The Shoulder Impingement Syndrome (SIS) is considered to be an umbrella term for a cluster of signs and symptoms. The common clinical presentation of a SIS patient is localised pain around shoulder complex, functional disability, painful arc sign during elevation and weakness of external rotation [1]. SIS contributes 27% of the total shoulder injuries burden [2]. Since, the shoulder stabilises the upper quadrant, so it is considered to be a cornerstone for upper limb activities. SIS particularly generates significant impairment in function, so it has to be managed at early stages.
SIS is initially classified as subacromial space stenosis that results in compression of rotator cuff structures and gradual tendon attrition with potential chance of failure. Many of the recent literature also suggest that SIS is an end result of numerous pathologies of the shoulder [3,4]. Physiotherapy intervention usually comprise multimodal interventional strategies like exercise, MT, advice and patient education [3-5]. The goal of MT combined with TEs to accelerate reduction of pain, promote healing, restores pain free ROM and increase rotator cuff strength. Scapular exercises have also been reported to increase the activity of the middle trapezius, lower trapezius and serratus anterior muscles [6-8].
Manual Therapy (MT) or joint mobilisation is defined as skilled passive movement with therapeutic intent [8]. It uses low velocity, rhythmic oscillatory application applied in various grades. The mobilisation methodologies like Maitland approach are supposed to cause therapeutic effects either by structural or neurophysiological mechanisms [8].
A number of earlier published articles on conservative management of SIS have not been able to firmly come to a conclusion on the efficacy of the MT combined with TE. The paucity of clear guidelines on management of SIS is due to limitations in study designs and protocols in previous researches [9-11].
The aim of this study was to examine the overall effectiveness of the MT combined with TE in management of SIS and update the current state of knowledge with respect to pain, strength, active movement and SPADI scale.
Materials and Methods
Searching strategy
This study was conducted as per Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines and Cochrane handbook for systematic reviews of intervention and the trial was registered at central trial registry CTRI/2018/05/013892. Medical and health science databases were searched electronically: PubMed and Physiotherapy Evidence Database (PEDro) from beginning till the date of search (i.e.,) August 2020. The search strategies used in both databases were same and the keywords and Boolean operators used (AND, OR) are given in [Table/Fig-1]. The study was approved by the Institutional Ethical Committee (IEC number: 01/04/JMI/SS/FNS).
| Search steps | Query (PubMed/PEDro) | Items found (PubMed/PEDro) |
|---|
| #1 | Search Shoulder Impingement Syndrome (SIS) (Title/Abstract) | 2422/164 |
| #2 | Search Shoulder Impingement Syndrome (SIS) (Title/Abstract) AND physiotherapy (Title/Abstract) OR physical therapy (Title/Abstract) | 543/41 |
| #3 | Search Shoulder Impingement Syndrome (SIS) (Title/Abstract) AND Therapeutic Exercise (Title/Abstract) | 308/72 |
| #4 | Search Shoulder Impingement Syndrome (SIS) (Title/Abstract) AND Manual Therapy Search Shoulder Impingement Syndrome (Title/Abstract) OR manipulative therapy (Title/Abstract) | 146/36 |
| #5 | Search subacromial impingement syndrome (Title/Abstract) AND physiotherapy (Title/Abstract) OR physical therapy (Title/Abstract) | 546/26 |
| #6 | Manual Therapy combined with Therapeutic Exercise (Title/Abstract) AND physiotherapy (Title/Abstract) OR physical therapy (Title/Abstract) | 26/10 |
Selection criteria
The study population was patients with SIS, intervention was MT combined with exercise therapy, comparator was exercise alone and outcomes were pain level, muscle strength, ROM, and SPADI score.
Two reviewers independently screened the articles from the two databases. The articles were screened according to the title and abstract after removing the duplicates from two sources.
Inclusion and Exclusion Criteria
English research publications that were randomised controlled trials and quasi-experimental trails, comparing physiotherapy interventions for management of SIS, were considered for the analysis. Full text version was retrieved if the title and abstract were unclear for deciding the inclusion of the study. Furthermore, the studies were included if the SIS was clinically diagnosed with shoulder physical examination tests. Only published full text studies were considered for the present review.
Studies were excluded if they had patients with prior or existing shoulder dislocation in the same or opposite shoulder, Acromio-Clavicular (AC) joint pathology, cervical spine radiculopathy, prior shoulder surgery on symptomatic side, positive drop arm test and patients who were on current medication like Nonsteriodal Anti Inflammatory Drugs (NSAIDs) or who had received steroid injection in past 12 months. The studies in which physiotherapy management were not used, case studies and case reports were excluded.
