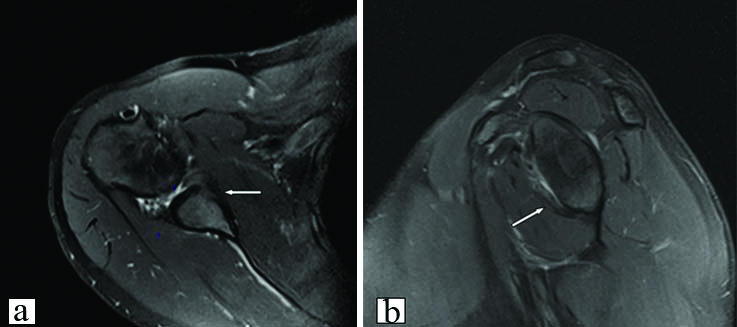
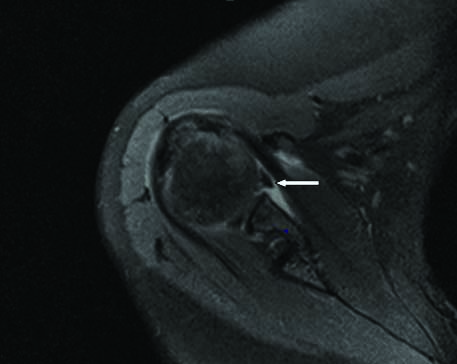
As shown in [Table/Fig-9], small grade partial-thickness articular surface supraspinatus tendon tears [Table/Fig-10] were the most commonly and predominantly affected the anterior fibres (rim-rent tear) of the supraspinatus near the insertion. These were followed by large grade partial-thickness articular surface supraspinatus tendon tears [Table/Fig-11]. There was one case each of intrasubstance and bursal surface supraspinatus tendon tears [Table/Fig-12]. There was no significant retraction of fibres in case of partial tears. There was no case of infraspinatus partial tear.
Location and grading of the partial-thickness tendon tears.
| Tear location | Supraspinatus (n) Grade of the tear | Infraspinatus (n) Grade of the tear | Subscapularis (n) Grade of the tear |
|---|
| Small | Medium | Large | Small | Medium | Large | Small | Medium | Large |
|---|
| Articular surface | 6 | 1 | 4 | 0 | 0 | 0 | 2 | 2 | 0 |
| Interstitial | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Bursal surface | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 8 | 1 | 4 | 0 | 0 | 0 | 3 | 2 | 0 |
Partial articular surface tear- small grade: Coronal STIR image demonstrates a small grade partial-thickness articular surface tear (arrow) of the supraspinatus tendon.
Partial articular surface tear- large grade: Coronal oblique T2 FSE image demonstrates a large grade partial-thickness articular surface tear (arrow) of the posterior fibres of the supraspinatus tendon.
Partial tear- bursal surface: Coronal STIR image demonstrates a small grade partial-thickness bursal surface tear (arrow) of the supraspinatus tendon.

As depicted in [Table/Fig-13], full-thickness tendon tears were most commonly seen in the anterior fibres of the supraspinatus [Table/Fig-14]. Full-thickness tears of the subscapularis tendon most often involved the superior fibres [Table/Fig-15]. There was a case of large full-thickness tear involving both supraspinatus and infraspinatus with moderate atrophy and moderate fatty infiltration of both muscles. There were no massive tears. Tears involving the anterior fibres of supraspinatus and superior fibres of subscapularis tendons were associated with biceps pulley lesions and LHBT instability.
Grading of the full-thickness tendon tears and associated muscle atrophy.
| Muscle atrophy | Supraspinatus (n) Grade of the tear | Infraspinatus (n) Grade of the tear | Subscapularis (n) Grade of the tear |
|---|
| Small | Medium | Large | Small | Medium | Large | Small | Medium | Large |
|---|
| No atrophy | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Mild | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Moderate | 1 | 3 | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| Severe | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Total | 4 | 7 | 1 | 0 | 0 | 1 | 1 | 2 | 0 |
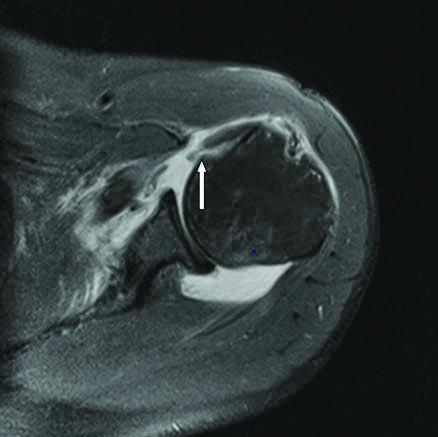
Complete tear- supraspinatus tendon: Coronal STIR and sagittal FS PD FSE images demonstrate a small grade full-thickness tear (arrow) of the anterior fibres of the supraspinatus tendon with retraction of fibres till the humeral insertion.
