For successful placement of dental implants, the clinician needs adequate bone in three dimensions around endo-osseous implants to enhance Bone Implant Contact (BIC) area and primary stability. The absence of optimum bone calls for complex procedures such as sinus lifts, bone augmentations using grafts that aggravates patient morbidity, dramatically higher costs and limited patient satisfaction. To overcome disadvantages of grafting, graft-less solution used in combination or alone, such as tilted implants, use of long, narrow implants, bicortical implants, all-on-4 techniques have enhanced patient acceptance and clinical ease. All-on-4 protocol is one such combination treatment concept whose success has been demonstrated mainly in ideal/moderate osseous structures. Further, it accommodates 10-12 teeth per arch, mostly without second molars compromising chewing efficiency and creating cantilevers especially in rehabilitations opposing complete set of natural teeth. Additionally, optimal number of implants required to support full arch prosthesis remains unclear. Therefore, to circumvent the limitations of all-on-4 technique, 6 long (16-25 mm) and tilted implants have been used to restore 14 teeth in severely atrophic maxillary arch of a healthy 75-year-old female in the following case report. Tall implants engage basal cortical bone aiding in immediate fixation and increase in surface area of osseo-integration. All implants were placed using minimally invasive flapless technique and immediately loaded within 3 days with a screw-retained multiunit Direct Metal Laser Sintering (DMLS) prosthesis. The pterygoid cortex engagement of distal implants does not have any deleterious biomechanical effect eliminating the distal cantilever.
Bicortical, Cantilevers, Corticalisation, One-stage surgery, Osseodensification, Subcrestal, Surgical template
Case Report
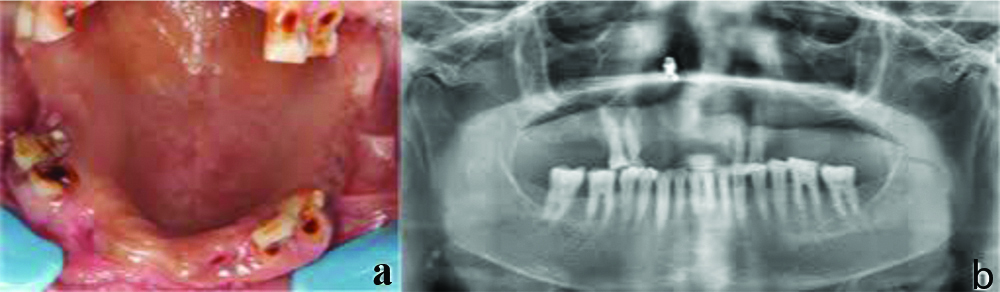
A healthy 75-year-old female reported to a private clinic with chief-complaint of difficulty in chewing food. The patient reported with history of extraction of three teeth due to mobility one month ago. She did not have any significant medical history or habits. On oral examination, #13, 16, 21 healing extraction sockets and #14, 15, 23, 24 severely attrited terminal dentition was present. All mandibular teeth were present [Table/Fig-1a]. Patient was subjected to panoramic radiograph (Genoray Papaya, Delhi, India) [Table/Fig-1b] and cone-beam computerised tomography scan (Carestream, India) that demonstrated an atrophic posterior maxillary ridge (bone height 6.0 mm, width 4.0 mm), [Table/Fig-2a] Anterior maxilla exhibited reduced bone volume with labial undercuts and irregular crests [Table/Fig-2b]. Bone quality assessed was type 3 in posterior maxilla and posterior part of premaxilla and type 2 in anterior part of premaxilla.
a) Preoperative maxillary picture showing terminal dentition; b) Preoperative OPG.
a) Maxillary ridge dimensions at #24,25,26; b) Maxillary labial undercuts at #11,12. c) Stereolithographic maxillary model of patient with surgical stent.