Cohens kappa coefficient expressed the strength of the selection of the studies and disagreements were resolved by third reviewer. There was main disagreement between the two authors on the point of number of included studies {one author wanted to include articles that were purely on SIS (n=5), another author wanted to include articles that were based on specific phenotypes (subcoracoid impingement, calcific tendinitis etc.,) of impingement syndrome, including SIS (n=6). The third reviewer resolved this disagreement by only including articles having broad diagnosis of SIS rather than specific phenotypic diagnosis}.
Data extraction
Two reviewers extracted the data from the included studies by using a spreadsheet to record details of the study (author, year, journal, type of Physical Therapy (PT) intervention used, outcome measures and result of the study). Two reviewers reviewed the quality of the paper and also performed risk of bias assessment and disputes were resolved through discussion and consensus with the third author.
Outcome measure
The purpose of the present study was to summarise the effects of MT combined with TE vs TE alone for SIS on impairments like pain levels, functioning and strength of the shoulder girdle musculature.
Methodological quality of the study
Physiotherapy evidence database (PEDro) scale [12] was utilised to score the prospective experimental studies to be included in the review. Studies scoring high on the methodological quality (score ≥6/10) were only considered for the review. For the quasi-experimental controlled studies, the modified downs and black scale [13] was used for assessment of methodological quality. Studies scoring high on the methodological quality (score ≥17/28) were only considered for the review. Agreement level between the two reviewers was evaluated using kappa coefficient. The normative values for agreement were <0.40 for poor, 0.40 to 0.75 for acceptable and >0.75 for excellent [14].
Data synthesis
The conclusion was drawn by compiling findings in the study. The findings include checking for the methodological quality and result of the outcomes were used to form the final conclusion. A meta-analysis was performed using the required statistics (mean, Standard Deviation (SD), Standardised Mean Difference (SMD), 95% Confidence Interval (CI)) using the review manager software.
Statistical Analysis
The present study used the Rev Man version 5.3 (Cochrane collaboration) for meta-analysis and generating risk of bias charts. The readings from the outcome measures were obtained on a customised data filling form. The continuous data was evaluated for SMD with 95% CI at p<0.05.
Results
Selection of the Studies
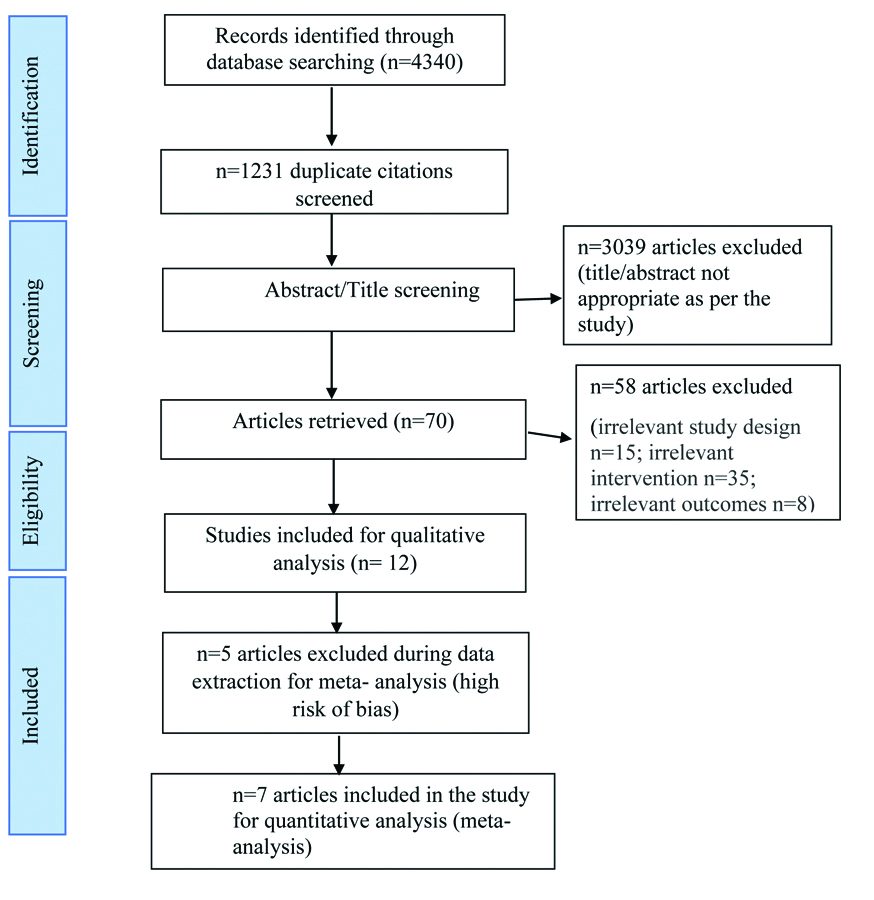
The initial search of the two databases resulted in 4340 results, out of which 1231 were duplicates. After the screening of articles by title and abstract, 70 articles were further shortlisted and these were studied in detail through their full text. Their detailed evaluation was done on basis of the participants, clinical diagnosis of SIS, study design, intervention etc. Evaluation resulted in exclusion of 58 articles. Twelve articles were included for the systematic review (qualitative analysis) [5,15-25] whereas out of these twelve studies, five were not considered for the quantitative analysis due to high risk of bias and finally, 7 studies were considered for meta-analysis in the present study [5,15-19,24] [Table/Fig-2]. The studies have been summarised in the form of table [Table/Fig-3].