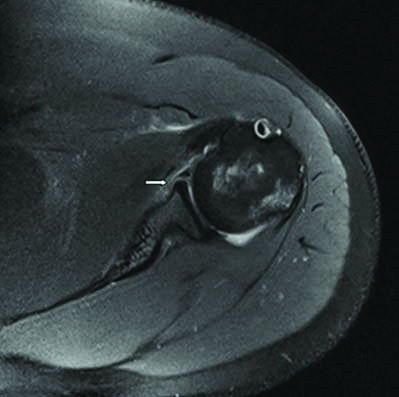
Complete tear- subscapularis tendon: Axial FS PD FSE image demonstrates medium grade full-thickness tear (arrow) of the superior fibres of the subscapularis tendon with retraction of the fibres till the glenoid.
As shown in [Table/Fig-16], the biceps pulley lesions were seen in four cases and medial subluxation of the LHBT in five cases. In one of the cases, there was microinstability resulting in anterosuperior impingement. Anterior instability was the most common type of glenohumeral joint instability as shown in [Table/Fig-17]. Sublabral recess was the most common labral variant. BLC type 1 was the most common type [Table/Fig-18]. The most common type of acromion was type 2 [Table/Fig-19]. Glenohumeral joint effusion was seen in majority of the cases. Additional MRI findings are shown in [Table/Fig-20].
MRI findings of rotator cuff interval and Long Head of the Biceps Tendon (LHBT) pathologies.
| MRI finding | Number of cases |
|---|
| Biceps pulley injuries | 4 |
| Medial subluxation of the LHBT | 5 |
| Medial dislocation of the LHBT | 1 |
| LHBT tendinosis | 2 |
| LHBT partial tears | 2 |
| LHBT tenosynovitis | 10 |
| Anterosuperior impingement | 1 |
Glenohumeral joint instability (13 cases).
| MRI finding | Number of cases |
|---|
| Anterior instability | 12 (92.30%) |
| a) Soft tissue/Classic Bankart | 4 |
| b) Bony or osseous Bankart | 4 |
| c) Perthes lesion | 4 |
| d) Hill-Sachs lesion | 11* |
| Posterior instability | 1 (7.70%) |
| a) Reverse Bankart | 1 |
| b) Reverse Hill-Sachs lesion | 1 |
*One case had only posterolateral humeral head contusion and no Hill-Sachs lesion
Labral variants and Biceps Labral Complex (BLC) types.
| Type of labral variant | Number | Percentage (%) | BLC Type | Number | Percentage (%) |
|---|
| Sublabral foramen or hole | 3 | 5.55 | Type 1 | 48 | 88.89 |
| Sublabral recess | 6 | 11.11 | Type 2 | 6 | 11.11 |
| Buford’s complex | 3 | 5.55 | Type 3 | 0 | 0 |
| Absent anterosuperior labrum | 3 | 5.55 | | | |
| Acromion type | 1 | 2 | 3 | 4 |
|---|
| Number of cases | 13 | 41 | 0 | 0 |
| MRI finding | Number of cases |
|---|
| Subacromial-subdeltoid bursitis | 32 (59.26%) |
| Joint effusion | 30 (55.55%) |
| Fracture | 2 |
| Bone contusion | 2 |
| Acromioclavicular joint arthrosis | 25 (46.29%) |
| Acromioclavicular joint subluxation | 1 |
| Os acromiale | 1 |
| Muscle contusion | 3 |
| Muscle tear | 1 |
| Musculotendinous unit strain | 1 |
Discussion
Demographics of Shoulder Pain and Instability
In this study of 54 patients with shoulder pain and instability, majority was males and most of the patients were older than 50 years. Right shoulder was more commonly affected than the left. Shoulder pain was more commonly seen in the older patients. However, shoulder instability was more commonly seen in the younger patients with the most common age group being 21-30 years and all were males.
