The COVID-19 outbreak has impacted the world in an unparalleled manner. In addition to increasing the mortality rate, it has altered the daily routines including work, education, family and leisure [1,2]. This worldwide lockdown has brought many facilities to a standstill, including rehabilitation and poses a substantial challenge to provide therapeutic services. For instance, the provisions of speech and language therapy to the children with communication difficulties are paused due to the necessity of face-to-face interaction between the therapists and the children [3].
Children with various communication disorders such as Language Developmental Disorders, Stuttering, Cleft Lip and Palate, Learning Disorder, Autism, and Hearing Loss, face chronic problems that negatively impact the social, physical, economic, and the psychological state of the family. This has been aggravated due to the pandemic situation and calls for immediate attention to the children with needs [4]. The hardships are doubled in case of the parents of children with HI or these children with co-morbid conditions such as Autism Spectrum Disorders (ASD), Multiple Disabilities, who find it difficult to adapt to this sudden change, as they are so used to the pattern and services that they were hitherto provided, which might also increase the chances of developing anxiety/behavioural issues [5].
In order to cope with communication delays, auditory, speech, and language therapies are highly crucial after the fitting or surgical implantation of the hearing device. Any lack of auditory stimulation after being aided with hearing aids/implantable devices, can result in reduced quality of life and academic performances [6]. Reading and writing skills might also be lagged due to these communication delays [7]. Therefore, it is critical to emphasise on an uninterrupted auditory bombardment, apposite care and maintenance, and Auditory Verbal Therapy (AVT) for the attainment of successful speech and language milestones.
Due to these unexpected turns of events, new modes of service delivery and professional assistances are expected by the parents. The inability to access rehabilitation services due to transportation suspension, acts as a huge drawback to the patients who live in remote areas and outskirts of the city [4]. Hence, the best choice to bridge the uninterrupted therapeutic services during a pandemic is via telepractice.
Telepractice are the telecommunications technological application to the delivery of Speech-Language Pathologist (SLP) and audiology services at a distance by linking clinician to clinician or clinician to patient for consultation, assessment and intervention [8]. Telepractice is an innovative and easily implementable solution to overcome the above-mentioned problems and its primary aim is to provide services for clients in different geographical areas who have limited access and to those who have motor coordination problems [1]. Although telepractice is renowned worldwide, it is still inaccessible due to various factors such as unawareness, limited access to telecommunication devices, financial limitations, poor network coverage, and the child’s limitations such as their disability, etc.
Correspondingly, to provide a solution, the Speech and Language services were resumed at our institution in April 2020 via the telecommunication mode during this period. While trying to implement the services to all the children with HI, various difficulties were faced by the parents in enrolling their child into telepractice.
Therefore, to have a better perspective of the limitations and provide appropriate solutions during lockdown, the aim of the present study is to briefly discuss three main domains which include: (i) Communication challenges faced by children with HI; (ii) Effectiveness and need for Telepractice; and (iii) Means to improve the service delivery.
Materials and Methods
A cross-sectional descriptive study was conducted in MERF Institute of Speech and Hearing, Chennai from July 2020 to August 2020. A convenience sampling was opted for enrolling the participants in the study. The parents of Hearing Impaired children, who were already availing rehabilitation services, were targeted to obtain their perspectives.
A self-rating questionnaire was self-made. The questions were framed based on few challenges faced by respondents as they informally reported. To address the parental perspective, the questionnaire was developed in English as most of the parents were literate to understand the language. The questionnaire consisted of close-ended questions, with appropriate open-ended sub-divisions that were grouped into five sections. Section A contained four questions regarding demographic details, Section B contained three questions on brief history of hearing loss and the management option, Section C contained seven questions based on Postimplant rehabilitation workup, Section D contained ten questions based on communication challenges during lockdown and Section E contained 1 question based on a service delivery model awareness and grouped into two parts: Part A has ten questions- for 10 children who received telepractice services and Part B has two questions-for 30 children who did not receive telepractice services [Annexure].
Inclusion and Exclusion criteria: An inclusion criterion incorporates parents of both pre-lingual and postlingual children with HI (with and without co-morbid conditions). Children belonged to the age group of 1 year 10 months to 17 years, who were intervened with unilateral or bilateral hearing devices and begun to receive Aural Rehabilitation services. This included a total of 40 parents (40 children) who participated in the survey. Parents of Hearing Impaired children who were intervened with sign language, speech reading, or total communication were excluded.