PRISMA flowchart of search and screening process of studies.
Overview of the included studies.
| Study/PEDro/MDBS score | Participants/Sessions | Diagnosis | Outcome measures | Interventions | Reported result | Results/Conclusion |
|---|
| MT+TE Group | TE. Group | Pain | Str. | ROM QoL/FD |
|---|
| Bang MD and Deyle GD 2000 [15]Score-6/10Follow-up- 4 weeks and 8 weeks | Mean age±SD) 43.01±9.10 yrs Total participants: 52MT+ET and ET: 6 sessions | a) Scapula fixed, passive internal rotation in scaptionb) Active shoulder abduction.c) Resisted isometric test of abduction, IR and ER | a) Pain: VAS levelb) Strength: Isometric str, for IR, ER and abductors.c) Functional assessment scale | MT: PA mobilisation Exercise therapy:Planar exercises, rowing, seated press up, elbow push up, anterior and posterior shoulder girdle muscle exercise | Exercise therapy: Planar exercises, rowing, seated press up, elbow push up, anterior and posterior shoulder girdle muscle exercise | + | + | + | 4 weeks: no difference between groups8 weeks: MT+TE group was more effective than group |
| Bennell K et al., 2010 [16]Score-9/10Follow-up 12 weeks and 22 weeks | Mean age±SD: 60±10.21 yearsTotal participant 120 MT+ET and ET: 1st week-2 times a day.2nd week-once daily for 10 week | a) Painful active abduction/external rotationb) Positive “quick test” for impingement syndrome. | a) Pain: VAS scaleb) Strength- abduction, external rotation, internal rotationc) SPADI scale | Manual therapy: Passivemobilisation of the shoulder complex, STMExercise therapy:Scapular retraining,CBT, patient education.HEP maintained for further 10 weeks | Exercise therapy:Basic planar exercises, placebo ultrasonic, gentle local application of non-medical gel to the shoulder area for 10 min. | + | + | + | 12 weeks: no difference in both groups.At 22 weeks:MT+ET group was more effective than TE group. |
| Kachingwe AF et al., 2008 [5]Score-7/10Follow-up: 6 weeks | Mean age±SD:46.40±8.70 yearsTotal participant: 33All groups received treatment once a week for 6 weeks | a) Supero-lateral shoulder painb) Positive impingement testsc) Painful shoulder elevation d) Pain/restriction of functional movements. | a) Pain: VAS levelb) ROM: measurement of flexion and scaption.c) SPADI scale | Exercise plus mobilisation group:Exercises:capsular stretches, PCT, strength tr. of scapular musclesMobilisation group:shoulder joint distraction, AP, PA and inferior glides.Exercise plusMWM group:Exercise same as in Exercise plus mobilisation group | Exercise group: capsular stretches, PCT, strengthening of scapular musclesControl group:Only advise | + | NA | + | At 6 weeks: Pain level improved in exercise therapy and both Manual Therapy groups.At 6 weeks MWM group groups were most effective in improving function while mobilisation group was least. |
| Yiasemides R et al., 2011 [17]Score-9/10Follow-up at 1, 3 and 6 months | Mean age±SD: 60.10±4.32 yearsTotal participant: 98 | a) Painful active shoulder uniplanar movements, b) Hypomobility and pain during accessory motion testing of the shoulder complex joints. | a) SPADI scaleb) ROM c) Self-rated change in symptoms | Manual therapy:PA/AP glides, distractionExercise therapy,PE | Exercise therapy,PE | + | NA | + | Improvement in both groups, no significant difference between the groups |
| Conroy DE and Hayes KW; 1998 [18]Score-8/10Follow-up: 3 weeks | Mean age±SD: 52.90±3.45 yearsTotal participant:14MT+TE and TE: 3 sessions per week for 3 weeks. | a) Pain around superolateral shoulder region b) Decrease in AROM elevationc) Painful subacromial compressiond) Limitation in functional elevated positions | a) Pain: VAS levelb) ROM-elevation and rotation.c) Overhead function grading | Manual therapy: PA/AP glides, STMExercise therapy:AROM: multiplanar active assisted exercise with stick and towel Strengthening exercise: press up, isometric rotations, stretching exercises, PE | Exercise therapyAROM- active assisted exercise with stick and towel in all three planes.Strengthening exercise-press up, isometric rotation, stretching exercises, PE. | + | NA | + | MT+TE group was effective to reduce pain levelImprovement in both groups, no significant difference between the groups. |
| Lee DR and Kim LJ 2016 [21]Score-13/28Follow-up 8 weeks | Mean age±SD: 18.2 yearsTotal participant-23ET: 3 times a week for 8 weeks. | Physician diagnosed subacromial impingement syndrome over preceding 6 months | a) Strength Internal rotationb) External rotation | NA | CKC shoulder multiplanar exercises in sling | NA | + | NA | Internal and external rotation strength improved after intervention |
