Hernias occurring through the anterior abdominal wall are classified as ventral hernias and further as primary and secondary. Primary ventral hernias include umbilical, epigastric, spigelian, and lumbar hernias, while secondary ventral hernias include the incisional hernias occurring following a previous operation [1]. Ideally, all ventral hernias require mesh repair to prevent recurrence. However, small hernias especially umbilical and paraumbilical, have been managed without a mesh. Mesh repairs particularly for umbilical hernias are associated with recurrence rates of 1%, whereas those of the simple suture technique are associated with a recurrence of upto 16% [2].
Mesh repair has evolved over the years and several studies have been conducted comparing various types of meshes and approaches [2,3]. The introduction of prosthetic meshes post the earlier primary suture closure, resulted in a decrease in recurrence rates from 63% to 32% [3]. Laparoscopic repair with prosthetic mesh also showed good results. Some studies done on umbilical, paraumbilical hernias comparing the open and laparoscopic approach and concluded that though the hospital stay was shorter in the laparoscopic group, there was no significant difference in the short term complications observed [4-6]. However, in general, laparoscopic repairs are associated with smaller scars, less postoperative pain, shorter hospital stay, and less wound related complications like wound infection, but longer operation time and higher disposable material cost compared to the open approach [7].
Several attempts have been made to utilise the pros of both approaches and reduce the cons. One such effort is the use of dual mesh patch repair (Ventralex patch). These patches are available in different sizes and are used as intra peritoneal meshes using an open approach. Careful selection of mesh size and patients are important and defect size should be less than 3-4 cm in diameter without divarication of recti to have adequate overlap [8,9]. This is the first series in India reporting the results with the use of reinforced deployment patch of layered lightweight polypropylene, coated with a heat bonded gel of Omega-3 Fatty Acid (O3FA).
This study was conducted to describe an open technique in ventral hernia repair and describe the complication profile of this procedure with specific focus on recurrence rate.
Materials and Methods
The present study was a retrospective study which was conducted at the Department of General Surgery Unit IV, Christian Medical College and Hospital, Vellore, Tamil Nadu, India and was approved by Institutional Review Board (approval number 13891 dated 24/03/2021). Data was collected from 1st January 2011 to 31st December 2017 using electronic hospital record data base. Data entry and analysis was done over a period of two months (April 2020-May 2020).
Inclusion criteria: The demographic details of all the patients who had hernia repair with Ventralex patch between January 2011-December 2017 under general surgery unit 4 alone were included in the study.
Exclusion criteria: No patient was excluded within the time period of the study.
Sample size: There were total of 248 patients who underwent hernia repair using a Ventralex patch from January 2011 to December 2017, all of whom were recruited in this study.
Two years after our last hernia repair between 1st January 2020 to 31st March 2020 a telephonic survey and chart review was conducted to enquire about the potential surgical complications that had risen without our knowledge postoperatively.
Prosthesis
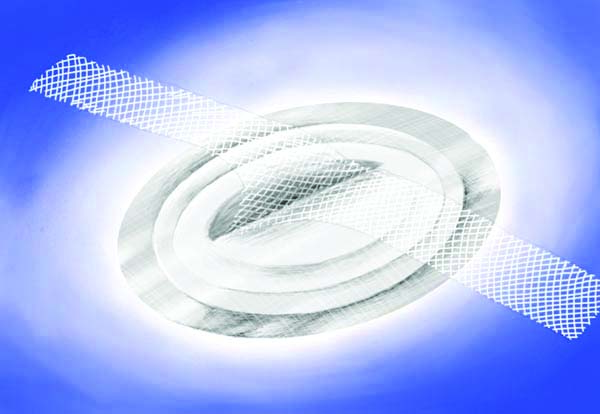
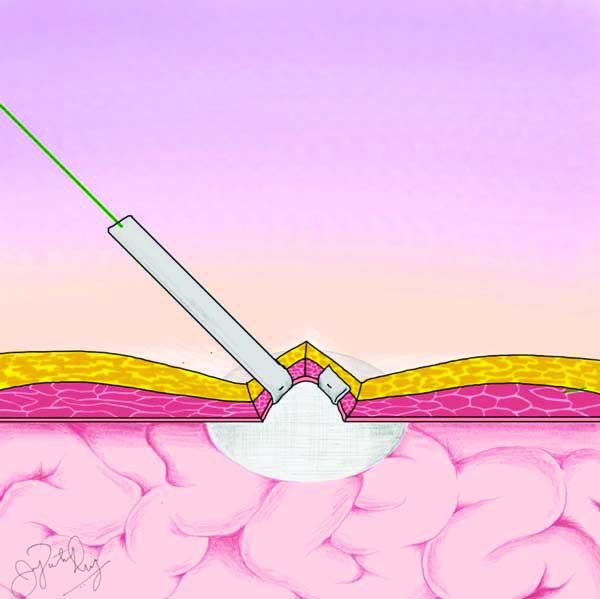
The Ventralex Patch prosthesis is a composite poly tetra-fluoro ethylene and polypropylene mesh with an O3FA-coated washer designed to maintain a smooth contact surface for incorporation around the hernia defect [8]. The visceral side of the patch includes an anti-adhesive barrier layer coated with O3FA, and the anterior layer of mesh has a light spray O3FA coating on the monofilaments [Table/Fig-1]. The device also contained two fixation straps that allow the perimeter of the Ventralex Patch to be tightly secured to the abdominal wall and promote uniform incorporation. The fixation straps were to be sutured to the facial sheath using 1-0 Prolene or 2-0 prolene with minimum of 2 sutures and a maximum of 6 sutures based on surgeon’s preference [8]. The prosthesis is available in three standard sizes- small, medium, and large.