The questionnaire was content validated by seven experienced Audiologists and Speech-Language Pathologists (SLP) to rate the importance of each question using a likert scale. Options included were ‘very important, important, moderately important, slightly important and unimportant.’ A qualitative analysis and frequency count was done for all the responses. Questions that received ‘very important’ and ‘important’ options for more that 50% of the validators were included in the questionnaire. Their comments and suggestions were incorporated for the same.
Before administration, the purpose and duration of the survey were briefed to the parents of the Hearing Impaired children and informed consent was obtained with an assurance that the responses will remain anonymous. The data collection began by two modalities an interview method via a telephonic survey for four participants. The interviewers were cautious in interacting with the parents considering the psychological impact created by the pandemic. For 36 participants, an alternative method via the electronic format was also followed. Parents were posted the link to the questionnaire and were asked to fill up the responses.
Statistical Analysis
Answers from all the sections were observed and categorised. Frequency count was done for all the questions. Percentages were calculated for major and minor responses using Microsoft office Excel 2010.
Results
Mean age of 40 children (22 male and 18 female) was 5.34 years. Out of 40 responses obtained, the onset of hearing loss for 37 (92.5%) subjects has been congenital. Among them, 35 (87.5%) had been diagnosed before three years of age. These children have been using different hearing devices among which 35 (87.5%) were Cochlear Implantees, 4 (10%) were auditory brainstem implantees and 2.5 % (1/40) used bone conduction hearing aids.
Postimplant Rehabilitation Workup
Out of 40 children, 16 (40%) of participants were able to reach the clinics during lockdown for mapping, while the other 24 (60%) of implantees had been mapped only before the stay-at-home orders. Similar data were obtained for Aided Audiogram testing. Before the stay home orders were issued, 25 (62.5%) of children were already mainstreamed (attending regular school), while 15 (37.5%) of them were not, due to delayed intervention. If the child was already attending regular school, the respective parents were questioned if their children were attending the online classes. It was found that 9 (36%) were attending the online classes wherein 6 (66.7%) of them faced difficulties and 7 (77.7%) felt that their child can do better with the help of a SLP. Out of total, 24 (60%) of the children attended the AVT sessions regularly, and 33 (82.5%) frequently attended two sessions per week. Other than that, the prognosis of auditory rehabilitation sessions was also documented and it was noted that 19 (47.5%) felt the improvement seen was ‘good’ while the majority were quite satisfied.
Impact of Lockdown on Communication Abilities
To assess the effects of lockdown on communicational developments, the following factors were considered:
a) Hearing Device-based problems
b) Speech and Language performance variability
c) Home training methods
Total of 22 (55%) of our respondents did not report functional or structural device failure, but one respondent among them reported that the delivery of their serviced device was delayed due to errant transportation conditions. And the rest, 18 (45%) of the participants had trouble shooting and other issues that are listed in [Table/Fig-1].
Device related problems faced by the participants (n=18).
| Device related problems | Number of participants |
|---|
| Limited or no access to the rehabilitation center to fix the device | 4 |
| Reduced the output from the device | 2 |
| Exhaustion of batteries | 3 |
| Transmitting cable breakage | 5 |
| Connecting pin breakage | 2 |
| Device malfunctioning (unaware of details) | 2 |
Secondly, regarding the child’s Speech and Language performance during the lockdown, 26 (65%) of parents reported that their child’s performance has not deteriorated. Among which 12 (46%) of parents responded no significant difference and 14 (54%) reported betterment during the lockdown. While others, 14 (35%) reported a significant reduction. The reasons are tabulated below in [Table/Fig-2]. About 37 (92.5%) of the parents were able to provide home training, unlike 3 (7.5%) of them who were unable to provide on a regular basis due to time constraints.
Differences in Speech and Language performance accounted before and after lockdown commencement (n=28).
| Speech and language performance | Reasons | Number of participants (%) |
|---|
| Better during lockdown-14 (35%) | Intensive home training and adequate stimulation | 12 (85.7%) |
| Communicative intent of the child | 1 (7.1%) |
| Arranged therapy sessions via telepractice | 1 (7.1%) |
| Worsened during lockdown-14 (35%) | No speech and language stimulation from a structured therapy setting | 5 (35.7%) |
| Reduced home training and stimulation | 3 (21.4%) |
| Behavioural issues due to the sudden change of the pattern in routine | 1 (7.1%) |
| Reduced device usage due to external device failure (Battery exhaustion issues, Connecting cable failure) | 4 (28.5%) |
| Device unavailability (given for Troubleshooting) | 1 (7.1%) |
To probe further along the lines of reasons behind the reduced performance, the dependence on external cues (speaker: speech reading and environment-related: azimuth and distance of the sound source) and non verbal communication methods before and after the lockdown was enquired about, using a closed-ended option of yes/no. The response elicited is given in the [Table/Fig-3].