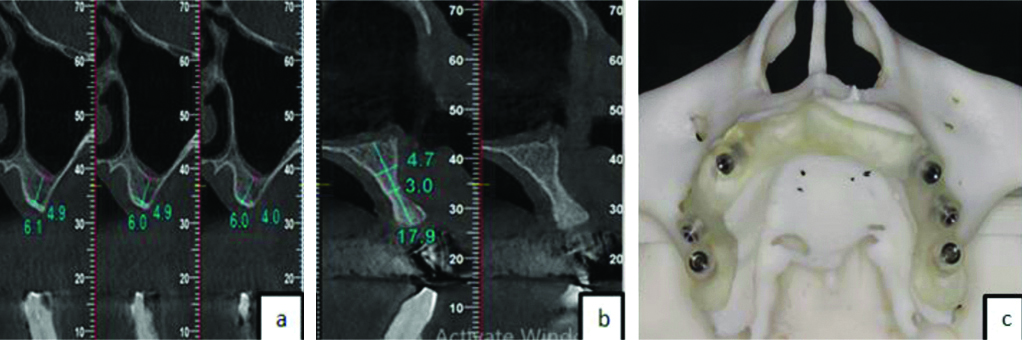
Patient was explained in detail about treatment options like implant/tooth supported removable and implant supported fixed prostheses. Patient opted for implant supported fixed prosthesis. Considering the age of patient, it was important to provide patient centric minimally invasive treatment with immediate function. All treatments encompassing morbid sinus grafting and bone augmentations that delayed function were ruled out. Owing to poor bone density and volume in posterior maxilla, higher functional forces in molar region and presence of all mandibular teeth, it was prudent to have longer tilted implants that engage basal cortical bone for purposes of primary stability and immediate function and provide more chewing surfaces in occlusion without any cantilever. All the above factors were considered and Tall and Tilted Pin Hole Placement Immediate Loading (TTPHIL) protocol was recommended [1,2]. After obtaining signed consent for treatment, oral prophylaxis was performed followed by maxillary and mandibular diagnostic alginate (Algitex, DPI, Karnataka, India) impressions. Cone Beam Computed Tomography (CBCT) data was used to make stereolithographic models and surgical stents [Table/Fig-2c].
One hour prior to surgery, tab. amoxicillin 1 g was given orally and was followed-up with 500 mg for 3 times/daily for next 3 days. All implants (Bioline I, Bioline Dental GmbH & Co. KG, Berlin, Germany) were placed under 2% lignocaine hydrochloride with adrenaline 1:200000 (Lignox 2%). Atraumatic extraction of #14,#15,#23,#24 were done followed by immediate implantation in same appointment. Surgical template with metal sleeves was placed against alveolar ridge tissue anchored at midline [Table/Fig-3a]. Anterior fixture was placed anterior to anterior wall of maxillary sinus from distal to mesial direction towards nasal cortex in first quadrant. Using surgical guide, a pilot drill of 1.2 mm was positioned through mucosa into alveolar bone upto 6 mm depth [Table/Fig-3b]. Radiovisiographic Image (RVG) (Carestream, Kodak, India) was taken to confirm 300 tilt to occlusal plane [Table/Fig-3c].
a) Surgical STL stent; b) anterior implant 300 drill direction; c) Intraoral Periapical (IOPA) showing pilot drill direction.
