Bilayer Mesh Repair for Inguinal Hernia- An Open Alternative to Laparoscopic Repairs
Abinash Kanungo1, Chinmaya Ranjan Behera2, Riddhika Majumder3, Subrajit Mishra4, Subrat Kumar Sahu5, Pran Singhpujari6
1 Assistant Professor, Department of Surgery, Kalinga Institute of Medical Sciences, Bubaneswar, Odishha, India.
2 Assistant Professor, Department of Surgery, Kalinga Institute of Medical Sciences, Bubaneswar, Odishha, India.
3 Postgraduate, Department of Surgery, Kalinga Institute of Medical Sciences, Bubaneswar, Odishha, India.
4 Senior Resident, Department of Surgery, Kalinga Institute of Medical Sciences, Bubaneswar, Odishha, India.
5 Associate Professor, Department of Surgery, Kalinga Institute of Medical Sciences, Bubaneswar, Odishha, India.
6 Professor, Department of Surgery, Kalinga Institute of Medical Sciences, Bubaneswar, Odishha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chinmaya Ranjan Behera, Assistant Professor, Department of Surgery, KIMS and PBMH, KIIT Campus 5, Patia, Bubaneswar, Odisha-751024, India.
E-mail: chinmayarbehera@gmail.com
Introduction
In 1999, Gilbert described the technique of using a bilayer mesh device, Prolene Hernia System (PHS) for tension free repairs of inguinal hernias through an open anterior approach. This provides an anterior, posterior and plug repair, and hence successfully covers the myopectineal orifice, the lack of which is a glaring drawback for the Lichtensteins repair. This also confers the same benefit provided by the laparoscopic hernia repairs which uses the preperitoneal space to cover this same region that is, Transabdominal Preperitoneal Patch Plasty (TAPP) and Total Extraperitoneal patch Plasty (TEP).
Aim
To observe the overall outcome of using an open bilayered dual mesh in a population of Odisha, attending a tertiary care hospital.
Materials and Methods
All patients admitted with inguinal hernias in the Department of General Surgery, Pradyumna Bal Memorial Hospital, KIMS, Odisha, India were included in the study. They all underwent the PHS bilayer mesh repair. The relevant patient specifics like, preoperative clinical findings and intra and postoperative results were noted in a master chart. Patients were followed-up for one year, and further long-term complications were noted, if any.
Results
There were a total of 40 patients. The mean duration for the procedure was 61.5 minutes (SD-22.8) and there was no inadvertent injury. The patients were encouraged to resume all physical activities from the first postoperative day. All the patients had an uneventful recovery, with a mean hospital stay of four days. Four patients presented with seroma after one week of surgery, while 22 patients had cord oedema. Both subsided spontaneously within three weeks, without further intervention. No recurrence was noted in any of the patients.
Conclusion
The PHS bilayer dual mesh repair is ideally suited for population in a low resource setting. It ensures coverage of the entire vulnerable area of groin along with a considerably shorter duration of operation, minimal risk of intraoperative injury.
Gilbert, Prolene hernia system, Transabdominal preperitoneal, Totally extra peritoneal
Introduction
Globally, inguinal hernia remains, one of the most common surgical pathology. Annually, more that 20 million people undergoes Inguinal Hernia Repair surgery, worldwide [1,2]. Inguinal hernia occurs in the groin area, it could be direct, indirect, or bilateral. It forms in around 75% of all abdominal wall hernias with a life-time prevalence of 27-43% in men and 3-6% in women [3,4] by protrusion of viscera or adipose tissue through the inguinal or femoral canal. Inguinal Hernias are almost always symptomatic, and surgery remains the only cure with high success rate [1]. Strangulation is the most life threatening complication, if remains untreated.