Dependency on cues before and after lockdown commencement. Number of participants (n=40).
| Comparison before and after lockdown commencement | Number of participants (%) |
|---|
| Yes | No |
|---|
| Dependence more on non verbal communication instead of verbal means | 13 (32.5%) | 27 (67.5%) |
| Dependence more on external cues | 14 (35%) | 26 (65%) |
Thirdly, with respect to the duration of home training, the responses were recorded on a close-ended checklist format. A larger number employed incidental teaching and a few resorted to scheduled home training for 30-60 minutes. Concerning the materials required, 65% (26/40) of respondents have sufficient home training materials to carry out the home training activities while the others had no availability. Also, a majority of the parents use language stimulation techniques and training materials to provide the home training rather than using online games and videos to teach their children.
Throwing light on the need for therapeutic services and its accessibility, this study reveals that though 70% (28/40) of the parents wanted therapy during this lockdown, only 12 (42.9%) of parents approached their SLP.
Service Delivery Model
The awareness of telepractice services for Speech and Language among Indian parents was found to be 23 (57.5%) while 17 (42.5%) of parents were unaware. A follow-up question was asked to those who were aware of the teletherapy services as to whether their child was attending telepractice. Out of 23, 10 (43.5%) of participants were currently enrolled in speech and language telepractice sessions and 13 (56.5%) were not enrolled despite being aware.
Subsections of the service modality A and B were divided for those enrolled in telepractice sessions and those who were not enrolled, respectively.
Part A: With an accelerated application of teletherapy to these hearing impaired children, authors wanted to document the prevalence and effectiveness of Telepractice services. Out of 10, 1 (10%) reported that they received telepractice sessions for 4 weeks, 3 (30%) received for 3 weeks, 4 (40%) received for 2 weeks and 2 (20%) received for 1 week. They added that they were continuing the services at the time of the survey and were willing to continue in the future. This provides an inference that the implementations of these facilities prove to be beneficial.
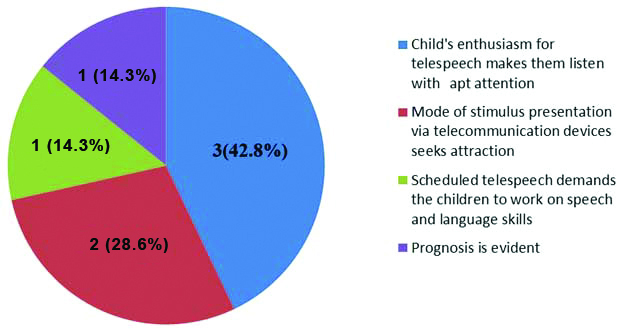
Concerning the frequency of practice, a distributed plan of practice was outlined. A majority of them had 2 sessions per week for 8 (80%) and 2 (20%) had 3 sessions/week. On further questioning, 2 (20%) suggested more sessions per week. Keeping in mind the children’s exposure to screen time, the duration of telepractice was tailored according to the attention span of the child. It ranged from 40-60 minutes for 3 (30%), 30-40 minutes for 5 (50%) and 20-30 minutes for 2 (20%). This duration can be altered according to the child and the parent’s needs. With additional probing, out of 10, it was revealed that the attention span for 6 (60%) of the children was adequate to concentrate for one full session unlike 4 (40%) of them who were unable to concentrate. Besides that, 6 (60%) of the children were eager to attend the sessions, 3 (30%) were willing at times and 1 (10%) did not look forward at all. Some of the reasons for the findings included- interrupted classes and preoccupation with leisure activities which made them uncooperative, during the extensive lockdown period. The satisfaction of the services provided was recorded, and it was discovered that 7 (70%) found it to be effective. Some of the open-ended follow-up reasons are represented in the [Table/Fig-4].
Reasons for satisfaction of the services- Number of participants (n=7).
