Clinical Spectrum of Corneal Epithelial Microsporidiosis
Prabhakar Singh1, Abhishek Gupta2, Richa Gupta3
1 Cornea and Anterior Segment Consultant, Department of Cornea and Anterior Segment, Nirwana Netralaya, Sasaram, Bihar, India.
2 Senior Resident, Department of Retina Services, IGIMS, Patna, Bihar, India.
3 Senior Resident, Department of Pediatric Services, IGIMS, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Prabhakar Singh, Awadh Vatika, Satanpur Bokaro Steel City, Jharkhand, India.
E-mail: prabhakar1aiims@gmail.com
This case series aims to highlight three different clinical variants of microbiologically proven epithelial microsporidiosis, and their customised management wherein the current series, patients with suspected epithelial microsporidiosis were subjected to corneal scraping to confirm the diagnosis. Different microbiologically proven clinical variants were observed and documented. Three clinical variants of epithelial microsporidiosis were noted. The first was of 45-years-old male patient, presented with only raised punctate lesions, and responded to topical lubricants only. The second variant, 28-years-old male patient, had anterior chamber reaction (flare and cells), Keratic Precipitates and descemets folds. This variant also responded with topical lubricants over a period of one month. The third variant, 32-years-old male patient at presentation, had typical epithelial raised punctate corneal lesions, however at one week subepithelial infiltrates appeared. These lesions responded to topical steroids. The current series highlights three different clinical variants of microbiologically proven epithelial microsporidiosis and their customised management.
Clinical variants, Keratoconjunctivitis, Microsporidial keratitis, Spring water
Introduction
At the outset of rainy season a sudden upsurge in the number of microsporidial keratoconjunctivitis is seen. In absence of general awareness among Ophthalmologists regarding the various clinical manifestations either the disease is over treated or wrongly treated. This case series tries to highlight three different clinical variants of microbiologically proven epithelial microsporidiosis and their customised management.
Case Series
Case 1
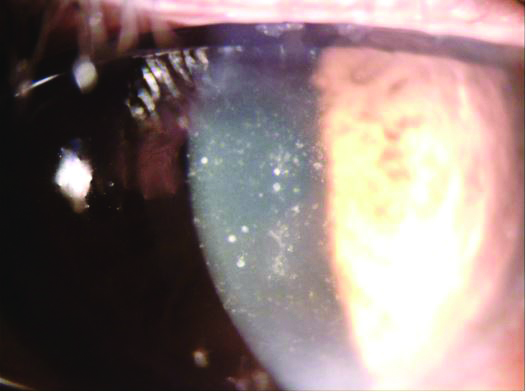
A 45-year-old male patient, presented to the Ophthalmic clinic with complaints of foreign body sensation and redness in the right eye since 10 days. He gave a history of bathing in a natural spring 10 days ago. On slit-lamp examination of the right eye, diffuse punctuate raised epithelial lesions with stuck on appearance were noted without any signs of anterior chamber inflammation [Table/Fig-1]. The corneal scraping showed microsporidial spores. The patient was started on topical lubricants (Carboxymethyl cellulose). At 1 week, the lesions had decreased significantly, however complete cure was noted at the end of 1 month.
Showing typical features of epithelial micorsporidiosis.
Case 2
A 28-year-old male patient, with complaints of redness and foreign body sensation since two days, in the right eye presented to the ophthalmic clinic. He gave a history of accidental spillage of water into the right eye while working in the field, five-day-ago. On examination of the right eye, multiple raised punctate epithelial lesions with stuck on appearance were noted along with anterior chamber reaction with flare. Decemets Membrane folds and keratic precipitates were also present [Table/Fig-2]. The corneal scraping showed microsporidial spores.
Showing presence of anterior chamber reaction, keratic precipitates and Descemets. Membrane folds in addition to typical epithelial features of epithelial microsporidiosis.
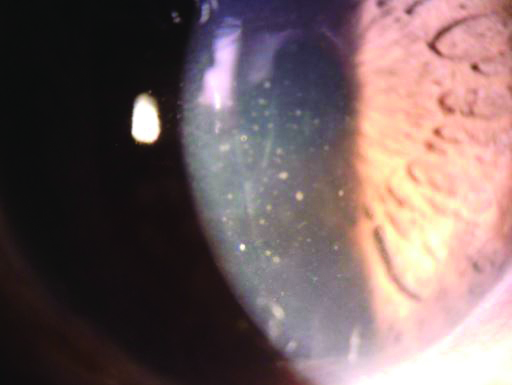
The patient was kept on topical lubricants (carboxymethyl cellulose) and reviewed at one week. At one week the keratic precipitates persisted; however, the corneal lesions and anterior chamber reaction had decreased significantly. At 1 month, the cornea cleared completely and crenated edges of old Keratic Precipitates noted in absence of any anterior chamber reaction.
