Zirconia is considered as an alternative material for the fabrication of implants. The ratio of patients opting for a metal free treatment is constantly increasing. Despite significant advancements in surface modification techniques, Bone Implant Contact (BIC) is far below ideal 100 percentage. Surface roughness is a double-edged weapon in dental implants. Literature shows that surface roughness within 1-1.5 nm is secret factor behind bioactive implants [1]. Textured implant surface exhibits more surface area for integrating with bone. But successful and feasible technique to obtain micro-roughened surface especially in commercially available zirconia implants is still challengeable.
Materials and Methods
The present study was an in-vitro study and its purpose was to observe the surface changes on zirconia implants after UV treatment. Since this was an in-vitro study and no animals and humans were involved in the study, the ethical clearance was not obtained. It was conducted over a period of six months (March 2020 to August 2020) at Central Electrochemical Research Institute, Karaikudi, Tamil Nadu.
Since the study is first of its kind, on an experimental basis, based on simple random sampling, ten commercially machined one-piece Zirconia implant (white sky implant system-Bredent company) was used to evaluate the surface topography [Table/Fig-1], five each in study and control group. The implants were all received in their original sterile packaging and were opened only at the start of the study. They were carefully handled in order to prevent contamination during further manipulation. Damaged implants and implants with faulty sterile packing were excluded.
Commercially available single piece zirconia implants.

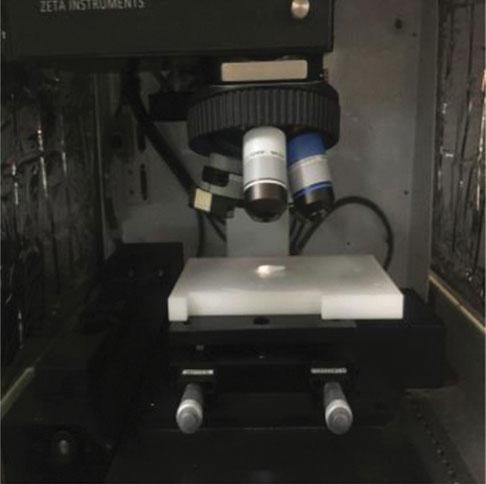
Study group was surface treated by UV radiation [Table/Fig-2] for 48 hours with following parameters- UV activation device with 15W bactericidal lamp; intensity 2 mW/cm2 and shorter wavelength of 254 nm [Table/Fig-3]. Microanalysis of the samples was done at three different regions (abutment, thread and crest) by optical profilometry [Table/Fig-4]. For a direct comparison same magnification (5x) was used at all investigation sites [Table/Fig-5]. A box was marked on the implant sample to ensure topographical measurements on the same spot.
UV chamber used for Photofunctionalization.

Provision in the UV chamber for choosing shorter wavelength.

Optical profilometry instrument.

Zirconia implants on 3D optical profilometry.
Statistical Analysis
Data was analysed for descriptive and inferential statistics using SPSS version 20.0. The statistical test applied was independent t-test which compared the mean of two groups. A p-value less than 0.05 was considered statistically significant.