| Merolla G et al., 2010 [22]Score-15/28Follow-up 3 months6 months | Mean age±SD: 22±2.50 yearsTotal participant-31 ET: 2 sessions per week for 6 months | a) Negative for articular and muscular tears.b) Painful and weak infraspinatus | a) Pain: VAS scaleb) Isometric strength of infra muscle (normal vs scapular retraction) | NA | Side lying horizontal flexion, side lying vertical abduction, side lying shoulder external rotation, forward punches,rowing exercise, side lying posterior capsular stretching | + | + | NA | Pain level improved at both 3- and 6-months interval.Strength improved in both positions at 3 and 6 mo. Follow-up. |
| Merrola G et al., 2010 [23]Score-11/28Follow-up 3 and 6 months | Mean age±SD: 23±4.20 yearsTotal participant-29 | a) No articular and rotator cuff tearsb) Kibler scapular dyskinesis pattern classification | a) Pain: VAS scaleb) Strength: supr. and infra.c) ROM: IR | NA | Exercise for lower andmiddletrapezius, serratus anterior,Rhomboids and posterior capsular stretching | + | + | + | Pain level, strength and ROM improved at 3 and 6 months Follow-up. |
| De meyK et al., 2012 [25]score-15/28Follow-up 6 weeks | Mean age±SD: 24.6±7.81 yearsTotal participant-47TE: 6 weeks | Two out of five to be positive-a) Neers testb) H K testc) Jobes test d) Apprehensione) Relocation test | a) SPADI scaleb) MVIC activity of trapezius muscle group and serratus anterior. | NA | Side lying horizontal flexion, side lying vertical abduction, prone lying shoulder extension, side lying ER | + | - | + | Improvement in pain and function and reduction in trapezius muscle activity. |
| Cha JY et al., 2014 [24]Score-19/28Follow-up 12 weeks | Mean age: 22 years.Total participant: 30MT+TE: 3 sessions per week for 12 weeks | a) Postero-superior pain during ABER position.b) Positive apprehension and relocation testc) Positive impingement testsd) Positive Jobes test | a) Pain: VAS scaleb) IR/ER torque-dynamometry | Manual therapy: soft tissue mobilisationExercise therapy(Mon): scapular W, T and Y exercises(Wed) Rotations in scaption, Military press, “T” scapular exercise, triceps and biceps curls extension, rowing exercise(Fri) “T” scapular exercise | Group 2 (control group)No rehabilitation regime | + | + | NA | At 12 weeks MT+TE group showed better result. |
| Chen JF et al., 2009 [19]Score-8/10Follow-up: 1 and 6 months | Mean age-65 yearsTotal participants: 90MT+TE and TE group: 6 to 10 sessions | a) Unilateral pain over the shoulder girdleb) Painful ROMc) Reduced AROM <110°d) Hypomobility | a) SPADI scaleb) ROMc) Global perceived effect (GPE) scale | Manual therapy: GH, SC, and AC jointsExercisesCKC NM exercise, PE | Exercise CKC exercises to develop NM controlPE | + | NA | + | At 1- and 6-months improvement in both groupsMT +TE is not superior to TE. |
| Senbursa G et al., 2007 [20]Score-4/10Follow-up at 4 weeks | Mean age±SD: 48.8±7.7 yearsTotal participants:30MT+TE: 12 sessions (3 times a week × 4 weeks)TE: 7 days a week for 4 weeks (self-training) | a) Marked loss of AROM and PROM.b) Painful shoulderc) Painful isometric ER | a) Pain: VAS scaleb) ROMc) Strength | Manual therapy:GH joint mobilisation, DTF Exercise therapy:stretching, PNF exercise, resistance band planar and scapular exercises | Active ROM exercises, stretching, PNF exercises, resistance band planar and scapular exercises | + | + | + | MT +TE is more effective in improving pain, ROM and strength improvement |
MT+TE: manual therapy combined with therapeutic exercise; TE: therapeutic exercise; VAS: visual analogue scale; ROM: range of motion; MDBS: the modified downs and black scale; FD: functional disability; QoL: quality of life; IR: internal rotation; ER: external rotation; STR: strength; STM: soft tissue mobilsation; CBT: cognitive behaviuoral therapy; MWM: mobilisation with movement; GH: glenohumeral; SC: sternoclavicular; ST: scapulothoracic; PE: patienteducation; PNF: proprioceptive neuromuscular technique; PCT: posture correction technique: HEP: home exercise program; DTF: deep transverse friction; AROM: active range of motion; PROM: passive range of motion; CKC NM: closed kinetic chain neuromuscular exercise; MVIC: maximum voluntary isometric contraction; HK: hawkins kennedy test; ABER: abduction external rotation; PA glide: posteroanterior glide; AP glide: anteroposterior glide; +: Stands for improvement
Results of the Methodological Quality of the Study
