The Percutaneous Nephrolithotomy (PCNL) a common endourologic procedure for removal of renal stones is associated with significant pain owing to nephrostomy tube placement [1,2]. Various modalities for postoperative analgesia after PCNL include systemic narcotics and Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), port site infiltration, paravertebral block, intercostal block, epidural block and more recently quadratus lumboram and erector spinae blocks [3-5]. Patients undergoing renal surgeries may suffer from impaired renal function which necessitates judicious use of sedatives and NSAIDs. Hence, regional analgesic technique would be a better option.
Intercostal Nerve Block (INB) is an age old effective regional block. Peritubal infiltration from renal capsule to skin under fluoroscopic guidance would also alleviate pain after PCNL and is technically simple [4,5].
Looking into the limited published literature that compares these two techniques, this study was conducted aiming to compare the analgesic efficacy of INB with fluoroscopic guided peritubal infiltration using bupivacaine. Primary outcome was duration of analgesia and secondary outcomes were total analgesic requirement in 24 hours, pain scores at various time intervals in postoperative period, intraoperative haemodynamics and any complications.
Materials and Methods
After getting institutional research and ethics committee approval (GMCKKD/ RP2016/EC/227) this randomised clinical study was registered in clinical trial registry of India (CTRI/2018/03/012354). The study was conducted as per Consolidated Standards of Reporting Trials (CONSORT) guidelines, from May 2018 to October 2018, in a tertiary care teaching hospital.
Inclusion criteria: Eighty patients scheduled for PCNL of age between 20 to 60 years, belonging to American Society of Anaesthesiologist’s (ASA) physical status I and II with a Body Mass Index (BMI) of 18-25 kg/m2 were recruited for the study.
Exclusion criteria: Patients with history of allergy to local anaesthetics, chronic pain syndromes, coagulopathy, infection at site of block, chest deformities and stone size of >2 cm were excluded from the study.
Sample size calculation and group division: Sample size calculation was done using the formula
where Zα/2=the critical value of the Normal distribution at α/2 (for a confidence level of 95%, α is 0.05 and the critical value is 1.96), Zβ=the critical value of the Normal distribution at β (for a power of 80%, β is 0.2 and the critical value is 0.84), σ2=the population variance which was calculated using the formula . Using the data from the study by Parikh GP et al., and taking d as 1 hour (a clinically significant difference of pain free interval between the groups), the sample size estimated was 34 in each group [6]. Considering 15% drop out, 40 patients were recruited in each group using computer generated randomisation chart.
Group IC received intercostal nerve block and group IF received peritubal infiltration with bupivacaine under fluoroscopic guidance. Method of concealment was sequentially numbered, sealed, opaque envelopes. Patients who met the inclusion criteria were randomly allocated to two groups of 40 each using computer generated randomisation chart. Group IC received intercostal nerve block and group IF received peritubal infiltration with bupivacaine under fluoroscopy guidance. Method of concealment was sequentially numbered, sealed, opaque envelopes.
All patients were assessed preoperatively by detailed history, physical examination and laboratory evaluation. On the day before surgery, procedure was explained to each patient and informed written consent was taken for participation to study. The Numeric Rating Scale (NRS) was also explained to them for postoperative pain assessment. All patients were given tab alprazolam 0.5 mg on the night before surgery.
On arrival to the operation theatre, after application of Electrocardiography (ECG), pulse oximeter (SpO2) and Non-Invasive Blood Pressure (NIBP), patients were premedicated with midazolam 0.02 mg/kg, glycopyrrolate 0.2 mg and fentanyl 2 μg/kg Intravenously (IV). After preoxygenation, General Anaesthesia (GA) was induced with propofol 2.5 mg/kg and succinyl choline 1.5 mg/kg followed by intubation with appropriate size endotracheal tube. Anaesthesia was maintained with isoflurane (0.8-1.5%) in O2+N2O mixture and atracurium. All patients were given paracetamol 1 gm as IV infusion after intubation. After positioning the patients prone for surgery and checking vitals, the blocks were performed pre-emptively by consultant anaesthesiologist and time of block was noted.