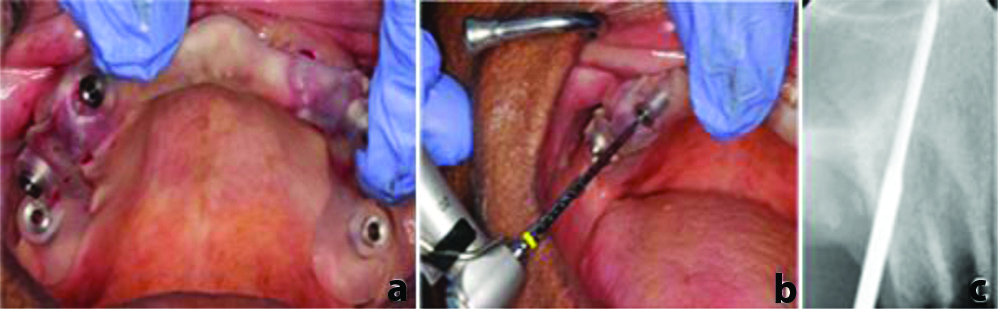
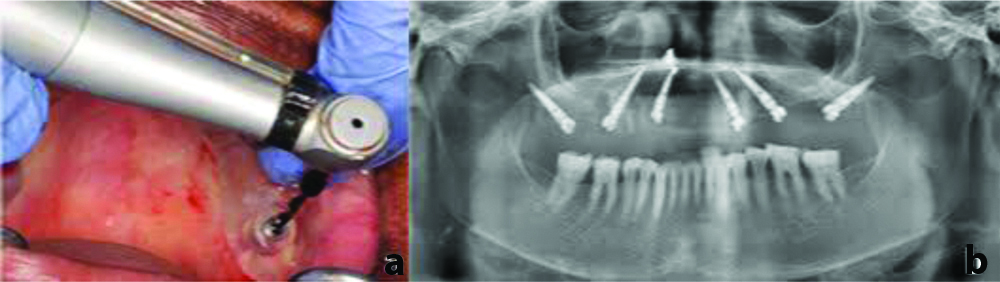
Then, 1.4 mm diameter single drill was used to drill through template at low speed of 400-600 rpm for proprioception of nasal cortex engagement. A 3.5×18 mm tapered implant mounted on implant driver was driven into drilled course. A 40Ncm torque and reverse torqueing forces were obtained using torque rachet. A confirmative RVG was taken. The second implant (3.5×18 mm) was placed using same protocol at premolar site parallel to first implant in distal to mesial direction at 450 to occlusal plane. All implants were placed subcrestally. Following palpation of hamular notch, pterygoid implant (3.5×20 mm) drill was directed mesio-distally and bucco-palatally about 5mm laterally at approximately 450 to occlusal plane. The drill was stopped after engaging pterygoid cortex [Table/Fig-4a]. A verification RVG with depth guage was taken; implant (3.5×18 mm) was driven slowly until subcrestal placement was achieved. Same approach was followed for second quadrant. A 300,450,450 multiunit abutments were placed in anterio-posterior sequence to achieve implant parallelism [Table/Fig-4b].
a) Pterygoid implant 45° drill direction; b) OPG showing 6 tilted implants with multiunit abutments.
Provisional fixed prosthesis was delivered until permanent prosthesis was fixed. Impression copings (Bioline-I, Bioline Dental GmbH & Co.KG, Berlin, Germany) with appropriate diameters were placed on multiunit abutments and splinted with pattern-resin (GC pattern resin, GC dental, India) to transfer intraoral spatial relationship of nonparallel implants to working cast accurately and achieve prosthesis passive fit [Table/Fig-5a]. Implant level impressions using the open tray technique were made [Table/Fig-5b].
a) Maxillary open tray impression with putty and light body material; b) Splinted impression copings.