Quality analysis of the studies [5,15-24,25] demonstrated score from 6 to 9 out of 10 on PEDro scale [Table/Fig-4a] and 11-19 out of 27 on the modified downs and black scale [21-24,25] [Table/Fig-4b]. Treatment allocation was concealed in only three studies [16,17,19]. Blinding of the patient was done in two studies [16,18], assessor blinding in six studies [5,15-19] and only two studies blinded the therapist [17,18]. The mean sample size of the included studies was 48 patients (range=29 to 120 patients). The outcome measure for all studies comprised pain, disability and functioning level and strength evaluation although the measurement scales/tools differed in studies. The mean score for the PEDro scale was 7.28.
PEDro scale scoring for studies.
| Articles | Adequate randomisation | Allocation concealment | Blinding patients | Baseline comparability | Binding therapist | Blinding assessor | Outcome data >85% | Intention to treat | Between group results | Point measures/measures of variability | PEDro score | Percentage |
|---|
| Bang MD and Deyle GD [15] | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 | 60% |
| Bennell K et al., [16] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 | 90% |
| Chen JF et al., [19] | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 | 80% |
| Kachingwe AF et al., [5] | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | 70% |
| Yiasemides R et al., [17] | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 | 90% |
| Conroy DE and Hayes KW [18] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 | 80% |
| Senbursa G et al., [20] | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 4 | 40% |
Modified downs and black scale scoring for studies.
| Article | Reporting | External validity | Internal validity (study bias) | Internal validity (confounding selection bias) | Power | Score (total) |
|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 27 |
| Cha JY et al., [24] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 19 |
| Merolla G et al., [22] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 11 |
| Merolla G et al., [23] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 15 |
| De mey K et al., [25] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 15 |
| Lee DR and Kim LJ [21] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 13 |
| Scoring: high quality/low bias (>20); moderate quality (17-19); low quality/high risk of bias (<16) |
Some studies for which data was extracted were quasi-experimental studies [21-24,25]. While PEDro scale is specific for scoring in randomised control trials. Therefore, the modified downs and black scale was used for these studies. Inter-rater agreement for all items on each scale was examined and kappa coefficient with 95%CI was calculated to be 0.73 (95% CI 0.70-0.84, p<0.001) for the modified downs and black scale and 0.80 (95% CI 0.71-0.87, p<0.001) for PEDro scale which suggests acceptable to substantial agreement respectively. The criteria for evaluating grades of risk of bias for PEDro scale was a score of greater than equal to 6 out of 10. The modified downs and black scale classified studies as per score obtained as high quality/low bias (>20), moderate quality (17-19) and low quality/high risk of bias (<16). Seven studies had low risk of bias i.e., scored 6 or more on PEDro scale and scored >16 on the modified downs and black scale [5,15-19,24]. Five trials obtained score in high risk of bias (PEDro score <6 and the modified downs and black score<16) [20-23,25] [Table/Fig-4a,b].
Risk of Bias Assessment Across Studies
Commonly scored methodological shortcomings were inadequate allocation concealment (n=4) [5,17,18,20], inadequate blinding Patients (n=5) [5,15,17,19,20] and inadequate therapist blinding (n=5) [5] [Table/Fig-5].
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study (Rev Man 5.3).
| Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding of participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias |
|---|
| Bang MD and Deyle GD, 2000 [15] | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ? |
| Bennell K et al., 2010 [16] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? |
| Cha JY et al., 2014 [24] | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ? |
| Chen JF et al., 2009 [19] | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | |
| Conroy DE and Hayes KW 1998 [18] | ✓ | ✗ | ? | ✓ | ✓ | ✓ | ✓ |
| Kachingwe AF et al., 2008 [5] | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ? |
| Yiasemides R et al., 2011 [17] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? |
| ✓= low risk of bias; x= high risk of bias; ?= unclear risk of bias. |
As far as the modified downs and black checklist is concerned the shortcomings were mainly in the external validity (n=4) [21,22,24,25], internal validity (n=4) [21-23,25] and confounding selection bias (n=3) [21-23] [Table/Fig-4b].