Ventralex patch; Two layered patch with inner prolene layer and outer Omega-3 Fatty Acid (O3FA) coated layer.
Procedure
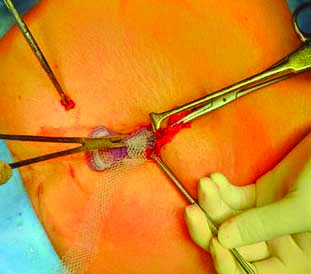
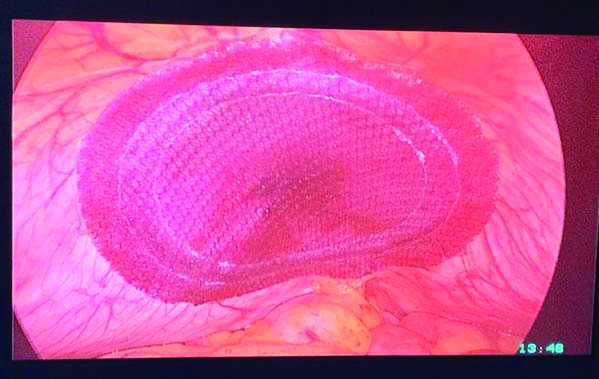
The operative procedure includes making a small incision of 2-5 cm, entering the hernia sac and reducing the content. Next, the hernia patch is placed intraperitoneally and both fixation tabs are anchored to fascia using non-absorbable sutures [Table/Fig-2,3,4,5,6]. Taking extra fixation sutures and facial defect closure is optional. Skin and subcutaneous tissue are closed with absorbable sutures. In few cases author had confirmed the lie and placement of mesh using diagnostic laparoscopy postmesh fixation [Table/Fig-7].
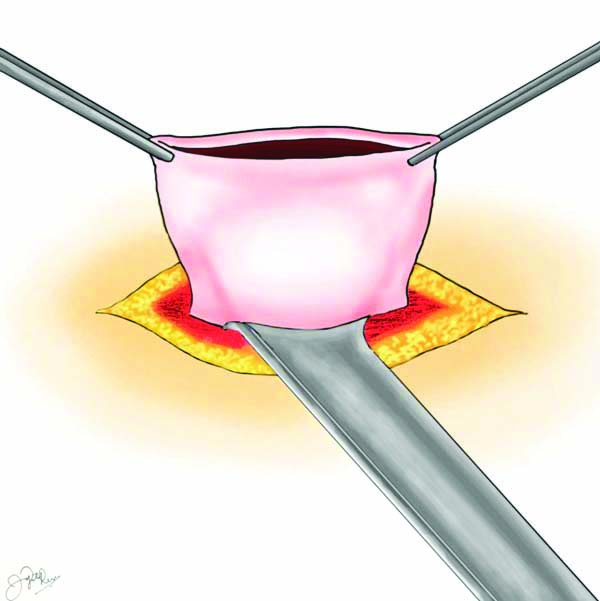
Placement of mesh into the peritoneal cavity.