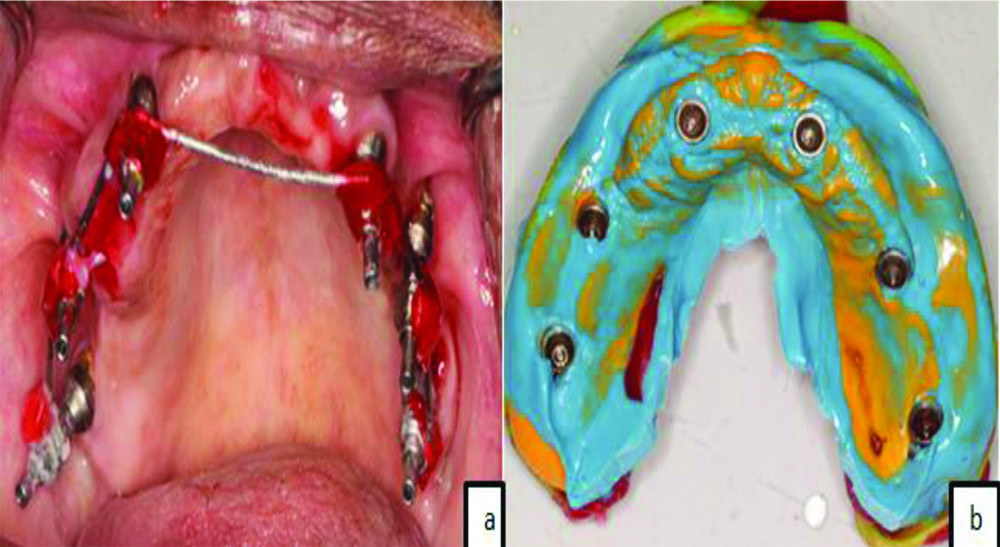
Two stage impression techniques using putty and light body (GC Flexseed, GC dental, India) was followed. Titanium based metal cylinders (Ti-bases) were screwed onto multiunit abutments and customised to interocclusal height. Aluwax (Maarc perfect bite, Hyvincare, India) was engaged around metal bases and interocclusal bite recorded [Table/Fig-6a]. Implant analogs were attached to open tray copings and soft tissue was reproduced employing soft tissue moulage material (Kerr, Orange, CA, USA), and maxillary and mandibular definitive working casts were poured using type-III dental stone (Microstone, Whip Mix Corp., Louisville, USA). Final cast and interocclusal bite were sent to laboratory for fabrication of screw retained acrylic prosthesis. The prostheses were adjusted to maintain occlusal point contacts in centric relation and anterior guidance in protrusion and group function in lateral excursions. Front profile with provisional prosthesis can be seen in [Table/Fig-6b].
a) Jaw relation record using Aluwax; b) Frontal profile with provisional prosthesis.
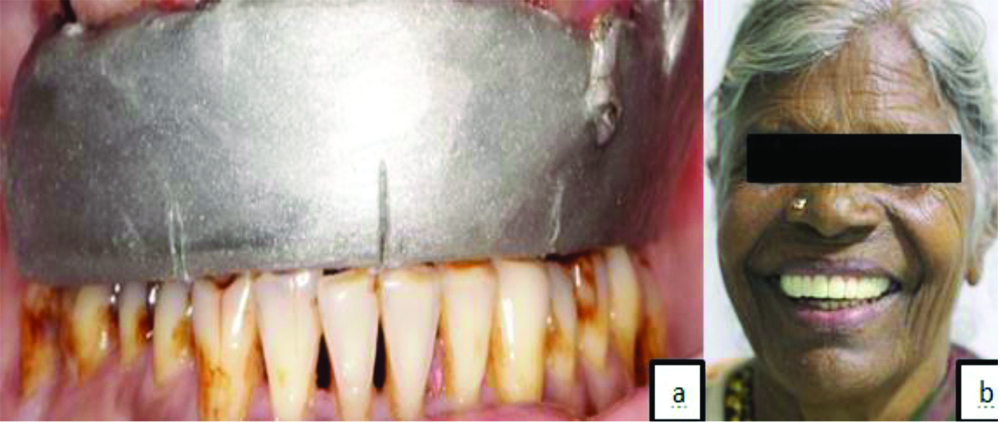
OPG was taken to confirm prosthesis fit. In each follow-up visit (after 1 day, 3 days, 1 week and 1 month), oral hygiene maintenance, prosthesis fit and healing assessed and were found to be satisfactory. After 3 months, provisional prosthesis was replaced with EXOCAD DMLS metal ceramic permanent fixed prosthesis adhering to previously mentioned steps [Table/Fig-7a-c]. Appropriate consent was obtained from the subject for using the images in the case report.
a) Permanent fixed Computer-Aided Design and Computer-Aided Manufacturing (CAD/CAM) prosthesis; b) OPG showing prosthesis loaded on 6 tilted implants; c) Frontal profile showing permanent CAD/CAM prosthesis.