The present study findings correlated with the study of Yamamoto A et al., on 1366 shoulders of 683 residents of a Japanese mountain village [14]. In that study, 20.7% of the study population had rotator cuff tears and prevalence increased with age. The tears were most commonly associated with elderly population, males, affected the dominant arm and history of trauma. Milgrom C et al., studied the integrity of the rotator cuff in both dominant and non-dominant shoulders of 90 asymptomatic adults between the age group of 30 to 99 years using ultrasound and found the prevalence of partial- or full-thickness tears increased markedly after 50 years of age [15]. The present study findings of shoulder instability correlated with the study of Tas M et al., on 208 cases (163 male, 45 female) of traumatic shoulder dislocations in Turkey [16]. In that study, males were more commonly affected than females and peak age incidence in males was between 21 to 30 years (96.5% male). Shruthi GT et al., also reported increased incidence of rotator cuff injuries in the fifth and sixth decades and males were more commonly affected [17].
Rotator Cuff Injuries
In the present study, the most common type of rotator cuff injury was tendinosis, followed by partial-thickness and full-thickness tendon tears. Supraspinatus tendon was the most commonly affected tendon followed by subscapularis and infraspinatus tendons. Teres minor tendon was normal in all the cases. The most common grade of tendinosis was mild or grade 1. Small grade partial-thickness articular surface supraspinatus tendon tears were the most common with no significant retraction of fibres in case of partial tears. Full-thickness tendon tears were most commonly seen in the anterior fibres of the supraspinatus. Full-thickness tears of the subscapularis tendon most often involved the superior fibres. Tears involving the anterior fibres of supraspinatus and superior fibres of subscapularis tendons were associated with biceps pulley lesions and LHBT instability.
Shruthi GT et al., and Mall NA et al., reported that supraspinatus tendon injury was the most common rotator cuff injury, followed by subscapularis and infraspinatus injury [17,18]. Shruthi GT et al., and Löhr JF and Uhthoff HK reported that partial tears were commoner than complete tears and partial tears frequently involved the articular surface [17,19]. Itoi E and Tabata S, also reported that partial articular surface tears occur more frequently than partial bursal surface or intrasubstance tears [20]. Resnick D, also reported that partial or incomplete tears to be twice as common as complete or full-thickness tears of the rotator cuff [21].