Results
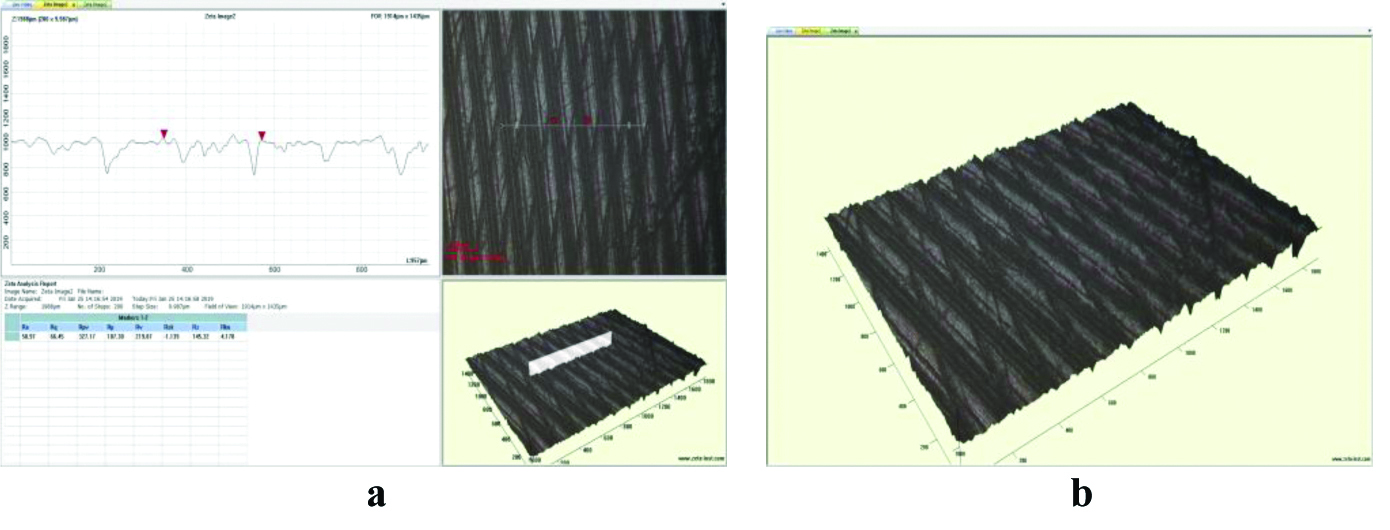
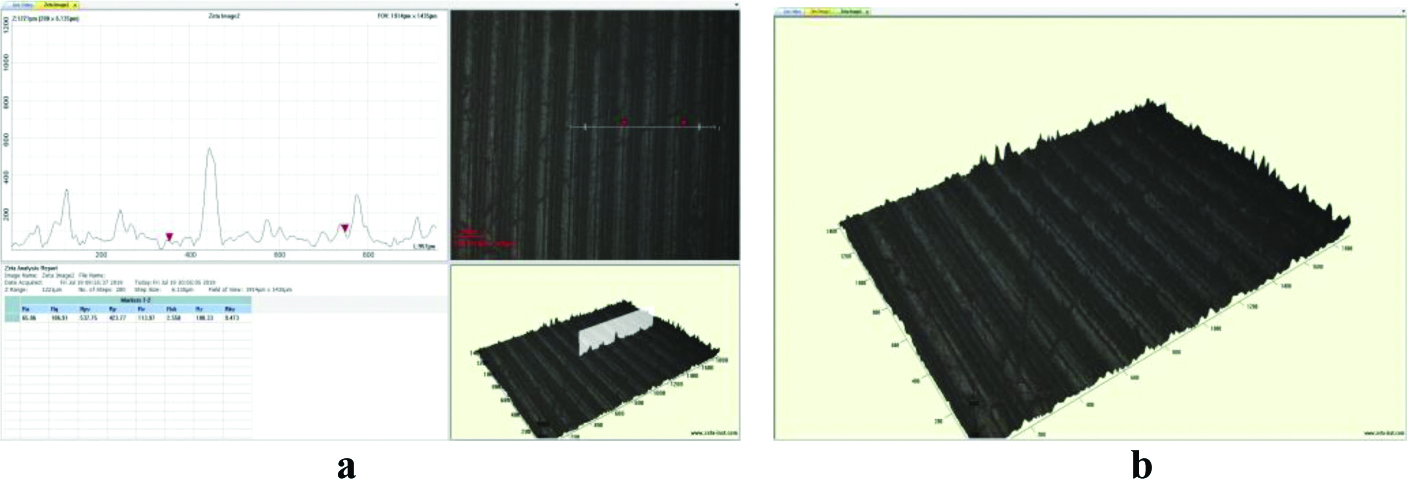
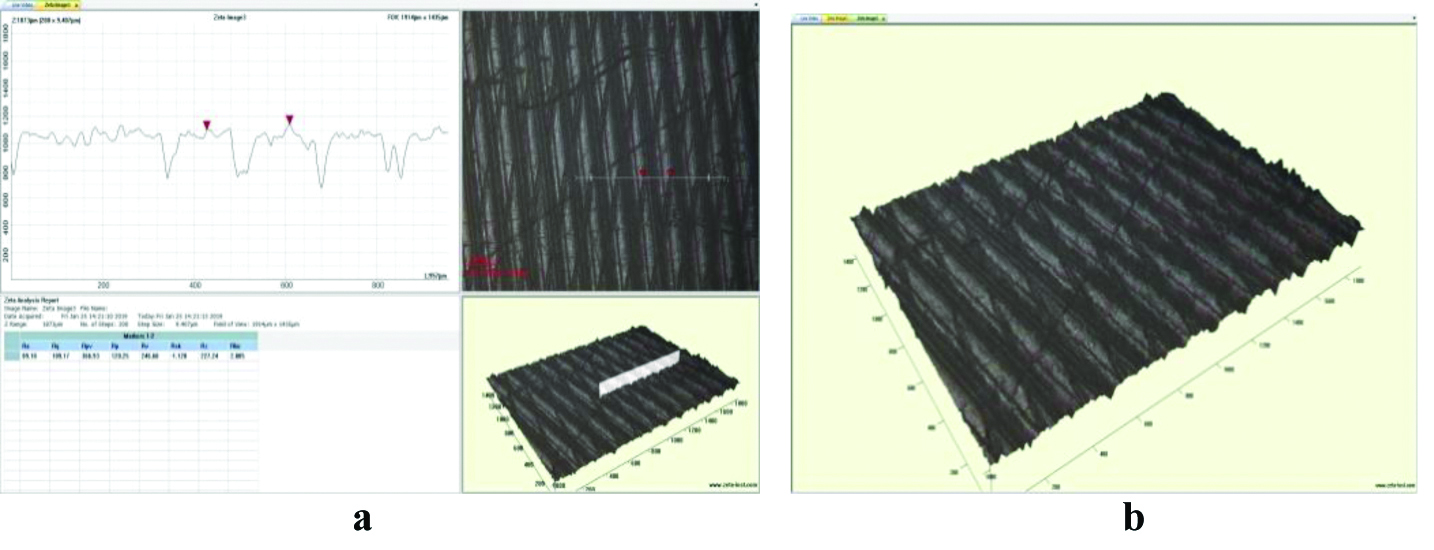
Scanning micrographs of the study and control group revealed significant difference in micro topography. Photofunctionalized group surfaces in all three regions (abutment, thread and crest) varied by the presence of distinct protrusions with highest number of peaks per unit and highest density of summits contributing to increased surface area. In contrast, control group had comparatively smooth surface texture [Table/Fig-6,7,8,9,10 and 11].
a) A 2D topography and graphical representation of the roughness profile of implant of control group abutment at (5X) magnification; b) A 3D topography image.