In group IC, patients received intercostal nerve block under landmark guidance with 0.25% bupivacaine 5 mL each at 10,11,12 intercostal spaces. Inferior edge of each targeted rib was palpated 6-8 cm from midline with index finger of left hand. A 23 gauge short bevel needle attached to a 10 mL syringe was inserted at the tip of finger until it touched the rib. The fingers of left hand grasped needle hub tightly and walked the needle 3-5 mm off the lower rib edge where 5 mL of drug was injected after negative aspiration.
In group IF, peritubal infiltration was given with 15 mL 0.25% bupivacaine. This was done using a 23 G Quincke type spinal needle under fluoroscopic guidance assisted by the surgeon. The needle was advanced upto renal capsule along the expected nephrostomy tube insertion track and local anaesthetic was injected while withdrawing the needle throughout the whole depth (renal capsule, muscles, subcutaneous tissue and skin). Heart rate, SpO2, Non-Invasive Blood Pressure (NIBP) and end tidal carbondioxide were monitored throughout the surgery at five minute intervals. Patients were also monitored for rise in airway pressures throughout procedure and bilateral equal air entry was confirmed by auscultation at the end. After completion of surgery, all patients were shifted to post-anaesthesia recovery room after reversal of residual neuromuscular blockade and extubation. Surgical procedures lasting more than three hours or converted to open stone surgery due to surgical difficulty were excluded from the study. In the study institution, PCNL was performed for stone size of less than 2 cm only and so multiple punctures requiring deviation from initial puncture site are unlikely. Nephrostomy tube used was 16 F for all cases.
The time of arrival of patient in recovery room was taken as zero hour. Further monitoring was continued in the Intensive Care Unit (ICU). Postoperative pain scores were assessed at zero hour, 1 hour, 2 hour, 3 hour, 6 hour, 12 hour and 24 hour by NRS during rest and after voluntary coughing (dynamic pain). Rescue analgesics were given when the NRS score ≥4 or whenever patients requested for analgesics. Tramadol 1.5 mg/kg with ondansetron 0.1 mg/kg IV was the first rescue analgesic and paracetamol 1gm IV infusion was the second rescue analgesic. All patients were monitored for any adverse effects like nausea, vomiting, bradycardia, breathing difficulty or desaturation. Duration of analgesia was taken from the time of block to the time of first rescue analgesic administration. Total rescue analgesic requirement in 24 hours was also noted.
Monitoring and data collection was done by the primary investigator who was blinded to the study groups. To ensure blinding the consultant anaesthesiologist, who performed the block, was not involved with the study further and the data assessor was also blinded about the group allocation.
Statistical Analysis
Data was analysed using Statistical Package for Social Sciences (SPSS) version 18 (IBM Corp, Armonk, NY, USA). Chi-square test was used to analyse all categorical variables and independent student’s t-test was used for quantitative variables. Data was expressed as mean±standard deviation (SD) and a p-value of <0.05 was considered significant.