Case 3
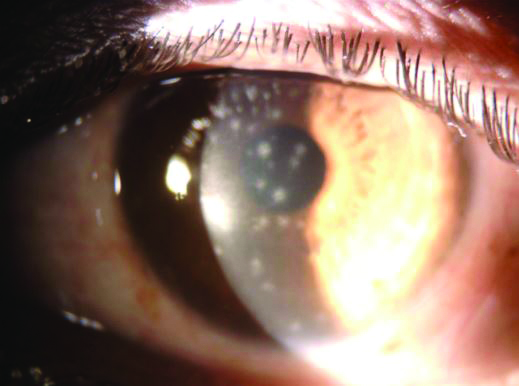
A 32-year-old male patient presented with the left eye redness and foreign body sensation since two days. He gave a history of bathing in a natural spring two days ago. On examination, typical multiple punctate raised epithelial lesions were noted. Corneal scraping showed microsporidial spores. Patient was started on topical lubricants (carboxymethyl cellulose). At one week, patient presented with multiple punctate anterior stromal infiltrates [Table/Fig-3]. The raised epithelial lesions disappeared at one week and clinically the current lesions were indistinguishable from corneal lesions in adenoviral keratoconjunctivitis. Patient was continued on topical lubricant and reviewed after three days; however, clinical worsening noted (enlargement of subepithelial infiltrates). At this visit, topical steroids (loteprednol etabonate) were started and patient was found to improve on topical steroids on subsequent visits. Patient was continued on tapering doses of topical steroids for eight weeks and then steroid was stopped. The patient recovered completely.
Showing absent raised epithelial lesions at one week, with presence of multiple punctate subepithelial to anterior stromal infiltrates.
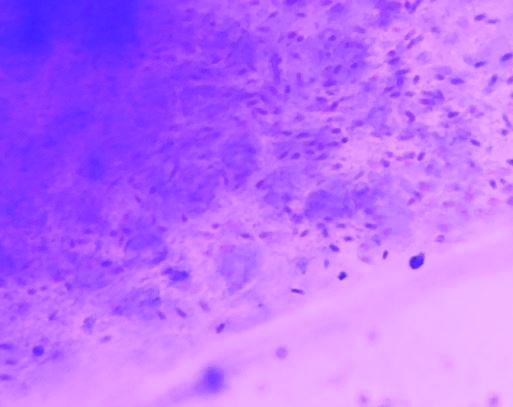
All the cases had associated papillary conjunctivitis and all cases were microbiologically proven cases of epithelial microsporidiosis [Table/Fig-4]. The number of cases of epithelial microsporidiosis peaked during rainy season when the natural springs started overflowing and with accidental spillage of water into the eye. So far 16 such cases have been recorded, however only three of these, each representing the prototype case will be discussed here.
Showing plenty of microsporidial spores in corneal scraping (Grams staining, 100x magnification).
Discussion
At the outset of rainy season, a sudden increase in the systemic infections have been noted; so is true for ocular infections also. Microsporidial infection of eye is one of those infections and natural springs often act as a reservoir [1]. The Microsporidia are known to cause keratoconjunctivitis, corneal stromal keratitis, scleritis, and endophthalmitis [2-8]. In our climatic scenario, corneal epithelial microsporidiosis is very commonly seen, though often misdiagnosed as viral keratoconjunctivitis and mistreated. The raised punctate epithelial lesions with stuck on appearance, with or without endothelial dusting are very typical of this. Adenoviral keratoconjunctivitis and Thygeson’s superficial punctate keratitis are close differential diagnoses. The microsporidial disease is often under-reported in view of lack of awareness among ophthalmologists. The thought that-microsporidial keratoconjuntivitis (epithelial) is a disease of immunocompromised, still prevails amongst the ophthalmologists. There are various studies quoting different treatment modalities including fluoroquinolones, fumagillin, albendazole, Poly Hexa Methylene Biguanide (PHMB) etc., [9]. However, previous studies clearly mentions that the disease is self-limiting and can be treated with topical lubricants only [10,11].
This case series aims to highlight three different clinical variants of microbiologically proven epithelial microsporidiosis and their customised management. The first case discussed here is very similar to the prototype epithelial microsporidiosis cases discussed in literature, which responded very well to topical lubricants [10]. The natural course of the disease discussed here does not have any intermediate steps; in contrast to case 3, where intermediate stage was noted at one week. At one week, case 3 had anterior stromal infiltrates which were similar to subepithelial infiltrates in adenoviral keratoconjunctivitis. Das S et al., in their studies have shown association of adenoviral keratoconjunctivitis and epithelial microsporidiosis [12]. The presence of subepithelial infiltrates were attributed to concomitant adenoviral infection in their study. However, the presence of subepithelial infiltrates can also be the natural course of the disease suggestive of immune mediated etiology and thusresponds to topical steroids.