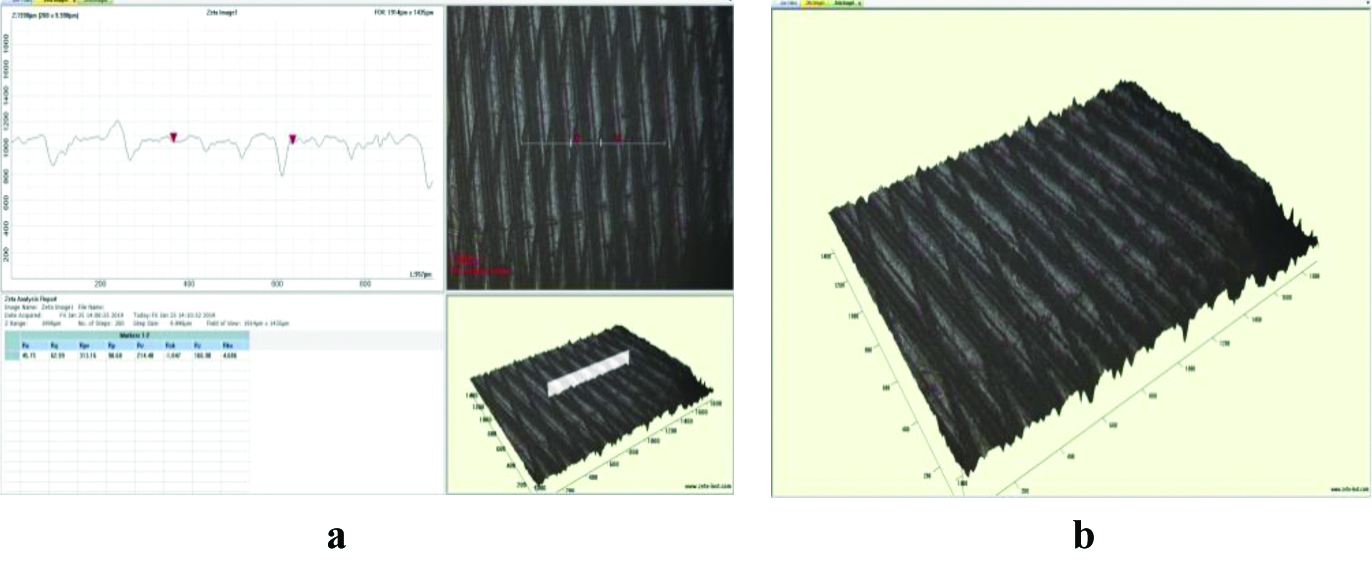
a) A 2D topography and graphical representation of the roughness profile of implant of study group abutment at (5X) magnification; b) A 3D topography image.
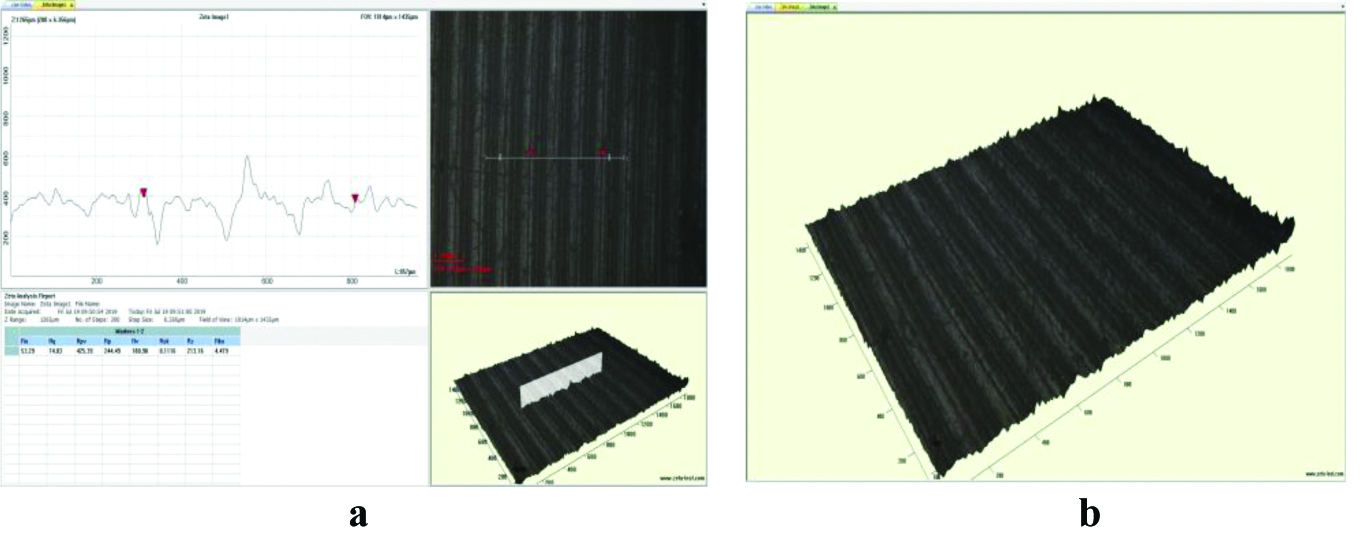
a) A 2D topography and graphical representation of the roughness profile of implant of control group crest at (5X) magnification; b) A 3D topography image.