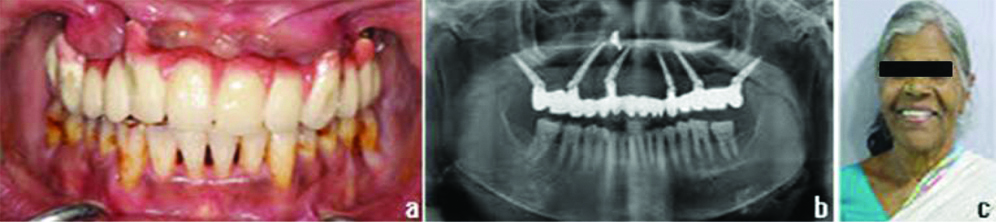
A follow-up of implant and prosthetic survival was done up to 1 year. There were no peri-implant pockets or implant mobility or any associated soft tissue changes. No radiolucency was observed on the OPG. The prosthesis was functioning well and did not show any chipping, fracture, screw loosening or screw fracture.
Discussion
Owing to maxillary sinus pneumatisation and osseous quality in the above patient, TTPHIL technique was used to obtain bicortical anchorage from nasal fossa, anterior wall of maxillary sinus and pterygomaxillary region minimising micromovements; thus, helping in better primary stabilisation [1-3]. Cortical engagement was possible due to longer, tilted implants. From biomechanical point of view, anterio-posterior position of implants provided favourable inter-implant distance [4], improved bone implant contact area, eliminated cantilever and consequently lead to efficient load distribution [5]. Complete cantilever elimination can be attributed to engagement of pterygoid cortex which compensated for poor osseous structure [2,5]. From clinical perspective, the protocol followed fulfilled pre requisite for immediate functional loading of implants by achieving high primary stability [6]. Moreover, the technique eliminated need for grafts, bypassed vital structures and reduced treatment cost [1]. Thereby, this implant distribution aided in the restoration and replacement of 14 maxillary teeth including second molars that improved chewing efficiency as compared to 10-12 teeth of all-on-4 concept.
The stability and function of loaded implants depend on robust peri-implant mucosal barrier [7,8]. Reduction in postoperative pain, swelling, intraoperative bleeding, surgical time, soft and hard tissues preservation and maintenance of blood supply are some advantages of flapless technique [9]. Furthermore, frequent dis/reconnections compromised mucosal barrier causing apical migration and marginal bone loss [10,11]. Yamada J et al., concluded that flapless guided surgery for immediate loaded fixtures depicted predictable outcome and high implant survival rate in edentulous maxilla [12]. Additionally, Martinez CPA et al., demonstrated that combining flapless surgery and subcrestal implant placement aids in preservation of crestal bone and increased osseointegration [13]. Subcrestal implant placement compensated for predictable bone loss by allowing bone regeneration and soft tissue growth by 1mm [14]. It facilitates osseointegration to abutment surface [15] and minimises thread exposure by formation of marginal tissue architecture enhancing aesthetic outcome [14,16].
For immediate functional loading in type-3 osseous bone quality, densification of surrounding bone is crucial for improved primary stability, bone-implant contact area and osseointegration. Drill surface aids in peripheral compaction of bone chips and debris through “osseodensification” [17]. Usage of single osteotomy drill reduced temperature [18], improved vascularization favouring bone regeneration [19]. Implant threads engage surrounding bone causing lateral condensation of spongy bone through “corticalisation” [20]. Hence, TTPHIL technique combined one stage, flapless surgery, single drill, subcrestal placement and basal cortical bone fixation allowing delivery of immediately loaded provisional fixed prosthesis by maintaining mucosal integration.
Biomechanical effects are compounded in poor bone quality and sinus pneumatisation [21]. Therefore to improve biomechanical efficiency, previous studies have advocated use of 6 implants for maxillary rehabilitation instead of conventional all-on-4 technique [22,23]. Nonetheless, these techniques cannot completely eliminate cantilever. Employing zygomatic implants can be invasive, technique sensitive and limited by anatomy of zygomatic bone [24]. One year follow-up, showing satisfactory clinical results elucidate in the direction of validation of TTPHIL technique in atrophic maxilla. Nevertheless, its use in more number of patients and long-term clinical and radiographic follow-up is needed for better validation of technique.