Though a variety of procedures can be performed, none can be termed as ideal. Every surgeon’s main goal in hernia surgery is maximum safety, fewest complications, minimal disability and permanence of repair. Surgeons should protect the entire vulnerable area of groin for permanence of hernia repair, especially with newer tension-free mesh technique. Laparoscopic techniques for inguinal hernia have been introduced to reduce hernia recurrence and facilitate patient recovery and early return to work.
Several studies comparing laparoscopic hernia repair with a variety of open conventional hernia repairs and open tension-free mesh techniques have been published. Laparoscopic repairs have been associated with less postoperative pain, a shorter convalescence and an earlier return to work compared with the open tension-free repair. Still, the place of Laparoscopic Inguinal Hernia Repair (LIHR) remains controversial because of technical complexity, serious complications, and longer operating time [4]. Laparoscopic surgery requires complicated medical equipment and surgical tools that are quite difficult to sterilise and to correctly maintain in good condition.
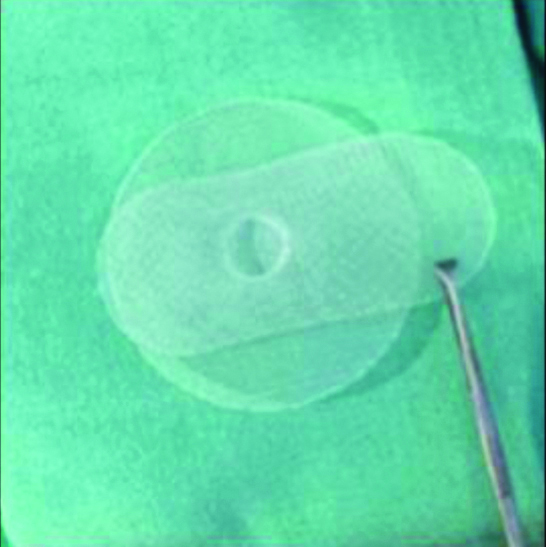
In 1999 Gilbert described a novel technique of using a bilayer mesh device (PHS) for tension-free repair of inguinal hernias through an open approach [4]. [Table/Fig-1] shows the image of PHS. This provides an anterior, posterior and plug repair, thereby covering the entire Myopectineal Orifice of Frauchaud, which is a major advantage of this repair over the other open mesh repair. However, its advantage over laparoscopic repairs is its shorter operative time, easy learning curve, can be done under regional or local anaesthesia and cost effectiveness. It also avoids any inadvertent intraoperative injuries (bowel, bladder and vessel injuries), which is a major concern in laparoscopic hernia repairs [4-6].
Most of the patients visiting the study hospital are farmers or daily labourers that present with large, neglected hernias. As their livelihood depends on heavy physical labour, it is essential that they are provided with a repair that ensures early return to work without compromising on their physical abilities. With this study, the authors aimed to evaluate the outcome of using PHS technique/gilberts open bilayer mesh technique in patients with hernia.
Materials and Methods
This cross-sectional observational study was conducted in the Department of General Surgery at Pradyumna Bal Memorial Hospital, KIMS, Bhubaneswar Odisha, India, between October 2017 to September 2019, with due consent from all the patients. Ethical clearance committee approval was taken prior to the study. (KIMS/KIIT/IEC/68/2017).
A sample size of 40 patients was taken, on the basis of number of patients who had consented to undergo PHS repair for inguinal hernia, in the due course of time.
Inclusion criteria: All patients that presented to the Surgical Out Patient Department (OPD) of PBMH KIMS with inguinal hernia and were diagnosed with Inguinal Hernia by clinical examination, were included for the study. All these patients were who were to undergo the surgery, were explained about the PHS procedure and the alternative options. Only those patients who consented for PHS repair were included in the study group.
Exclusion criteria: Patients below 12 years of age, or patients having obstructed hernia were excluded from the study. Patients with any other co-morbidities such as immunocompromised status, cardiopulmonary compromise, renal/liver failure and ascites were also excluded.