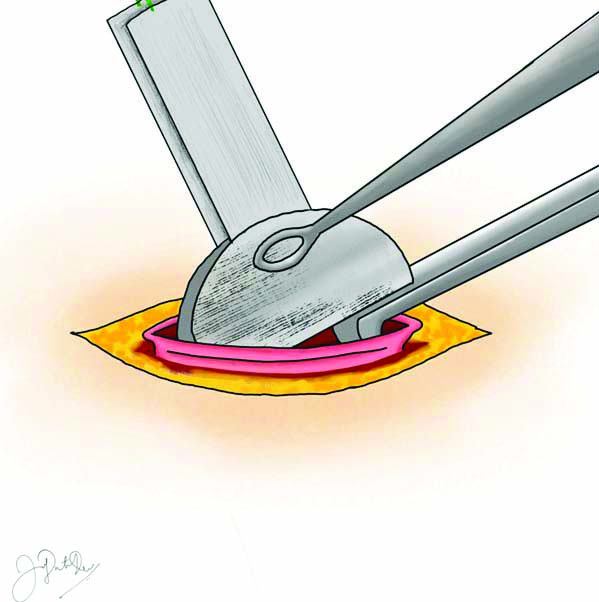
Positioning of mesh in the peritoneal cavity.
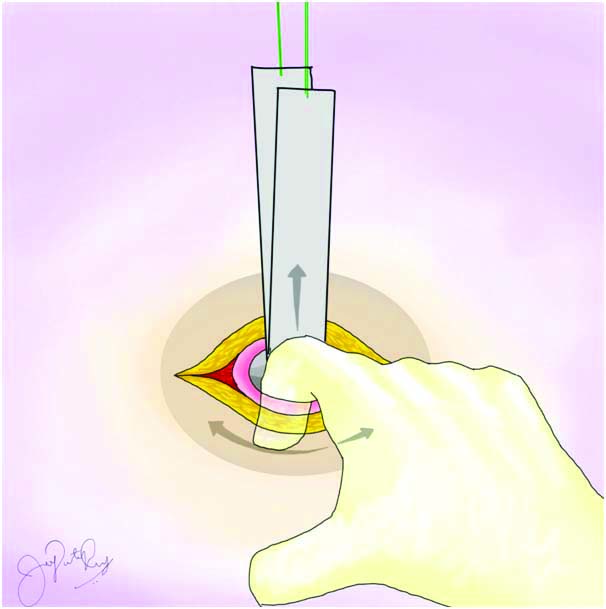
Anchoring of mesh to the muscle.
Intraoperative image of mesh placement.
Laparoscopic view of mesh lie in the peritoneal cavity.
Data collection: The patients were followed-up postoperatively, at first and third week in the Outpatient Department (OPD) following the operation. During this period, patients were assessed for the wound integrity, presence of necrosis, superficial skin infections, seroma, skin dehiscence, and recurrence. Authors also followed-up with all the patients through a telephonic survey two years after the last hernia repair in the study to look for recurrence and other complications. A total of 207 patients did not require follow-up after three weeks, but were provided with the office telephone number and email address, if ever the need arose. The average laparoscopic and traditional open sublay cost was arrived from data from our institutional electronic record database. This group of patients were not part of the study group. However, they were randomly selected from the electronic hospital data base only for cost-analysis.
Statistical Analysis
Descriptive statistics reported using frequency and percentage for categorical variables. Continuous variables reported using mean±SD. Comparison of mean reported using two independent sample test. Association between categorical variables reported using Chi-square/Fisher’s-Exact test. Statistical Package for the Social Sciences (SPSS) 21.0 (IBM Bangalore) software was used.
Results
A total of 248 patients were recruited for this study over a seven year period. The patients’ mean age was 50.57 years (minimum being 22 years and maximum being 100 years). Most of them were female {151, (60.89%)}. The mean BMI was 28.37 kg/m2, with the minimum being 14 kg/m2 and maximum being 49.4 kg/m2. The mean duration of the operation was 27.5 minutes and the mean length of hospital stay was 2.275 days (Hospital stay calculated from the day of operation to discharge) [Table/Fig-8]. Total 217 patients (87.5%) were discharged within 4 days’ time.
| Maximum | Minimum | Mean |
|---|
| Age (years) | 100 | 22 | 50.57 |
| Sex | 97 males | 151 females | |
| BMI (kg/m2) | 49.4 | 14 | 28.37 |
| Duration of operation (minutes) | 35 | 15 | 27.5 |
| Duration of hospital stay (days) | 17 | 1 | 2.275 (calculated from date of operation to discharge) |
There were 126 patients who had pain as their presenting complaint and 246 with swelling as their presenting complaint. Four patients presented with obstruction. There were 74 umbilical hernias (29.8), 107 paraumbilical hernias (43.2%), 11 epigastric hernias (4.4%) and 56 incisional hernias (22.6%) [Table/Fig-9]. Defects were classified into three groups based on size.