Kumar G et al., evaluated 100 patients with rotator cuff pathologies and reported that supraspinatus tendon (81%) was most commonly injured followed by subscapularis and infraspinatus tendons [22]. They also reported that partial tears were more common than complete tears and articular surface partial tears were the most common. Sharma G et al., also reported that supraspinatus tendon was the most commonly injured tendon [23]. However in their study, there was marginal increased involvement of the infraspinatus tendon compared to the subscapularis tendon.
The present study findings of rotator cuff injuries correlated with the above studies [Table/Fig-21] [17,22,23].
Comparison of various studies in the Indian population for the prevalence and distribution of rotator cuff injuries [17,22,23].
| Author | Publication year | Supraspinatus | Infraspinatus | Teres minor | Subscapularis |
|---|
| Kumar G et al., [22] | 2017 | 81% | 12% | 0% | 24% |
| Sharma G et al., [23] | 2017 | 100% | 24.4% | 0% | 20% |
| Shruthi GT et al., [17] | 2018 | 97% | 7% | 0% | 17% |
| Present study | 2021 | 81.5% | 9.25% | 0% | 40.74% |
Glenohumeral Instability
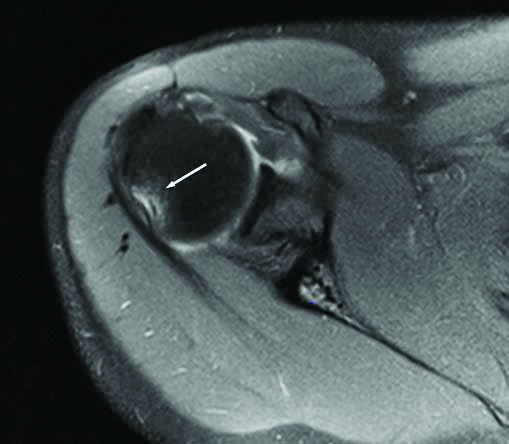
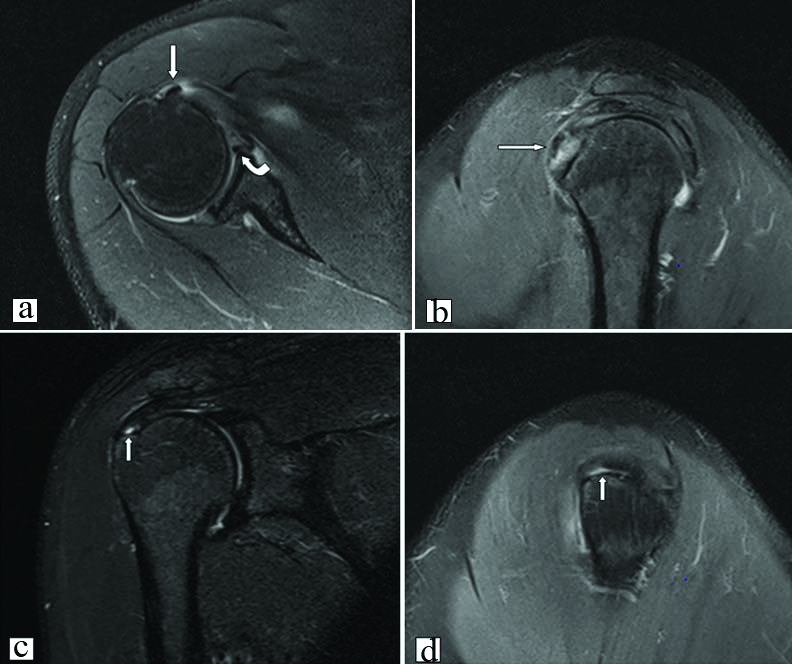
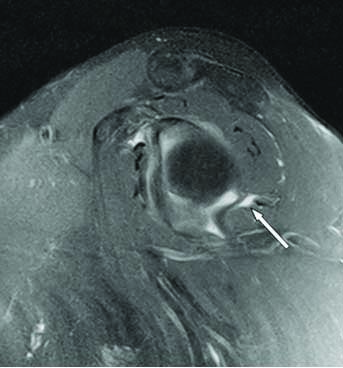
In the present study, there were 13 cases of glenohumeral instability with 12 cases of anterior instability and one case of posterior instability. In the 12 cases of anterior instability, there were four cases each of Perthes [Table/Fig-22], soft tissue Bankart [Table/Fig-23], and bony Bankart [Table/Fig-24] lesions. Eleven cases demonstrated Hill-Sachs lesion [Table/Fig-25] and one case had just contusion in the posterolateral aspect of the humeral head. Four of these 12 cases had associated rotator cuff pathology, three cases of tendinosis and one case of partial tear.
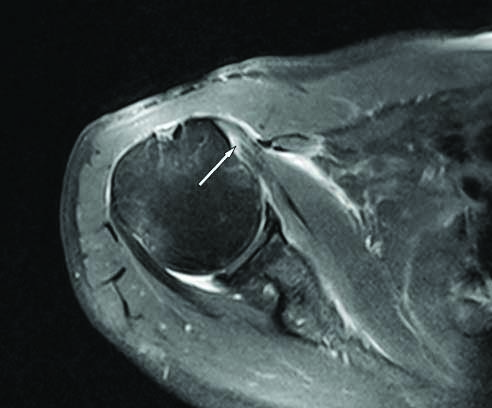
Perthes lesion: Axial FS PD FSE image demonstrates an anteroinferior labral ligamentous avulsion (arrow) with intact but medially stripped periosteum.
Bankart lesion: Axial FS PD FSE image demonstrates an avulsed anteroinferior labrum (arrow) and disruption of the anterior scapular periosteum.
Bony Bankart lesion: Axial and sagittal FS PD FSE images demonstrate an osseous or bony Bankart lesion (arrow).
Hill-Sachs lesion: Axial FS PD FSE image demonstrates a wedge shaped defect (arrow) in the posterolateral aspect of the humeral head at the level of the coracoid process.
Stoller DW et al., Matsen III F et al., and Rafii M also reported that 85% of dislocations are anterior dislocations [1,3,24]. Workman TL et al., reported that Hill-Sachs lesion can be seen in patients with subluxation and single or multiple episodes of dislocation [25]. Richards RD et al., reported the occurrence of posterolateral humeral head contusions, without Hill-Sachs lesion, on MRI [26]. Neviaser RJ et al., found that anterior dislocation of the shoulder may be associated with rotator cuff tears and if these tears are not identified and treated [27], may be the cause of recurrent anterior instability [1].