The following details were noted- age of patient, symptoms and the duration, medical history, complete physical examination findings, laboratory investigations, radiological investigations and duration of hospital stay. Intraoperative time was also noted (start time- when the skin incision was done, end time- once the site was sutured). Patients who participated for the study was then followed-up for a period of one year and further short term or long-term complications, if any, were noted.
Gilberts Open Bilayer Mesh (PHS) Surgical Technique
The PHS was used for all repairs. This 3D mesh comprises of two layers; an ellipsoid onlay layer, and an inferior layer for introduction into the preperitoneal space. Both layers are joined by a connecting cylinder of mesh acting as a plug into the internal ring.
The hernia sac was dissected and reduced into the abdominal cavity. To place the deep layer of the mesh, a preperitoneal space was created behind the transversalis fascia. Fingers were used for dissection and with the help of gauze the preperitoneal space was seperated. The onlay layer was trimmed and an opening was created for the spermatic cord. It was then fixed with a suture (2-0 prolene), at the cardinal points of the inguinal ligament and the conjoined tendon [Table/Fig-2].

Statistical Analysis
Categorical variables were presented as frequency. Continual parameters were shown as mean. The Chi-square test was applied for statistical analysis. A p-value of less than 0.05 was considered as statistically significant. All the analysis was carried out using the standard statistical software STATA 13.1.
Results
The minimum age of occurrence of Inguinal hernia was 20 years. The oldest patient was 77 years. The mean age of the population was 43.5±15.7 years; 39 out of 40 patients were male. Maximum number of patients had symptoms for 1-5 years. The most frequent presentation observed was a right-sided indirect inguinal hernia [Table/Fig-3]; However a varied presentation in terms of size and site of hernias were dealt with in this study [Table/Fig-4,5]. The occupational characteristics and co-morbidities are tabulated in [Table/Fig-6,7].
Distribution of type of hernia.
| Type | Frequency | Percentage |
|---|
| Right indirect | 17 | 42.5 |
| Left indirect | 8 | 20 |
| Right direct | 6 | 15 |
| Left direct | 3 | 7.5 |
| Bilateral direct | 3 | 7.5 |
| Bilateral indirect | 2 | 5 |
| Bilateral recurrent | 1 | 2.5 |
| Total | 40 | 100 |
Large bilateral recurrent inguinal hernia operated using bilayer mesh device.

Large left inguinal hernia operated using PHS device.

Frequency of co-morbidities.
| Co-morbidity | Frequency | Percentage |
|---|
| None | 28 | 70 |
| Hypertension | 5 | 12.5 |
| Diabetes | 4 | 10 |
| Both | 3 | 7.5 |
| Total | 40 | 100 |
Distribution of occupation.
| Occupation | No. of Patients |
|---|
| Farmers | 22 |
| Daily labourers | 9 |
| Business men | 4 |
| School teachers/professor | 2 |
| Sales person | 1 |
| Retired clerk | 1 |
| Housewife | 1 |
The mean duration of surgery was 61.5 minutes. The most frequently found content of the hernia was omentum [Table/Fig-8]. All patients received 2 doses of injectable amoxycillin and clavulanic acid 1.2 g, with exception of diabetic patients (N=4), who received four such doses. All patients were given the same postoperative analgesia regime-two doses of paracetamol 1 g Intravenous (IV) injection eight hourly in the immediate postoperative period. Diclofenac 100 mg IV injection was kept as an SOS drug. They were then given only paracetamol 650 mg tablet thrice daily for five days from the first postoperative day. None of the patients required additional analgesics. All patients were ambulated on the 1st postoperative day. The mean postoperative stay was for 4±2 days.
Intraoperative finding of omentum as content.

The patients were followed-up for a mean period of 266±40 days. Thirteen patients were followed-up for a full year. There were many dropouts in the early postoperative follow-up period. No recurrences were noted in the postoperative follow-up period. Four out of 40 patients presented with seroma after one week of surgery, while 22 patients had cord oedema. Both subsided spontaneously within three weeks, without further intervention. There was no evidence of surgical site infection in any patient.