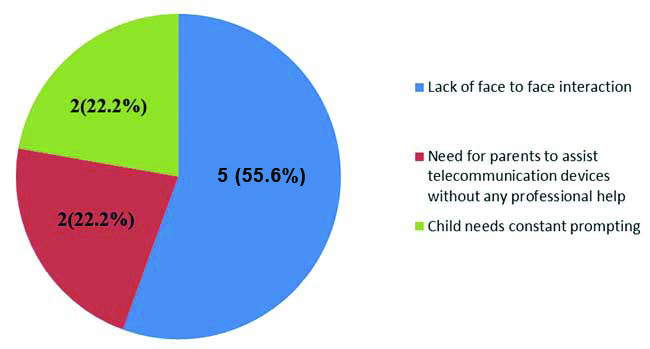
On the contrary, 3 (30%) of respondents were not satisfied and found it to be ineffective due to the child’s limitation such as inadequate attention span, sitting tolerance, and inability to understand. Although, all of them 10 (100%) were willing to avail the sessions continuously. Along the line of differences between parent’s participation and contribution during telepractice and face-to-face therapy, 9 (90%) of them faced differences and the reasons are listed in the [Table/Fig-5].
Reasons for differences in parents’ contribution during Telepractice and face-to-face therapy-Number of participants (n=9).
Finally, an open-ended question was posed to receive suggestions for improving the quality of online services provided by the therapist. Six (60%) of the participants’ had few suggestions and the recommendations were to increase in the number of sessions per week, addition of more colorful and attractive visualisation, and provision of activities for home-training.
Part B: This section included questions for the hearing impaired children who were not receiving telepractice facilities.
Initially, the parents were reviewed regarding telepractice services and asked if they wanted to receive the sessions from the speech therapist via online platform. Out of 30, 18 (60%) of them opted to attend after having few trials and got enrolled in the sessions. The other 12 (40%) did not want to/unable to attend telepractice due to personal reasons. Some of the other prominent reasons are included in the [Table/Fig-6].
Reported reasons for not opting teletherapy, number of participants (N=12).
| Reasons for not opting Tele-therapy | Number of participants (%) |
|---|
| Limited access to the telecommunication devices | 4 (33.3%) |
| Child’s limitation | 2 (16.6%) |
| Poor network coverage | 1 (8.3%) |
| Hearing device malfunctions | 2 (16.6%) |
| Unavailability of the parents | 1 (8.3%) |
| Unfamiliarity with telecommunication device usage | 1 (8.3%) |
| Sufficiency of home plan | 1 (8.3%) |
These respondents who were unwilling to attend telepractice were given the liberty to choose from other services such as aiding them with therapy materials, home training plans, and weekly monitoring through telephonic conversation. These responses were taken on a checklist format.
Discussion
Brief history of hearing loss and management option: Most of the hearing impaired children included in present study were implanted after early detection. Given that early intervention has begun, the necessity to provide intensive and continuous Speech and Language stimulation is also acknowledged.
Postimplant rehabilitation workup: One of the main goals postimplant is to mainstream children in inclusive schools. In our study, majority of the children were already mainstreamed due to early implantation. Attending regular schools requires good communication skills and abilities which denotes the effectiveness of AVT programs. The regularity of the child to the therapy sessions was checked. This was inquired based on the premise that regular sessions ensure better auditory skills and development and that the impact due to changed circumstances will be minimal. Also parents felt that AVT was benefitting their children in a large scale. This finding has also been supported by Chatterjee N et al., who quoted the comparison of the rating given by the parents before and after enrolling their children in the AVT program. Overall the speech and hearing improvement was good with a mean value of 8.06 post-therapeutically [9]. Since schools have converted their learning to virtual spaces, it is assumed that familiarity induced by them will also benefit telepractice, which is one of our main aims in this study.
Impact of lockdown on communication abilities: Majority of the children’s communication abilities were greatly affected due to device based problems. Most of respondents experienced problems with failure of device and troubleshooting. Almost half of the population (45%) faced some kind of problem with their devices and required troubleshooting assistance. Such root level causes form the first level of barriers to impede auditory stimulation and communication abilities. Similarly Ayas M et al., stated that 79% of the parents felt that their child’s audition and communication skills were reduced due to malfunctioning of the device especially speech processor breakdowns. Also, they reported that 96% of parents were unable to reach out to their health care provider for AVT sessions [3]. Also, Umashankar A and Prabhu P, quoted that all device failures cannot be resolved by an Audiologist and should to be sent back to the manufacturing company to fix the problem [10].