Conclusion(s)
The presented technique eliminated cantilever for maxillary rehabilitation using graftless, guided, single osteotomy, tilted six implants and 14 teeth, and was able to improve the clinical ease, patient acceptance and chewing efficiency in a single appointment. The patient was satisfied with implants and prosthesis, demonstrated good healing leading to overall success of implants and prosthesis at one year follow-up. By harnessing benefits of various concepts in implantology, this technique has been successful in providing patient and clinician centric treatment of severely atrophic maxilla.
[1]. Krekmanov L, Kahn M, Rangert B, Lindström H, Tilting of posterior mandibular and maxillary implants for improved prosthesis supportInt J Oral Maxillofac Implants 2000 15:405-14. [Google Scholar]
[2]. Salinas-Goodier C, Rojo R, Murillo-González J, Prados-Frutos JC, Three-dimensional descriptive study of the pterygomaxillary region related to pterygoid implants: A retrospective studyScientific Reports 2019 9(1):1617910.1038/s41598-019-52672-x31700047 [Google Scholar] [CrossRef] [PubMed]
[3]. Han CH, Mangano F, Mortellaro C, Park KB, Immediate loading of tapered implants placed in postextraction sockets and healed sitesJ Craniofac Surg 2016 27:1220-27.10.1097/SCS.000000000000275627391493 [Google Scholar] [CrossRef] [PubMed]
[4]. Maló P, de Araújo Nobre M, Lopes A, Rodrigues R, Tilted long implants in immediate functionClin Implant Dent Relat Res 2015 17:e134-42.10.1111/cid.1214424004159 [Google Scholar] [CrossRef] [PubMed]
[5]. Wang F, Huang W, Wu Y, Montanero-Fernandez J, Sheridan RA, Wang HL, Accuracy of cone beam computed tomography grayscale density in determining bone architecture in the posterior mandible: An in vivo study with microcomputed tomography validationInt J Oral Maxillofac Implants 2017 32(5):1074-79.10.11607/jomi.551828403249 [Google Scholar] [CrossRef] [PubMed]
[6]. Maló P, Rangert B, Dvärsäter L, Immediate function of Brånemark implants in the esthetic zone: A retrospective clinical study with 6 months to 4 years of follow-upClin Implant Dent Relat Res 2000 2(3):138-46.10.1111/j.1708-8208.2000.tb00004.x11359258 [Google Scholar] [CrossRef] [PubMed]
[7]. Perrotti V, Zhang D, Liang A, Wong J, Quaranta A, The effect of one-abutment at one-time on marginal bone loss around implants placed in healed bone: A systematic review of human studiesImplant Dent 2019 28(6):603-12.10.1097/ID.000000000000093131373902 [Google Scholar] [CrossRef] [PubMed]
[8]. Van der Zee E, Oosterveld P, Van Waas MA, Effect of GBR and fixture installation on gingiva and bone levels at adjacent teethClin Oral Implants Res 2004 15(1):62-65.10.1111/j.1600-0501.2004.01005.x14731178 [Google Scholar] [CrossRef] [PubMed]
[9]. Brodala N, Flapless surgery and its effect on dental implant outcomesInt J Oral Maxillofac Implants 2009 24:118-25. [Google Scholar]
[10]. Borie M, Lecloux G, Bosshardt D, Barrantes A, Haugen HJ, Lambert F, Peri-implant soft tissue integration in humans-influence of materials: A study protocol for a randomised controlled trial and a pilot study resultsContemp Clin Trials Commun 2020 19:10064310.1016/j.conctc.2020.10064333083628 [Google Scholar] [CrossRef] [PubMed]
[11]. Byrne G, Outcomes of one-stage versus two-stage implant placementJ Am Dent Assoc 2010 141(10):1257-58.10.14219/jada.archive.2010.005420884929 [Google Scholar] [CrossRef] [PubMed]