Risk of Bias Across Outcomes
a) Pain: Pain was reported by five studies at follow-up. All the five studies had low risk of bias [5,15,16,18,24]. All the studies reported reduction in pain in the MT and TE group at follow-up. There was statistically significant difference in pain reduction in between groups also. The post intervention measurements were done from 3 week onwards to 22 weeks.
b) SPADI: This was measured by SPADI scale. Four studies were evaluated for effectiveness of MT and TE for SPADI scale. All the four articles had low risk of bias (n=4) [5,16,17,19]. Two studies reported statistically significant difference in SPADI score after intervention in favours of MT combined with TE group [5,16] whereas two trials reported no statistically significant improvement in SPADI score [17,19].
c) Strenght: Three studies evaluated strength using a dynamometer. Three studies qualified the methodological criteria and had low risk of bias (n=2) [15,24]. Both the article reported statistically significant improvement (external rotation) in favour of the Therapeutic Exercise (TE) group.
d) Range of Motion (ROM) (elevation and abduction): Four studies evaluated the ROM (elevation and abduction) after interventions. All 4 studies had low risk of bias [5,17-19]. Two articles reported no significant differences in the elevation range [17,19]. However, 2 studies [5,18] reported improvement in elevation ROM.
Qualitative Summary of Strength of Evidence (Meta-analysis)
To construct the best evidence synthesis, five studies were rated to be of high quality [16-19,24], three were rated as medium quality [5,15,25] and four were low quality studies [20-23]. However, common exercise performed in the five high quality trials are glenohumeral mobilisations techniques, motor control exercises and scapular stabilisation and glenohumeral strengthening exercises.
Quantitative Analysis (Data Synthesis)
Seven studies were eligible for inclusion in the statistical pooling of data [5,15-19,24]. Reason for exclusion of other studies was score less than six on PEDro scale and four studies did not have any determinable control groups.
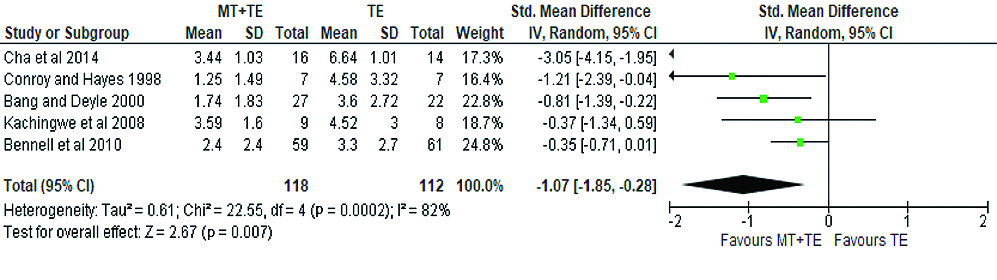
a) Pain: Five studies quantitatively assessed to analyse the effect of MT combined with TE when compared to TE alone [5,15,16,18,24]. Two hundred and thirty patients provided data related to effect of interventions on pain. Figure demonstrated that there was significant effect of combined MT and exercise on pain reduction (SMD: -1.07 (95% CI: -1.85, -0.28, p< 0.01) I2=82% [Table/Fig-6a].
Forest plot showing results of Manual Therapy (MT) combined with TE vs TE alone for pain.
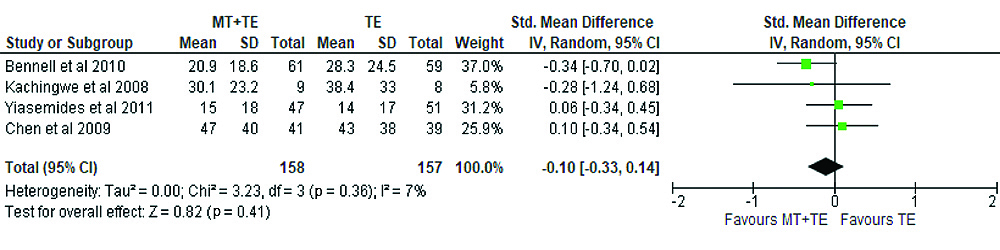
b) SPADI Scale: Four studies quantitatively assessed to analyse the effect of MT combined with TE when compared to TE alone [5,16,17,19]. A total of 315 patients provided data related to effect of intervention on SPADI scoring. Figure demonstrated that there was no significant effect of combined MT and exercise on SPADI scale scoring (SMD: - 0.10 (95% CI: -0.33, 0.14, p=0.41) I2=7% [Table/Fig-6b].