a) A 2D topography and graphical representation of the roughness profile of implant of study group crest abutment at (5X) magnification; b) A 3D topography image.
a) A 2D topography and graphical representation of the roughness profile of implant of control group thread at (5X) magnification; b) A 3D topography image.
a) A 2D topography and graphical representation of the roughness profile of implant of study group thread at (5X) magnification; b) A 3D topography image.
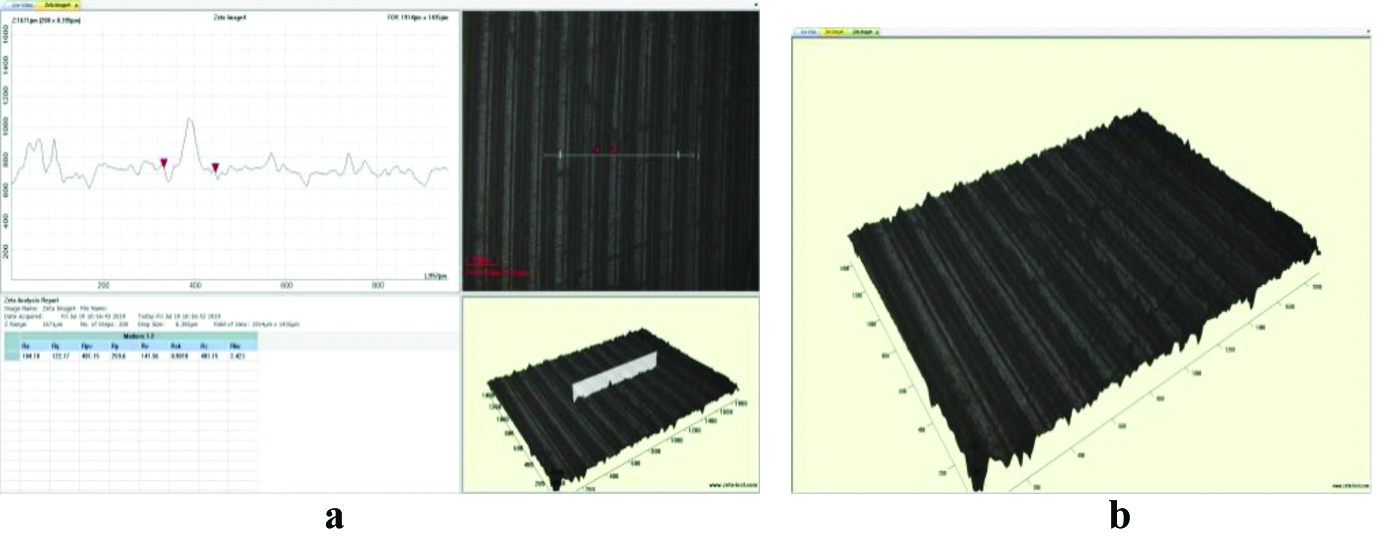
Quantitative analysis of surface roughness amplitude parameters: Ra (arithmetic mean deviation), Rq (root mean square roughness), Rz (height over the complete surface), Rp (maximum profile peak height), Rv (Maximum profile valley depth), Rsk (skewness) and Rku (kurtosis), Rpv (distance between the maximum peak height and maximum valley depth), measured for both study group and control group showed statistically significant higher mean roughness parameter for photofunctionalized implants in abutment, crest and thread region (p<0.05) [Table/Fig-12,13 and 14]. This clearly indicates that the zirconia implants have undergone significant changes after UV treatment on the above mentioned parameters.