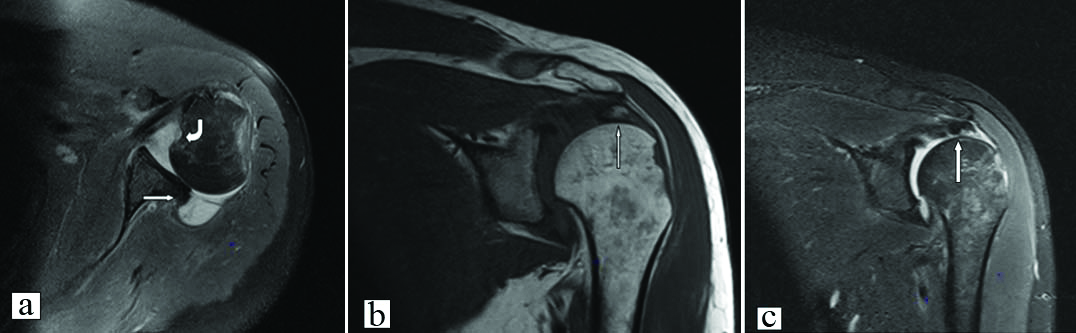
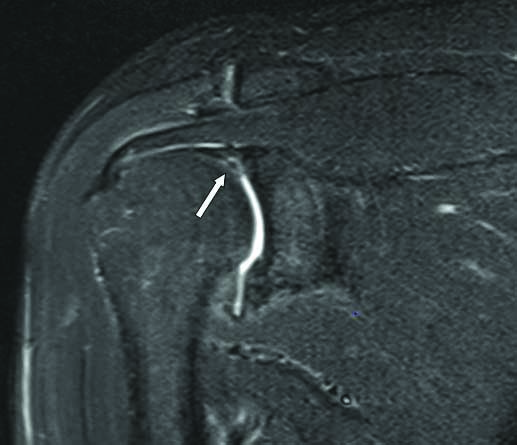
In the present study, there was one case (30-year-old male) of posterior instability which had reverse Hill-Sachs lesion, reverse Bankart [Table/Fig-26a], anterior labral avulsion and associated avulsion fracture of the supraspinatus tendon with retraction upto the humeral dome [Table/Fig-26b,c].
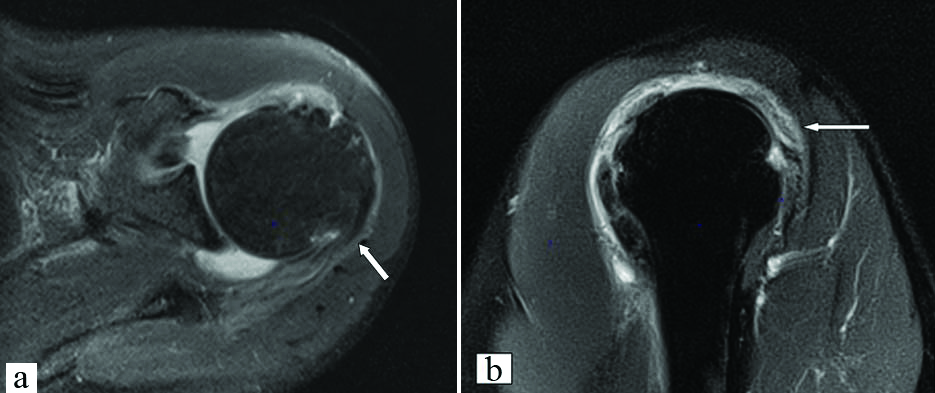
Posterior instability and rotator cuff injury in a 30-year-old male: a: Axial FS PD FSE image demonstrates posterior subluxation of the humeral head with a reverse Hill-Sachs lesion (bent arrow) and reverse Bankart lesion (arrow) and joint effusion. b and c: Coronal T1 and STIR images demonstrate avulsion fracture (arrow) of the supraspinatus tendon with retraction of the fibres till the humeral dome.
Stoller DW et al., reported the incidence of posterior instability between 2 and 4% in patients with shoulder instability [1]. Tung GA and Hou DD, reported increased posterior humeral translation, more extensive posterior labral tear, and avulsion of the posterior labrum and capsule complex in patients with clinical posterior instability [28].