Forest plot showing results of Manual Therapy (MT) combined with TE vs TE alone for SPADI.
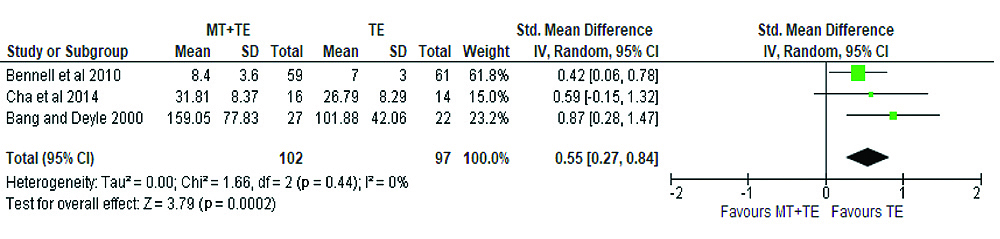
c) Strength: Three studies analysed the effect of intervention on strength of external rotators [15,16,24]. The total number of patients who provided data for the effect of intervention on external rotator strength was one hundred and ninety-nine. Figure demonstrated that there was a significant effect of TE intervention as compared to MT combined with TE (SMD: 0.55 (95% CI: 0.27, 0.84, p<0.01) I2=0% [Table/Fig-6c].
Forest plot showing results of Manual Therapy (MT) combined with TE vs TE alone for strength (external rotation).
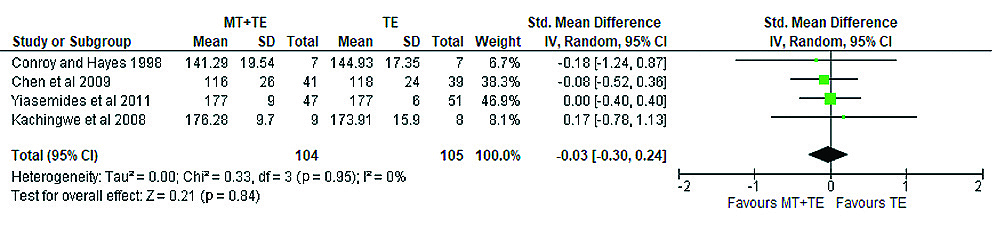
d) Range Of Motion (ROM) (elevation): Four studies analysed the effect of intervention on shoulder elevation range [5,17-19]. Two hundred and nine patients provided the data for the effect of intervention on shoulder elevation range. Figure demonstrated that there was a no significant effect of MT intervention when compared to TE (SMD:-0.03 (95% CI: -0.30, 0.24, p=0.84) I2=0% [Table/Fig-6d].
Forest plot showing results of Manual Therapy (MT) combined with TE vs TE alone for ROM elevation.
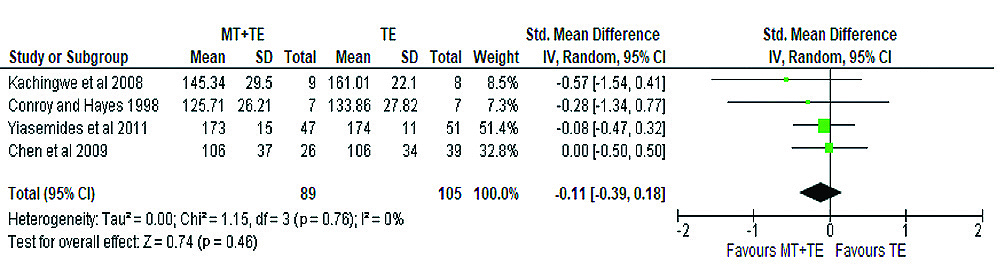
e) Range Of Motion (ROM) (abduction): Four studies analysed the effect of intervention on shoulder elevation range [5,17-19]. One hundred and ninety- four patients provided the data for the effect of intervention on shoulder elevation range. Figure demonstrated that there was a no significant effect of MT intervention when compared to TE (SMD: -0.11 (95% CI: -0.39, 0.18, p=0.46) I2=0% [Table/Fig-6e].
Forest plot showing results of Manual Therapy (MT) combined with Therapeutic Exercise vs Therapeutic Exercise alone for ROM abduction.
Discussion
The purpose of this review was to examine the gross effects of MT combined with TE over TE alone in patients diagnosed with SIS. The results of the quantitative assessment summaries that MT combined with TE are effective in reducing pain following treatment. This assessment is supported by three high quality [16,18,24] and two moderate quality [5,15] researches. Secondly, the external rotation strength increase in the TE group was supported by two high quality [16,24] and one moderate quality studies [15]. Thirdly, SPADI scale score improvement showed a nonsignificant change between the two treatment protocols. SPADI scale result was supported by 3 high quality [16,17,19] and one moderate quality [5] studies. ROM (elevation) also showed nonsignificant change and the results were supported by three high quality [17-19] and one moderate quality [5] studies while nonsignificant change in ROM (abduction) was supported by four high-quality studies [5,17-19]. In terms of similarity of the exercise type usage in the medium and high-quality studies and its association with pain decrement and improved external rotation strength, the rotator cuff strengthening exercise, scapular muscle exercises with resistance bands, stretching’s and mobilisation of the shoulder complex were a common denominator in these studies.