Results
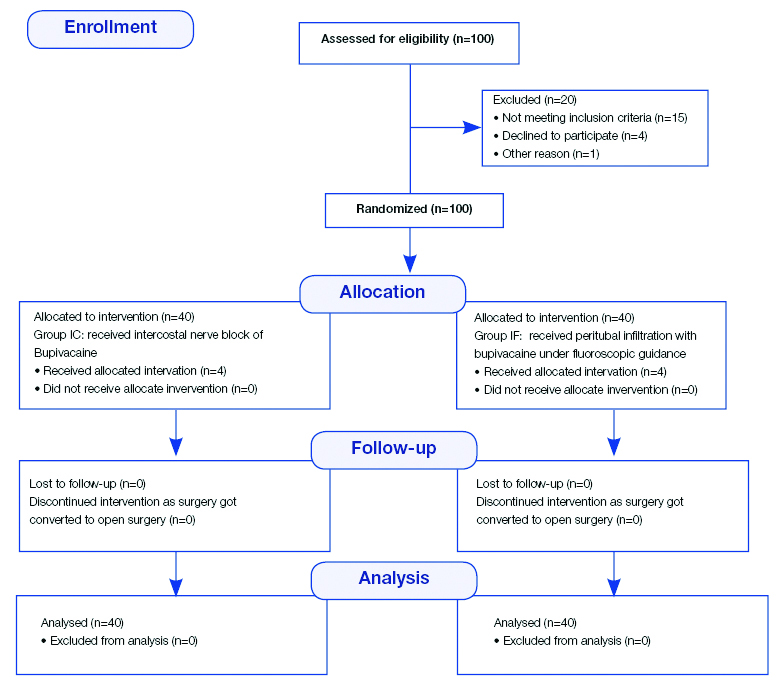
All the enrolled 80 patients completed the study. The CONSORT flow diagram for the study is depicted in [Table/Fig-1]. Both groups were comparable with respect to age, sex, height, weight, BMI and ASA physical status [Table/Fig-2].
| Parameters | Group IC (n=40) | Group IF (n=40) | p-value |
|---|
| Sex (male:female)* | 30:10 | 31:9 | 0.793* |
| ASA PS (I:II)* | 19:21 | 21:19 | 0.655* |
| Age (years) | 44.55±12.184 | 41.45±10.241 | 0.222† |
| Weight (kg) | 65.22±10.080 | 64.55±9.751 | 0.762† |
| Height (cm) | 163.03±5.577 | 161.63±6.067 | 0.286† |
| BMI (kg/m2) | 24.407±2.664 | 24.574±2.517 | 0.774† |
†Chi-square test; *Independent t-test; ASA: American anaesthesiology society; IC: Inter-costal nerve block; IF: Peritubal infiltration nerve block; p-value <0.05 considered significant