[12]. Yamada J, Kori H, Tsukiyama Y, Matsushita Y, Kamo M, Koyano K, Immediate loading of complete-arch fixed prostheses for edentulous maxillae after flapless guided implant placement: A 1-year prospective clinical studyInt J Oral Maxillofac Implants 2015 30(1):184-93.10.11607/jomi.367925615924 [Google Scholar] [CrossRef] [PubMed]
[13]. Martínez CPA, Vlahović Z, Šćepanović M, Videnović G, Barone A, Calvo-Guirado JL, Submerged flapless technique vs. conventional flap approach for implant placement: Experimental domestic pig study with 12-month follow-upClin Oral Implants Res 2016 27(8):964-68.10.1111/clr.1266526147852 [Google Scholar] [CrossRef] [PubMed]
[14]. Koh RU, Oh TJ, Rudek I, Neiva GF, Misch CE, Rothman ED, Hard and soft tissue changes after crestal and subcrestal immediate implant placementJ Periodontol 2011 82(8):1112-20.10.1902/jop.2011.10054121284552 [Google Scholar] [CrossRef] [PubMed]
[15]. Degidi M, Perrotti V, Shibli JA, Novaes AB, Piattelli A, Iezzi G, Equicrestal and subcrestal dental implants: A histologic and histomorphometric evaluation of nine retrieved human implantsJ Periodontol 2011 82(5):708-15.10.1902/jop.2010.10045021138355 [Google Scholar] [CrossRef] [PubMed]
[16]. Novaes AB Jr, Barros RR, Muglia VA, Borges GJ, Influence of interimplant distances and placement depth on papilla formation and crestal resorption: A clinical and radiographic study in dogsJ Oral Implantol 2009 35(1):18-27.10.1563/1548-1336-35.1.1819288884 [Google Scholar] [CrossRef] [PubMed]
[17]. Podaropoulos L, Increasing the stability of dental implants: The concept of osseodensificationBalk J Dent Med 2017 21(3):133-40.10.1515/bjdm-2017-0023 [Google Scholar] [CrossRef]
[18]. Bettach R, Taschieri S, Boukhris G, Del Fabbro M, Implant survival after preparation of the implant site using a single bur: A case seriesClin Implant Dent Relat Res 2015 17(1):13-21.10.1111/cid.1208223659356 [Google Scholar] [CrossRef] [PubMed]
[19]. Galindo-Moreno P, Nilsson P, King P, Becktor J, Speroni S, Schramm A, Clinical and radiographic evaluation of early loaded narrow diameter implants- 1-year follow-upClin Oral Impl Res 2012 23:609-16.10.1111/j.1600-0501.2011.02254.x22093047 [Google Scholar] [CrossRef] [PubMed]
[20]. Ali SM, Othman KS, Samad AA, Kh Mahmud P, Comparison between basal and conventional implants as a treatment modality in atrophied ridgesJ Dent Implant Res 2019 38(2):48-54. [Google Scholar]
[21]. Torrecillas-Martínez L, Monje A, Lin GH, Suarez F, Ortega-Oller I, Galindo-Moreno P, Effect of cantilevers for implant-supported prostheses on marginal bone loss and prosthetic complications: Systematic review and meta-analysisInt J Oral Maxillofac Implants 2014 29(6):1315-21.10.11607/jomi.366025153006 [Google Scholar] [CrossRef] [PubMed]
[22]. Testori T, Del Fabbro M, Capellini M, Zuffetti F, Francetti L, Weinstein RL, Immediate occlusal loading and tilted implants for the rehabilitation of the atrophic edentulous maxilla: 1-year interim results of a multicenter prospective studyClin Oral Implants Res 2008 19:227-32.10.1111/j.1600-0501.2007.01472.x18177428 [Google Scholar] [CrossRef] [PubMed]
[23]. Pomares C, A retrospective clinical study of edentulous patients rehabilitated according to the “all-on-four” or the “all-on-six” immediately function conceptEur J Oral Implantol 2009 2(1):55-60. [Google Scholar]
[24]. Dominguez EA, Guerrero C, Shehata E, Van Sickels JE, Zygoma implants or sinus lift for the atrophic maxilla with a dentate mandibleDent Clin N Am 2019 63(3):499-513.10.1016/j.cden.2019.02.01331097141 [Google Scholar] [CrossRef] [PubMed]