Twelve studies were qualitatively assessed. Five studies were found to have high quality/low risk of bias [16-19,24], two studies were having moderate quality [5,15] and five were found to have low quality/high risk of bias [20-23,25]. The largest risk of bias was due to inadequate allocation concealment and inadequate blinding of participants and assessors. In general, quantitative analysis was restricted to 7 trials due to the methodological quality of trials.
The literature review also indicates that there is limited meta-analysis studies comparing MT combined with TE. The current evidence is inconclusive with respect to beneficial effect of combine MT and TEs for reducing pain, improving function and limiting disability [26]. Another study performed systematic review and concluded no outcomes (pain, ROM, strength) in favour of combined MT and TE group [26]. Whereas, some studies demonstrated clinically important statistically significant effect on pain, ROM and functional improvement [27-33]. The present study also revealed strong evidence for pain reduction and external rotation strength improvement with a combination of MT and TE. There is moderate to strong evidence with regard to these two parameters which was previously not found to be the case.
There can be three plausible reasons for results obtained in the present review. Firstly, significant pain reduction with MT combined with TE occurred due to stimulation of the pain gate mechanism. The additive effect of MT and TE produced greater stimulation of the large diameter mechanoceptors (A-delta fibres) located in the joint capsule and ligaments than TE alone. The A delta fibre stimulation blocks the ascending transmission of the pain carrying C-fibres at the spinal level itself and reduces the pain perception resulting in analgesia. Even Periaqueductal Grey Matter (PAG) can be stimulated resulting in activation of the descending pain suppression system using tolerable noxious stimulation. This has been reported to release natural pain-relieving chemicals known as endorphins at the level of stimulation [34].
Secondly, significant increase in strength of external rotation with TE alone occurred due to changes in the muscular apparatus after specified duration of training. The increase in strength of the muscle happens due to neural adaptations and muscular adaptations. Initially, 3 weeks of rehabilitation is dominated by neural changes and afterwards muscular changes follow in healthy subjects. The neural adaptations include, increase in motor unit recruitment and neural discharges while there are m RNA changes and satellite cells upregulation during muscular adaptations phase. Due to pre-existing dysfunctions or pathological conditions strength training usually require longer time than usual to exert its beneficial effects [35].
Thirdly, the main rationale behind nonsignificant findings for disability and ROM is nonoptimal duration of the treatment. Most of the studies in the present review had an average intervention length of 7 weeks. The existing dysfunction comprise tightness of the muscles, capsules and decreased accessory of motion. Research has found that minimum 8 weeks of static stretching is sufficient to increase muscle length in healthy subjects [36]. The duration of intervention in the studies taken in present review might not have been enough in presence of pre-existing dysfunctions associated with SIS. In addition, patients with chronic musculoskeletal pain demonstrate an increased tolerance to stretch after 3 weeks of static stretching. The protocol of studies that were included didn’t use progressive MT which could have led to plateauing of therapeutic effects. Hence, these might be the rationales for not observing significant improvement.
The risk of bias in this study was low which gives strength to its conclusions. No intervention linked adverse clinical events were reported in this study. The bias was reduced because independent reviewers searched and selected the relevant studies and also assessed the quality of the studies.
Limitation(s)
This study has some limitations as the present review was done using only two databases and the authors limited the search to English language publications only, therefore, some relevant publications might have been missed.
Conclusion(s)
Based on high to moderate quality, the present review concludes that physiotherapy interventions are effective in treatment of impairments seen in patients with SIS. A holistic approach comprising a combination of MT and TE (glenohumeral mobilisation techniques, motor control exercises and scapular stabilisation and glenohumeral strengthening exercises) is effective to combat the impairments caused by SIS In future, adequately sampled, high-quality randomised controlled trails are needed to allow statistical pooling and quantitative confirmation of the results. In this review, studies which had used appropriate clinical criteria as a diagnostic measure for SIS were chosen. Since, clinical diagnostic method is reliable and valid but not a gold standard method, this could have led to outcomes being biased. Therefore, further studies utilising combined clinical and radiological diagnostic criteria are needed. In future, research on onset based (acute, subacute, chronic) and location based (subcoracoid, internal, subacromial) phenotypic classification should be done to investigate the effects of MT combined with TE.