Clinical parameters and co-morbidities.
| Parameter | | Number (percentage) |
|---|
| Type of hernias | Umbilical | 74 (29.8%) |
| Paraumbilical | 107 (43.2%) |
| Epigastric | 11 (4.4%) |
| Incisional | 56 (22.6%) |
| Defect size | Upto 1 cm | 60 (24.2%) |
| 2-4 cm | 182 (73.34%) |
| >4 cm | 6 (0.024%) |
| Co-morbidities | Diabetes mellitus | 72 (29%) |
| Hypertension | 86 (34.7%) |
| Chronic obstructive pulmonary disease | 26 (10.5%) |
| Obesity | 65 (26.2%) |
| Chronic kidney disease | 5 (2%) |
| Previous operations | 135 (54.7%) |
Defects smaller than 1 cm comprised of 24.2% (60 cases), defects ranging from 2-4 cm comprised of 73.34% (182 cases), and defects over 4 cm accounted for 0.02% (6 cases) [Table/Fig-9]. The most common defect size was 2 cm (117 patients, 47.2%).
Complications: A total of 21 patients (8.5%) developed surgical site infection of which five were found during hospital stay, 15 in the first week outpatient follow-up and one patient in the second week follow-up. A total of 27 patients (10.9%) had seroma out of which 20 were detected in the first week and seven in the second week of outpatient follow-up. One patient developed an entero-cutaneous fistula and another patient, an infected sinus both were picked up during hospital stay. A total of six patients developed superficial skin necrosis [Table/Fig-10]. A total of 16 hernia recurrences (6.5%; 13 females and 3 males) were reported. All the recurrences occurred within the first year of the operation. There were three recurrences in those patients with umbilical hernias (3/74), seven recurrences noted in patients with para-umbilical hernias (7/107), and six recurrences noted in patients with incisional hernias (6/56) [Table/Fig-10]. There were no recurrences noted in patients with epigastric hernia repairs. Of the patients with recurrences, two were previously diagnosed with Chronic Obstructive Pulmonary Disease (COPD), and four with diabetes mellitus. Seven patients were obese and had a BMI greater than 30 kg/m2. Cost analysis was done on in-patient hospital bill including disposables for all 248 patients which showed an average cost of INR.35,142/-.
Presence and percentage of postoperative complications.
| Complications | Numbers (Percentage) |
|---|
| Recurrences | 16 (6.5%) |
| Surgical site infections | 21 (8.5%) |
| Seroma | 27 (10.9%) |
| Entero-cutaneous fistula | 1 (0.004%) |
| Infected sinus | 1 (0.004%) |
| Skin necrosis | 6 (2.4%) |
Discussion
In the present study, 248 patients who underwent an open ventral hernia repair were investigated over a 2-7 year duration. There were a total of 16 recurrences (6.5%) documented during this study period. Study group was unique as it involved primary and incisional ventral hernias with a majority of them having a defect size of 2-3 cm. In literature there are no studies comparing laparoscopic or open mesh repair in this sub group of hernias. However, a meta-analysis of laparoscopic vs open repair for umbilical, paraumbilical hernias revealed that laparoscopic repair may be associated with a lower risk of wound infection, wound dehiscence, and shorter length of stay, lower recurrence but longer operative time and higher disposable cost [10]. However, meta-analysis of Randomised Controlled Trials (RCTs) alone on ventral hernias did not show any difference in recurrence rate [11].
Theoretically, this approach appears to have the advantage of both laparoscopic approach (less hospital stay and smaller scar) and open approach (shorter operation time and less disposable cost) in small defect hernias (≤4 cm). However, it is important to know whether short and long term complications are comparable to other repairs. There are similar studies in literature using ventral patch repair for small hernias. [Table/Fig-11] shows the comparison of present study complications with similar studies [8,12-17].