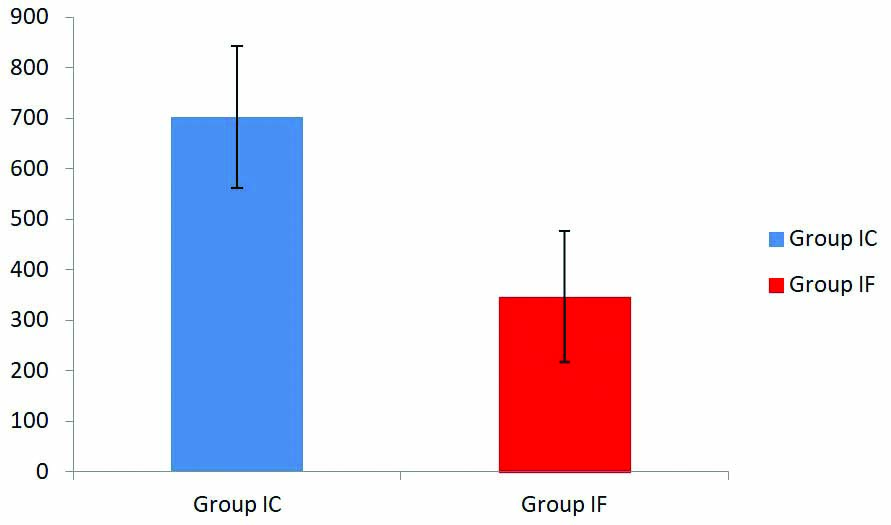
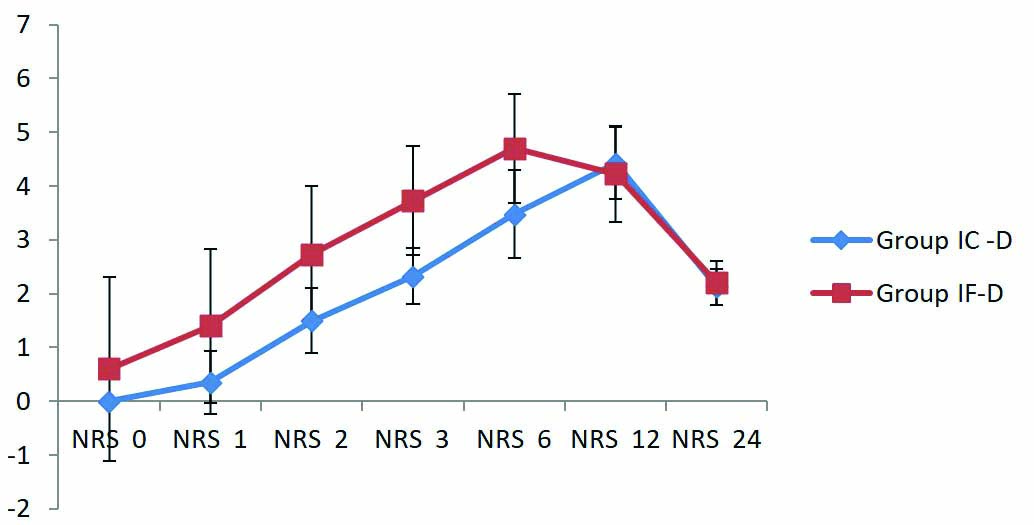
The duration of analgesia was 702.00±140.02 minutes in group IC and 346.50±129.56 minutes in group IF which was significant statistically with a p-value of <0.001 [Table/Fig-3]. The resting NRS score for pain was zero at recovery in the group IC whereas in group IF it was 0.57±1.615. The mean resting and dynamic pain scores were significantly lower in group IC at all time points up to 12 hour postoperatively compared to group IF and this difference was statistically significant with a p-value less than 0.05 [Table/Fig-4,5].
Comparison of duration of analgesia.
Postoperative resting pain scores. NRS-Numerical rating scale.
R: Resting
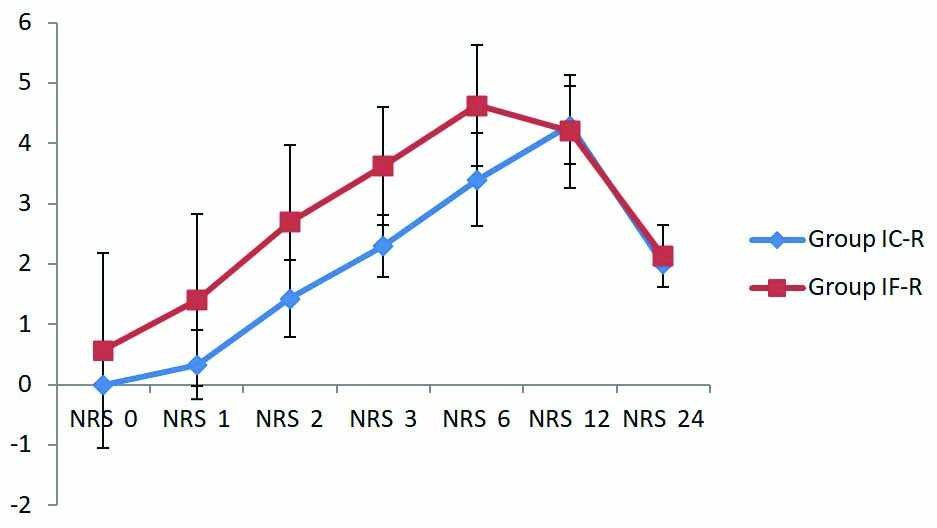
Postoperative dynamic pain scores.