Rotator Cuff Interval and Long Head of the Biceps Tendon (LHBT) Pathologies
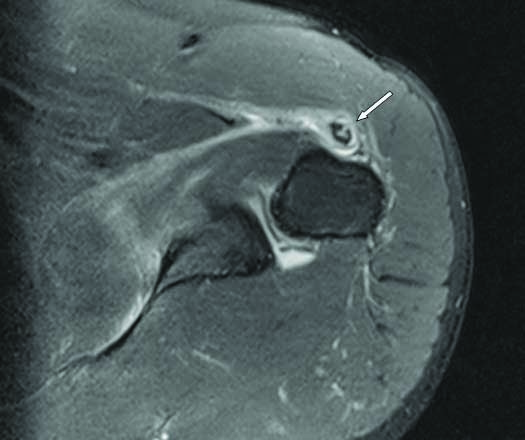
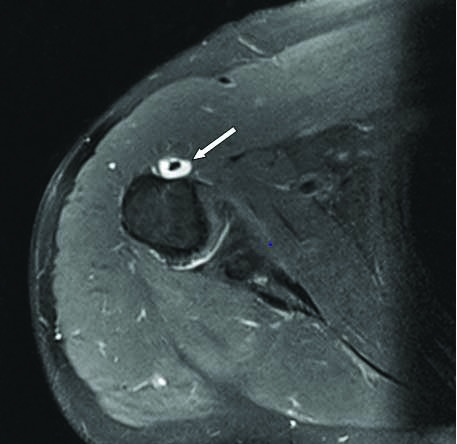
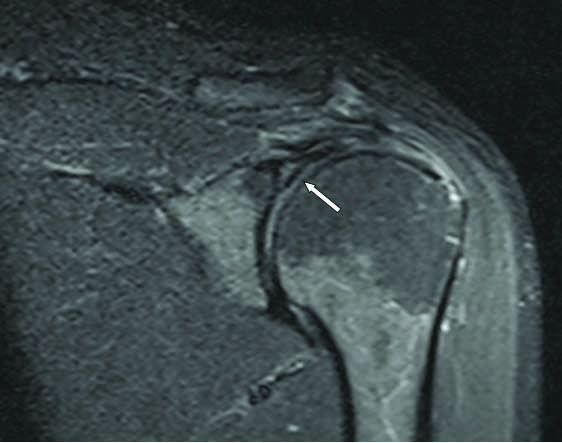
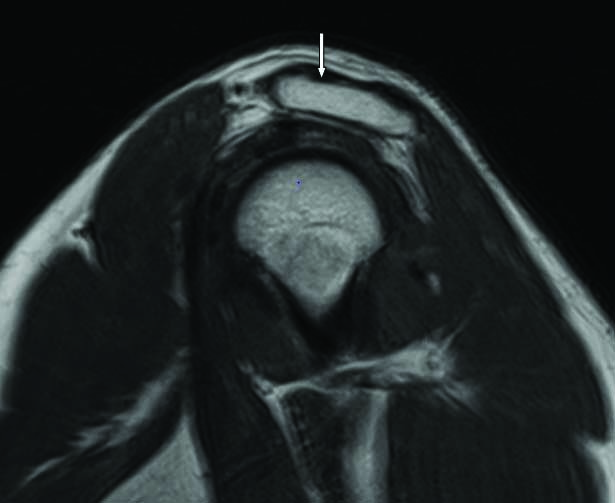
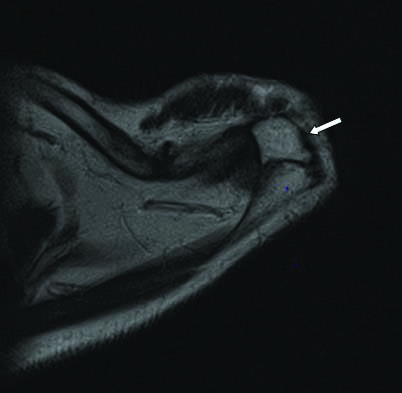
In the present study, there were four cases of biceps pulley lesions. All the four cases had tear of the medial sheath i.e., medial aspect of the CHL (MCHL) and SGHL complex (MCHL-SGHL complex). In two cases, there was additional tear of the lateral aspect of the CHL. Three of these cases resulted in medial subluxation of the LHBT. One case (55-year-old male) had Bennett type 5 biceps instability secondary to medium grade full-thickness tear of the supraspinatus and subscapularis tendons with muscle atrophy and biceps pulley tear which resulted in medial dislocation of the LHBT [Table/Fig-27a-c]. In one of these four cases (47-year-old male with Habermeyer group 3 or 4 biceps pulley lesion), there was tear of the MCHL-SGHL complex, medial subluxation of the LHBT [Table/Fig-28a,b], small grade rim-rent tear of the supraspinatus [Table/Fig-28c,d], medium grade partial-thickness articular surface tear of the superior fibres of the subscapularis [Table/Fig-28a,b], and anterosuperior labral tear [Table/Fig-28a], resulting in microinstability and anterosuperior impingement. There were two cases of mild medial subluxation of the LHBT with no demonstrable biceps pulley pathology. The other LHBT pathologies included partial tears [Table/Fig-29], tendinosis and tenosynovitis [Table/Fig-30].