Comparison of roughness parameters of study and control group at 5x magnification in the abutment region.
| UV treated ZR implants Mean±SD | ZR implants Mean±SD | Mean difference | ‘t’ ratio | p-value |
|---|
| Ra | 53.29±4.29 | 45.75±4.38 | 7.54±3.76 | 5.57 | <0.002* |
| Rq | 74.03±4.21 | 62.99±2.48 | 11.04±6.45 | 4.76 | <0.004* |
| Rpv | 434.39±3.21 | 313.16±9.59 | 121.234±11.21 | 30.06 | <0.0001* |
| Rp | 244.49±12.96 | 98.68±6.62 | 145.81±6.42 | 63.14 | <0.0001* |
| Rv | 189.90±8.63 | 214.48±8.68 | 24.58±1.22 | 55.88 | <0.0001* |
| Rsk | 0.1116±.01 | -1.047±0.02 | 1.1586±0.03 | 85.12 | <0.0001* |
| Rz | 213.16±9.07 | 166.90±6.45 | 46.264±15.43 | 8.33 | <0.0005* |
| Rku | 4.479±0.81 | 4.686±0.08 | 0.207±0.81 | 0.71 | <0.02* |
p-value <0.05 is statistically significant; ZR: Zirconia
Ra=arithmetic mean deviation, Rq=root mean square roughness, Rz=height over the complete surface, Rp=maximum profile peak height, Rv=Maximum profile valley depth, Rsk=skewness and Rku=kurtosis, Rpv=distance between the maximum peak height and maximum valley depth
Comparison of roughenss parameters of study and control group at 5x magnification in the crest region.
| UV treated ZR implants Mean±SD | ZR implants Mean±SD | Mean difference | ‘t’ ratio | p-value |
|---|
| Ra | 65.86±6.86 | 50.97±3.33 | 14.89±4.06 | 10.2 | <0.002* |
| Rq | 106.91±7.03 | 66.45±7.21 | 40.46±4.43 | 25.34 | <0.0001* |
| Rpv | 537.75±9.51 | 327.17±6.51 | 210.58±3.97 | 147.21 | <0.0001* |
| Rp | 423.77±3.96 | 107.30±4.57 | 316.47±0.78 | 1114.09 | <0.0001* |
| Rv | 113.97±2.18 | 219.87±3.58 | 105.9±1.41 | 207.81 | <0.0001* |
| Rsk | 2.588±0.12 | -1.139±0.03 | 3.727±0.10 | 78.58 | <0.0001* |
| Rz | 188.33±3.01 | 145.32±1.51 | 43.01±2.97 | 35.41 | <0.0001* |
| Rku | 9.473±0.59 | 4.178±0.49 | 5.2948±0.63 | 19.15 | <0.0001* |
*p-value <0.05 is statistically significant
Comparison of roughenss parameters of study and control group at 5x magnification in the thread region.
| UV treated ZR implants Mean±SD | ZR implants Mean±SD | Mean difference | ‘t’ ratio | p-value |
|---|
| Ra | 104.18±3.81 | 89.10±1.99 | 15.08±1.91 | 21.91 | <0.002* |
| Rq | 122.774±4.38 | 109.17±4.41 | 13.604±0.50 | 75.45 | <0.0001* |
| Rpv | 401.15±6.04 | 366.93±5.38 | 34.22±6.72 | 11.75 | <0.0001* |
| Rp | 259.6±4.09 | 120.25±3.10 | 139.35±4.27 | 75.32 | <0.0001* |
| Rv | 141.56±3.63 | 246.68±3.52 | 105.116±0.72 | 404.24 | <0.0001* |
| Rsk | 0.901±0.00 | -1.128±0.00 | 2.029±0.00 | 627.9 | <0.0001* |
| Rz | 401.15±3.78 | 227.24±2.44 | 173.91±1.5345 | 315.06 | <0.0001* |
| Rku | 2.423±0.17 | 2.805±0.60 | 0.382±0.4558 | 2.32 | <0.004* |
*p-value <0.05 is statistically significant
Discussion
Various surface modification techniques were used on zirconia based bioceramics with a goal to enhance peri-implant osteogenesis. Numerous studies have shown micro roughened implant surfaces showed an increased percentage of bone-to implant contact and require higher forces to break implant bone anchorage than implants with smooth surfaces [11-13].