D: Dynamic
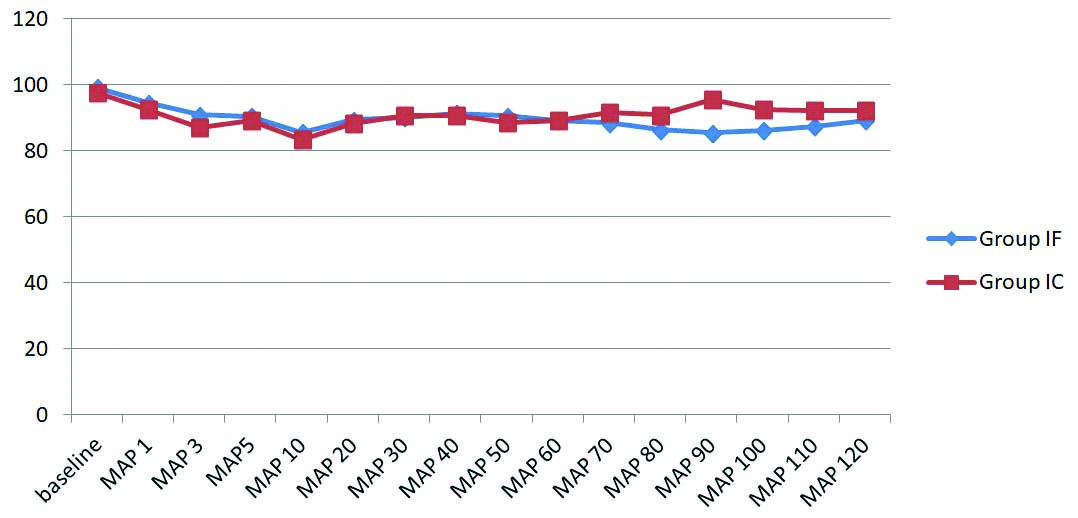
There was significant difference in postoperative rescue analgesic requirements too. Both tramadol (50.00±11.32 mg vs 82.50±24.15 mg) and paracetamol (100±303.82 mg vs 850±622.23 mg) requirements were lower in group IC with p-values less than 0.001 [Table/Fig-6]. Haemodynamics were stable intraoperatively and mean arterial pressures were comparable between groups at all time frames (p-value 0.909) [Table/Fig-7]. There were no incidences of block failure, desaturation, breathing difficulty, nausea or vomiting.
Comparison of rescue analgesic requirement in 24 hours.
| Rescue analgesic | Group IC (n=40) | Group IF (n=40) | p-value |
|---|
| Tramadol (mg) (mean±SD) | 50.00±11.323 | 82.50±24.152 | <0.001† |
| Paracetamol (mg) (mean±SD) | 100±303.823 | 850±622.237 | <0.001† |
†Independent t-test; p-value <0.05 considered significant
Mean arterial pressure.
MAP: Mean arterial pressure
Discussion
In this randomised study, that compared the effects of INB and fluoroscopic guided peritubal infiltration, administered pre-emptively, in mitigating postoperative pain after PCNL with respect to primary outcome of duration of analgesia and secondary outcomes of total analgesic requirement in 24 hours, pain scores at various time intervals in postoperative period, intraoperative haemodynamics and any complications. Since both blocks were administered before surgical procedure, they offered effective preventive analgesia. The results showed that INB is more effective than fluoroscopic guided peritubal infiltration. The time to first demand of rescue analgesic was significantly prolonged (p-value <0.001) with INB compared to peritubal infiltration.
The resting and dynamic NRS scores were significantly low with INB for first six hours. The total 24 hour requirement of first and second rescue analgesics (tramadol and paracetamol respectively) was also less with INB with a p-value of <0.001. There were no procedure related complications and intraoperative haemodynamics were stable. Thus, although INB is technically more challenging compared to peritubal infiltration, it provides superior analgesia. Peritubal infiltration is also a popular technique for postoperative analgesia after PCNL. In this study, the authors used fluoroscopic guidance for infiltration to improve the precision and efficacy. No study in the past compared the effectiveness of pre-emptively administered fluoroscopic guided peritubal infiltration and INB using 0.25% bupivacaine.