a-c) Bennett Type 5 biceps instability in a 55-year-old male: a and b: Coronal STIR and axial FS PD FSE images demonstrate medium grade full-thickness tear of the subscapularis tendon with residual attenuated tendon and medial dislocation of the LHBT (arrow). c: Coronal STIR image demonstrates medium grade full-thickness tear (arrow) of the supraspinatus tendon with retraction of the fibres till the humeral dome.
a-d) Microinstability secondary to Habermeyer group 3 or 4 pulley lesion causing anterosuperior impingement in a 47-year-old male: a and b: Axial and sagittal FS PD FSE images demonstrate a medium grade partial-thickness articular surface tear of the superior fibres of the subscapularis tendon, MCHL-SGHL complex tear with medial subluxation of the LHBT (arrow) and anterosuperior labral tear (bent arrow). c and d: Coronal STIR and sagittal FS PD FSE images demonstrate a small grade partial-thickness articular surface tear (arrow) of the supraspinatus tendon.
Partial tear of the LHBT with tenosynovitis: Axial FS PD FSE image demonstrates a partial-thickness tear (arrow) of the LHBT with thickened synovium and fluid within the tendon sheath.
Tenosynovitis of the LHBT: Axial FS PD FSE image demonstrates fluid (arrow) within the LHBT sheath.
Baumann B et al., retrospectively reviewed 1007 arthroscopies and found isolated pulley lesions in 7.1% of cases [29]. Baumann B et al., and Habermeyer P et al., concluded that a biceps pulley lesion leads to instability of the LHBT, which causes partial articular-side tears of the subscapularis and supraspinatus tendons [29,30]. The medially dislocated biceps tendon further reinforces anterior and upward translation of the humeral head, thus resulting in anterosuperior impingement. Godenèche A et al., analysed the relationship between LHBT lesions and subscapularis tears and concluded that in cases of a subscapularis tendon tear associated with a lesion of the SGHL/CHL complex, the LHBT is nearly always unstable and pathologic [31]. Hawi N et al., studied the pulley lesions in rotator cuff tears and concluded the presence of pulley complex lesions in 90.3% of surgically treated rotator cuff lesions, particularly in articular-sided injuries [32]. They also found a significant relationship between the incidence of SLAP lesions and the severity of pulley lesions. Dubrow SA et al., retrospectively reviewed the MRI shoulder of 66 patients who underwent arthroscopy for evaluation of the LHBT and found that MRI identified 29 patients (43.9%) with LHBT lesions (19 partial and 10 complete tears) [33].
Labral Variants and Tears
The most common labral variant was sublabral recess or sulcus [Table/Fig-31], followed by equal incidence of sublabral foramen or hole [Table/Fig-32], absent anterosuperior labrum and Buford complex [Table/Fig-33].
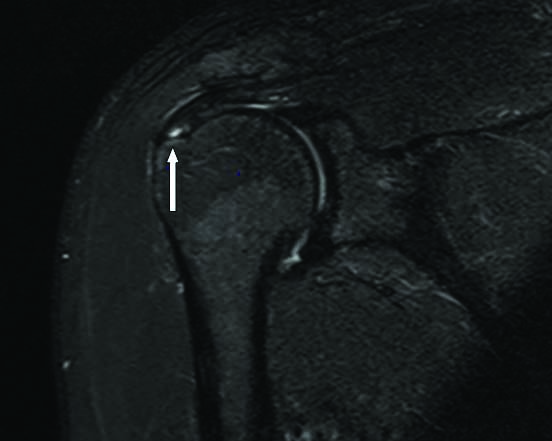
Sublabral sulcus- BLC type 2: Coronal oblique STIR image demonstrates a sublabral sulcus (arrow).

Sublabral foramen: Axial FS PD FSE image demonstrates a sublabral foramen (arrow) in the anterosuperior labrum.