Comparison of outcomes with similar ventral patch studies [8,12-17].
| Study | Type of study | Number of patients | Wound infection | Operation time | Hospital stay | Period of follow-up | Recurrence rates |
|---|
| Hadi HI et al., [12] | Prospective single centre study | 51 | 5.8% | 30 minutes | 1day | 4-26 months | 2% |
| Vychnevskaia K et al., [13] | Prospective single centre study | 101 | 2% | 33 minutes | 2 days | Mean is 28.5 months | 2% |
| Iversen E et al., [14] | Retrospective chart review | 152 | 3.3% | 39 minutes | NA | Mean 15.6 months | 2.6% |
| Berrevoet F et al., [15] | Prospective single centre study | 126 | 4 | 36.2±15.6 minutes | 0-2 days | Median 25 months | 2.8% |
| Martin DF et al., [16] | Retrospective chart review | 88 | 2.2% | 52 minutes | 1 day | Median 27 days | 0% |
| Tollens T et al., [8] | Retrospective chart review | 176 | 3% | NA | NA | Mean follow up 49 months | 8.9% |
| Ambe P et al., [17] | Retrospective chart review | 57 | 7.01% | 30.7minutes | 3.3 days | 5-19 months | 1.7% |
| Present study | Retrospective chart review | 248 | 8.5% | 27.50 minutes | 2.275 days | 2 years - 7 years | 6.5% |
Among short-term complications, wound morbidity in the form of seroma, skin necrosis, and wound infection have been the major hurdles in the use of mesh for small ventral hernias. Present study showed a wound infection rate in 8.5% and skin necrosis in 2.4%. A total of 10.9% of patients went on to develop a seroma. Similar studies in literature were retrospective studies with poor documentation of seroma formation, skin necrosis or haematoma formation. Most of the studies have documented surgical site infection ranges from 2-8% [12-17]. In the present study wound infection rate and other local complications were slightly higher compare to available literature. However, none of these wound complications lead to reoperation or mesh exit. In general wound infection rate for open repair was 23.4% and 4.4% for laparoscopic repair in ventral hernias [11,18]. In present study wound infection rate was between these values, however they are not comparable because of heterogenity of patients. Present study is the first of its kind to extensively document clinical data regarding Ventral Patch use from the sub-continent of India. The observed recurrence rate of 6.5% (Median follow-up 54 months) reported in present study is comparable to that reported by the regional cohort study from the Danish Hernia Database (up to 10%) over 43 months [19]. Similar studies with ventralex patch or other patch repairs showed recurrence rate varies from 2% to 14.8% comparable to present study results [12-15].
As described in the procedure, this technique uses a smaller incision compared to the traditional open approach because creation of a subcutaneous or pre-peritoneal plane for mesh placement is unnecessary. Ventral hernia repair using open or laparoscopic technique the average operation time varies between 100-110 minutes [18]. The average operation time for this procedure varies from 15 minutes to 45 minutes. However, hernias with defects of more than 4 cm or divarication of recti ideally cannot be repaired using this technique.
The average duration of operation in present study was 27.50 minutes which is shorter or comparable to similar studies with ventral patch repair [12-17]. Average length of hospital stay for ventral hernias in literature is three days for laparoscopic repair and five days for open repair. The mean duration of hospital stay in present study was 2.275 days. Similar studies with patch repair showed median hospital stay of 2-3.3 days [12,13,15-17]. Some studies have done these operations as day care surgeries with a median hospital stay of one day [12,16]. Thirty percent of present study operations were done as day-care procedures with 8 hours’ hospital stay.
The cost analysis of this technique revealed an average cost of INR 35,142/- from 248 patients. Thirty patients each who underwent laparoscopic and traditional open sublay mesh repair under the same unit were randomly selected from the hospital electronic database for cost-analysis from the time of admission to discharge. This revealed an average cost of INR 88,601/- for laparoscopic repair (including disposables) and INR 30,174/- for open regular sub-lay repair. In literature, laparoscopic repair is associated with increased disposable costs and hospital expenditure compared to open repair [20]. But overall healthcare expenditure was comparable to open repair because of short hospital stay and early return to normal life [20,21]. The use of the Ventralex Patch has the advantage of shorter hospital stay and early return to normal life with less disposable cost thus reducing the overall hospital expenditure further. In the present study short and long-term complications were comparable to several studies where similar mesh patches used [12-17]. Duration of operation, hospital stay was also comparable to similar studies and less than conventional open or laparoscopic techniques [12-17].
Limitation(s)
The follow-up was 100%, it was a telephonic conversation rather than having a clinical or radiological examination for recurrence.
Conclusion(s)
Ventralex patch repair is very efficient and effective in the treatment of selective umbilical, periumbilical, epigastric, and incisional hernias with a comparable complication profile in terms of short term complications and recurrence rate compared to available literature.
Authors would have like to conduct this study as a randomised controlled trial by assigning the patients either the hernia patch open sub lay mesh repair, or laparoscopic mesh repair.