PCNL is associated with significant pain owing to nephrostomy tube placement though it has other advantages over open stone surgery in terms of reduced hospital stay, decreased morbidity and early return to normal activity [1,2]. As pain after PCNL is complex in nature, no analgesic technique is 100% effective and may require a multimodal approach. Ineffective postoperative pain relief is associated with complications like delayed recovery, increased pulmonary and cardiac complications, Deep Vein Thrombosis (DVT), prolonged hospital stay and development of chronic neuropathic pain [7].
In a well-matched study, Jonnavithula N et al., compare analgesic efficacy of Peritubal Block (PB) with INB administered after surgery using ropivacaine as local anaesthetic [5]. In this study, the pain scores were lower in INB group for 24 hours, similar to observations of present study. The mean time to first demand for rescue analgesia was higher with intercostal block. The number of demands and the amount of analgesics consumed were also less in INB group.
In another Randomised Controlled Trial (RCT), contrary to the present study findings, PTB was associated with significantly lower postoperative pain compared to INB [4]. The mean Visual Analogue Scale (VAS) scores were lower in PTB group for first 48 hours. The time to first demand of analgesia was significantly higher with PTB compared to INB. This discrepancy in results may be due to the performance of PTB after surgery which is likely to be more precise especially in cases of multiple punctures. The total diclofenac consumption was also higher with INB compared to PTB.
In a Randomised Clinical Trial (RCT) by Ozkan D et al., ultrasound guided INB provided effective analgesia after PCNL with less 24-hour opioid requirement [8]. In the present study, also total requirement of first and second rescue analgesics were lower with INB. Peritubal infiltration with 0.25% bupivacaine was effective in alleviating pain after PCNL in another randomised study [9]. In this study, the duration of analgesia was nine hours and requirement of tramadol in the first 24 hour was 119.3 mg.
In a placebo controlled RCT of INB after PCNL, Honey RJ et al., used 20 mL 0.5% bupivacaine with epinephrine and the patients received IV narcotic based Patient Controlled Analgesia (PCA) postoperatively [10]. They concluded that INB with bupivacaine significantly improves pain control and health related quality of life postoperatively. This action of bupivacaine however disappears after six hours of surgery, following which difference in narcotic use becomes indistinguishable. This result is comparable to ours in that resting and dynamic NRS scores were lower in INB group for first six hours although lower concentration of bupivacaine (0.25%) was used in the present study.
Ropivacaine is another amide local anaesthetic with longer duration of action. An RCT by Parikh GP et al., compared ultrasound guided peritubal infiltration of 0.25% bupivacaine and 0.25% ropivacaine for pain relief after PCNL and concluded that ropivacaine is more effective than bupivacaine in terms of resting and dynamic VAS scores as well as mean time to first rescue analgesic [6]. To prolong the duration of action of peritubal infiltration, buprenorphine was added to bupivacaine in a study by Nirmala J et al., [11].
Analysing the results of present study and similar studies from literature it is clear that INB is a very good analgesic technique for pain relief after PCNL. To improve the duration of action of bupivacaine we can add adjuvants like buprenorphine. Fluoroscopic guided peritubal infiltration is also a good alternative to INB. Ultrasound guidance may be used to avoid potential complications of INB as well as to improve the precision. Studies comparing ultrasound guided INB and paravertebral block with newer techniques like erector spinae and quadrates lumborum blocks may be done in the future to alleviate pain after PCNL [12,13].
Limitation(s)
One of the major limitations of this study was that patient satisfaction was not assessed as an independent variable using objective scoring system. Also, authors failed to analyse duration of surgery although all surgeries lasted less than two hours only.
Conclusion(s)
Intercostal Nerve Block (INB) provides superior analgesia compared to fluoroscopic guided peritubal infiltration after PCNL as evidenced by prolonged duration of analgesia, lower pain scores in first six hours and reduced total analgesic consumption in 24 hours postoperatively.
†Chi-square test; *Independent t-test; ASA: American anaesthesiology society; IC: Inter-costal nerve block; IF: Peritubal infiltration nerve block; p-value <0.05 considered significant
†Independent t-test; p-value <0.05 considered significant