A moderately roughened microscale topography has been shown to be a critical feature in the successful osseointegration of implant materials [14-17]. Hence, achieving textured implant with various techniques is a fast-growing area of interest.
Identifying nano topographical technique with potential synergistic effects in producing biocompatible zirconia implant remains a challenge till date. Few studies suggest photofunctionalization (Ultraviolet radiation) is feasible as well as efficient surface treatment in rendering bioactive zirconia implants without compromising their physicochemical property [18-20].
Furthermore, correlation approaches using different techniques can expand the analytical capability in creating ideal implant. Optical profilometry enables resolution of sample to few nanometers. The advantages of using 3D Optical profilometry is its good resolution, high speed, reliability (cannot be damaged by surface wear or careless operator), and can be used in all kind of surfaces (Rough and smooth) [20]. Therefore, this research was done to assess the values of surface roughness parameters obtained by 3D optical profilometry, on zirconia implants after photofunctionalization (UV treatment).
In this study, topography of sample area was measured using 2D/3D scanning and surface roughness was calculated using amplitude parameter. Scanning micrographs depicted homogeneously roughened surface in UV treated group in all three regions. This is a favourable factor as sharp, deep internal line angles increases stress concentration. As zirconia is brittle stress concentration especially in thread area has to be avoided.
‘Ra’ parameter is most frequently used roughness parameter for a dental implant surface. In the present study Ra values of UV treated zirconia implants showed higher mean Ra values in all three regions, more pronounced in the rough surface (thread and crest) compared to the smooth surface (abutment). Hence, UV radiation has certainly roughened the zirconia implant surface akin to studies reported earlier [13].
Other favourable surface parameters like ‘Mean Rq, Rz Rpv, Rp, Rsk, Rz’ showed increased values in study group whereas Rv (Maximum profile valley depth) and Rku (kurtosis) decreased indicating UV photofunctionalization has certainly and uniformly roughened the zirconia implant surfaces. Higher Rp and reduced Rv value indicates appropriate friction and decreased wear respectively. Increased Rz is a measure of reduced odd scratches or irregularities. The Rku >3 denote uniformly roughned surface [13].
Rsk illustrates load carrying capacity, porosity, and characteristics of non conventional machining processes. Surfaces that are smooth but are covered with particulates have positive skewness, while a surface with deep scratches/pits will exhibit negative skewness. Skewness is very sensitive to outliers in the surface data [13]. Hence, increased Rsk in study group demonstrate photofunctionlisation converted negative Rsk to positive thereby increasing load carrying capacity and decreasing the porosity. This study provides an insight for further advancing long term clinical trials to substantiate role of photofunctionlisation and its degree of osseointegration.
Limitation(s)
Limitation of using this 3D optical profilometer in this study is that, its use is limited in the thread portion of the implant, where the slopes are very high, so the light gets reflected away from the objective, unless the slope has enough texture to provide the light. Considering the fact that this study was first of its kind, and the use of zirconia implants in replacement of tooth is still in the early stages, the sample size selected for this study was small and further studies with a large sample size needs to be conducted.
Conclusion(s)
Within limits of the study, photofunctionalization showed its ability to increase the microroughness on Zirconia implants without compromising their desirable physiochemical property. Hence, UV treatment is a potentially synergistic technique in producing biocompatible Zirconia implants.
p-value <0.05 is statistically significant; ZR: Zirconia
Ra=arithmetic mean deviation, Rq=root mean square roughness, Rz=height over the complete surface, Rp=maximum profile peak height, Rv=Maximum profile valley depth, Rsk=skewness and Rku=kurtosis, Rpv=distance between the maximum peak height and maximum valley depth
*p-value <0.05 is statistically significant
*p-value <0.05 is statistically significant