Most of the parents felt that their child’s communication abilities were not deteriorated. Relatable reasons were similar to Ayas M et al., in 2020 findings who stated 88% of the parents felt that the pandemic has taken a toll on their psychological well-being and that a majority found the home training to be hectic. While on the other hand, 67% of them commonly observed (behavioural) changes in their children as well. Few reported inabilities to home train their children on a daily basis [3]. A parallel finding sets out to frame the financial crisis to be one of the reasons behind this psychological impact, which inturn influences their child’s communication delay, thereby, affecting the parental care [4]. However, contradictorily, another study claimed that the parent-child interaction time has increased and it has been utilised for practicing language stimulation techniques and home training activities [1].
Home training was employed by most of our respondents during the lockdown phase concerning the necessity of their child’s communication improvement. They used language stimulation techniques and training materials more than virtual learning apps or games. This further reaffirms the view that lockdown enabled additional time to train their children has proved to be beneficial. Yet, a contradictory study disclosed that a few parents were unable to home train their children due to their uncooperativeness. It stated that only 50% of the parents followed home training schedule given by their speech-language therapists [3].
Service delivery model: Telepractice during the pandemic, has been widely used for children with many communication disorders which include hearing loss [9,11]. To emphasise the prevalence of telepractice in India, Rao PK and Yashaswini R refers to the people of India as “digitally literate”. Authors also said that the platforms for telepractice are all well set, but the development and application of telepractice services are yet to have an accelerated implementation [12]. Similar outcomes were seen in this study where most of the parents were generally aware about the virtual platform.
In this study, a majority of parents of children who receive teletherapy pointed out that the lack of face-to-face interaction with the clinician as a significant change. Apart from that, studies have also reported that parents noted their child’s inability to ‘connect’ with the clinicians, making it even more difficult to build a rapport [13,14]. Besides, caregivers and parents had to provide more guidance and assistance to operate the telecommunication devices and prepare home plans, in spite of it having a positive impact on teleconsultation [1]. Nevertheless, the compromised audio and video qualities during the sessions continue to be the most challenging issue faced by both parties, severely hindering the reception [1,14].
Only a minority of parents chose not to opt for teletherapy which is similar to the Royal College of Speech and Language Therapists (RCSLT, 2020) survey done in the UK suggests that 21.1% of their patients did not have access to telepractice [15]. Main reason of parents for not giving teletherapy to their children is due to limited use of technology, financial limitations and digital illiteracy. Geographical barriers with compromised network coverage are one of the limitations quoted in the literature [4]. Researchers have documented that the patients are not very receptive to technology due to the fact that face-to-face therapy operates differently in being more direct, with a personal touch [1]. They believe that face-to-face has always been the ‘gold standard’ for all the care provided [16]. Apart from the foresaid perception, the elderly required more adaptation time to follow the guidelines with respect to the use of newer technologies [1].
The respondents unwilling to attend telepractice were given the liberty to choose from other services such as aiding them with therapy materials, home training plans, and weekly monitoring through telephonic conversation. The paramount importance in the rehabilitationist’s responsibility to contact the clients to avail uninterrupted therapy services and aid them in whichever ways possible is noted here. Especially during the pandemic, regular follow-ups and counselling via telephonic communication can come a long way in bridging gaps.
Limitation(s)
There are few limitations to this study, including a small sample size. Results were based on the subjective responses only. Moreover, face-to-face interviews might have given better insight than telephonic and electronic methods. The psychological impact created by the pandemic might have impacted the perception of the participants. A bird-eye view of communication challenges were analysed without any specific area of interest. This study did not throw light on children with HI with co-morbid conditions who have more difficulty to adapt to the tele-mode of learning. With respect to telepractice, efficacy and effectiveness of telespeech could not be tracked with much accuracy as only 10 children were enrolled for a short span of period.
Conclusion(s)
This study addresses the communication challenges faced by children with HI during the lockdown. The findings of our study suggest that the Speech and Language performances have worsened for 35%, improved for 35% and no difference has been noted for 30% during the lockdown. As improvement after the commencement of lockdown is not significantly seen, there is a need to resume the therapy services. A majority of our respondents were aware of telepractice services and the minority were briefed regarding the telepractice procedures and accepted to avail the sessions. A handful of respondents, who were unwilling, opted to choose other modalities that helped us improve our quality of services. To understand the service delivery model and the associated difficulties that restrain the child’s communication ability in situations like the pandemic, a similar study can be done with a larger population to get unbiased results. The ultimate goal is to integrate telerehabilitation services into clinical facilities. With seamless improvement in technologies, the advancements should allow easy accessibility from patient’s home.