Buford complex: Axial FS PD FSE image demonstrates absence of anterosuperior labrum with a thickened middle glenohumeral ligament (arrow).
Smith DK et al., reported the prevalence of sublabral recess as 73% [34]. Wall MS and O’Brien SJ, and Snyder SJ, reported a normal anterosuperior sublabral foramen or hole in up to 11% of individuals [35,36]. Williams MM and Snyder SJ et al., reviewed 200 shoulder arthroscopies and found a Buford complex in 1.5% and a sublabral foramen in 12% [1,37].
In the present study, there were four cases of labral tears (excluding labral tears in glenohumeral instability)- three were SLAP tears [Table/Fig-34,35] and one was anterosuperior labral tear [Table/Fig-28a]. Out of the 3 cases of SLAP tears, 2 cases were type 1 [Table/Fig-34] and 1 case was type 2 [Table/Fig-35]. The anterosuperior labral tear was associated with anterosuperior impingement as discussed earlier. The reported frequency of types I-IV SLAP lesions has varied in the literature (type I, 9.5-21%; type II, 41-55%; type III, 6-33%; type IV, 3-15%). Type II SLAP lesions are by far the most frequent type identified on arthroscopy, and a similar predominance is expected on MRI [11,38-40].
SLAP tear type 1: Coronal STIR image demonstrates fraying (arrow) of the superior labrum.
SLAP tear type 2: Coronal oblique STIR image demonstrates a tear (arrow) in the superior labrum.
Acromion Variants and Acromioclavicular Joint Pathologies
Type 2 acromion [Table/Fig-36] was seen in 41 patients but it was not associated with any subacromial impingement syndrome. Rest of the cases had type 1 acromion [Table/Fig-37]. Os acromiale [Table/Fig-38] was seen in one case without any degenerative changes across the synchondrosis. There were no cases of type 3 or 4 acromion. Stoller DW et al., reported that type 1 and 2 acromions are more common than type 3 acromion in the general population [1].
Type 2 acromion: Sagittal FS PD FSE image demonstrates a Type 2 acromion (arrow) with a curved inferior surface that parallels the contour of the humeral head.
Type 1 acromion: Sagittal T1 image demonstrates a Type 1 acromion (arrow) with a flat acromial undersurface.
Os acromiale: Axial T2 FSE image demonstrates an Os acromiale (arrow) with no degenerative changes across the synchondrosis.
Acromioclavicular joint arthrosis was seen in 25 cases but was not associated with indentation on the bursal surface of the musculotendinous junction of the supraspinatus. One case of mild superior subluxation of the acromioclavicular joint was noted. Stoller DW et al., reported that true impingement with the undersurface of the acromioclavicular joint does not usually exist because the acromioclavicular joint osteophytes are usually sufficiently medial that they do not compromise the rotator cuff [1].
Additional Findings
Subacromial-subdeltoid bursitis and glenohumeral joint effusion were seen in approximately 50% of the cases. One of the rotator cuff injury cases had associated partial tear of the superior fibres of the teres minor muscle [Table/Fig-39]. Fractures (coracoid process, scapula and ribs), bone contusions and muscle contusions were noted in few of the traumatic shoulder dislocation cases.
Sagittal FS PD FSE image demonstrates a partial tear (arrow) of the superior fibres of the teres minor muscle.
Limitation(s)
Arthrography was not performed in any of the cases which would have helped in better identification of glenohumeral ligament variants and injuries and better characterisation of the SLAP tears. The present study was a descriptive study but arthroscopic correlation would have helped in confirmation and improving the accuracy of the reported findings.
Conclusion(s)
Rotator cuff injuries are the most common cause of shoulder pain and are seen more frequently after the fifth decade. Shoulder instability is most commonly seen in young male adults.
Tendinosis is the most common type of rotator cuff injury. Supraspinatus tendon is the most commonly injured tendon. Anterior instability is the most common type of shoulder instability. Biceps pulley lesions result in long head of biceps tendon instability, microinstability and internal impingement.
MRI can diagnose interstitial or intrasubstance tendon tears which are not visualised on arthroscopy. MRI description of tendon and labral tears, tendon retraction and muscle atrophy can guide the orthopaedician during arthroscopy and in treatment planning.
LHBT: Long head of the biceps tendon; SLAP: Superior labrum anterior and posterior
Note: Teres minor tendon was normal in all 54 cases
*One case had only posterolateral humeral head contusion and no Hill-Sachs lesion