Case 2 in contrast had intense anterior chamber reaction, keratic precipitates, Descemets membrane folds associated with raised epithelial punctate lesions. Observation over a period of one week on topical lubricants showed decreased severity of corneal lesions (including descemets membrane folds) with persisting keratic precipitates, so lubricants were continued. At one month the cornea became clear with presence of old keratic precipitates over endothelium.
So far literature shows evidence of only one clinical type similar to our case 1 [10]. Cases similar to case 2 and 3 have never been mentioned in literature. This case series probably paves a path for future research and well randomised studies on this.
Conclusion(s)
To conclude, corneal epithelial microsporidiosis can present with three different clinical pictures. Corneal scraping and direct microscopy at the outset help us establish the diagnosis. Though most of these respond to topical lubricants, however there is a subtype which needs topical steroids also. So, one has to customise the treatment based on the clinical features at presentation.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 18, 2020
Manual Googling: Nov 18, 2020
iThenticate Software: Apr 14, 2021 (5%)
[1]. Fan N, Wu C, Chen T, Yu W, Chen C, Lee S, Microsporidial keratitis in patients with hot springs exposureJournal of Clinical Microbiology 2012 50(2):414-18.10.1128/JCM.05007-1122116156 [Google Scholar] [CrossRef] [PubMed]
[2]. Friedberg DN, Stenson SM, Orenstein JM, Tierno PM, Charles NC, Microsporidial keratoconjunctivitis in acquired immunodeficiency syndromeArch Ophthalmol 1990 108(4):504-08.10.1001/archopht.1990.010700600520472108656 [Google Scholar] [CrossRef] [PubMed]
[3]. Metcalfe TW, Doran RM, Rowlands PL, Curry A, Lacey CJ, Microsporidial keratoconjunctivitis in a patient with AIDSBr J Ophthalmol 1992 76(3):177-78.10.1136/bjo.76.3.1771540567 [Google Scholar] [CrossRef] [PubMed]
[4]. Ashton N, Wirasinha PA, Encephalitozoonosis (nosematosis) of the corneaBr J Ophthalmol 1973 57(9):669-74.10.1136/bjo.57.9.6694202149 [Google Scholar] [CrossRef] [PubMed]
[5]. Pinnolis M, Egbert PR, Font RL, Winter FC, Nosematosis of the cornea. Case report, including electron microscopic studiesArch Ophthalmols 1981 99(6):1044-47.10.1001/archopht.1981.039300110440126786272 [Google Scholar] [CrossRef] [PubMed]
[6]. Davis RM, Font RL, Keisler MS, Shadduck JA, Corneal microsporidiosis. A case report including ultrastructural observationsOphthalmology 1990 97(7):953-57.10.1016/S0161-6420(90)38016-4 [Google Scholar] [CrossRef]
[7]. Mietz H, Franzen C, Hoppe T, Bartz-Schmidt KU, Microsporidia-induced sclerouveitis with retinal detachmentArch Ophthalmol 2002 120(6):864-65. [Google Scholar]
[8]. Yoken J, Forbes B, Maguire AM, Prenner JL, Carpentieri D, Microsporidial endophthalmitis in a patient with acute myelogenous leukemiaRetina 2002 22(1):123-25.10.1097/00006982-200202000-0002811884897 [Google Scholar] [CrossRef] [PubMed]
[9]. Loh RS, Chan CM, Ti SE, Lim L, Chan KS, Tan DT, Emerging prevalence of microsporidial keratitis in Singapore: epidemiology, clinical features, and managementOphthalmology 2009 116(12):2348-53.10.1016/j.ophtha.2009.05.00419815287 [Google Scholar] [CrossRef] [PubMed]
[10]. Joseph J, Sridhar MS, Murthy S, Sharma S, Clinical and microbiological profile of microsporidial keratoconjunctivitis in southern IndiaOphthalmology 2006 113(4):531-37.10.1016/j.ophtha.2005.10.06216488011 [Google Scholar] [CrossRef] [PubMed]
[11]. Moshirfar M, Somani SN, Shmunes KM, Espandar L, Gokhale NS, Ronquillo YC, A narrative review of microsporidial infections of the corneaOphthalmol Ther 2020 9(2):265-78.Epub 2020 Mar 1010.1007/s40123-020-00243-z32157613 [Google Scholar] [CrossRef] [PubMed]
[12]. Das S, Sahu SK, Sharma S, Nayak SS, Kar S, Clinical trial of 0.02% Polyhexamethylene biguanide versus placebo in the treatment of microsporidial keratoconjunctivitisAm J Ophthalmol 2010 150(1):110-15.10.1016/j.ajo.2010.01.03820447613 [Google Scholar] [CrossRef] [PubMed]