Discussion
Since the description of the onlay mesh technique by the Lichtenstein institute in 1989, several tension-free techniques have been described over the years. With the advances in laparoscopic surgery, laparoscopic TAPP repair and totally extraperitoneal repair approaches are being the most commonly used techniques in recent decade [5]. Each technique addresses a different area of weakness in the groin apparatus, while each claim low levels of recurrence [5]. It eventually lies down in the hand of the surgeon to include the most effective and less complicated procedure for their patients and fellow surgeons. For this study the surgeon decided to observe the PHS technique as its course of action has a combination of three techniques [6,7]. The “Rives technique”, in which the internal round pre-peritoneal component reinforces the myopectineal orifice, the “Lichtenstein technique”, where the external oval component placed over the fascia transversalis reinforces the floor of the groin, and finally, the “mesh plug technique”, where the internal and the external components are linked together by a cylinder placed in the hernia ring [6].
On the other hand, laparoscopic hernia repair may require general or regional anaesthesia for the procedure, longer operative duration, long learning curve and over all possess a higher risk for serious complications [8-11]. As demonstrated by Neumayer L et al., the risk of life threatening complication were high in LIHR than open hernia surgery with a adjusted Odd ratio of 11.2 (1.3-95.3) and odd ratio of recurrence at two year of surgery being 2.2 (1.5-3.2) [12]. It has also been determined that open hernia surgery is more cost-effective when compared to LIHR. Moreover, LIHR is a challenging procedure [13].
PHS can be a suitable alternative procedure to Lichtenstein Mesh Repair (LMR), and has been demonstrated in various studies done previously [14-17]. It has been further stated that the PHS has advantage over LMR technique due its combined triple mechanism of action. A comparative study done by Hebsur N and Shankar JCR, regarding the short-term and long-term complications of open hernioplasty repair technique demonstrated that seroma, infection, chronic pain were the most common complications [18]. In this study, 4 out of 40 patients developed seroma and 22 patients developed cord oedema, which subsided eventually without any further intervention.
Although laparoscopic hernia surgery and robotic techniques are the trending technique of the new world. PHS, one of the oldest techniques, still remains a safe practice as it marks a small learning curve while performing the surgery. The technique remains less complicated [13,18] and less time consuming to perform for the surgeon. Simultaneously, it remains one of the cost-effective techniques in comparison to other procedures like laparoscopic hernia surgery.
As from the above study, it can be concluded that most patient did not have any long term or short-term complications during the surgery. The technique was not only surgeon friendly but also provided compliance for the patients with minimal blood loss and postoperative complications. This procedure was done under simple local/spinal or epidural anaesthesia and did not require general anaesthesia. The mean postoperative patient stay at the hospital was 4±2 days.
Limitation(s)
The sample size is limited and the mean follow-up period was limited to 12 months wherein there were many drop outs too.
Conclusion(s)
From the study, it can be concluded that the procedure is safe in experienced and skilled hands. The open bilayer technique is easy to learn, and has a non-significant learning curve, short operative time. As, this mesh covers the entire myopectineal orifice, and has a three layer action, the PHS mesh repair may represent a superior alternative for the repair of inguinal hernias. It is a safe and effective technique for inguinal hernia training for trainees, with similar results to staff surgeons with less operative time that with other inguinal hernia techniques.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 07, 2021
Manual Googling: Jan 30, 2021
iThenticate Software: Mar 31, 2021 (19%)
[1]. Köckerling F, Simons MP, Current concepts of inguinal hernia repairVisc Med 2018 34(2):145-50.10.1159/00048727829888245 [Google Scholar] [CrossRef] [PubMed]
[2]. Jha DS, Pankaj D, A study to assess the prevalence and risk factors of inguinal herniaInt J Surg Sci 2020 4(3):330-32.Available from: https://doi.org/10.33545/surgery.2020.v4.i3e.51410.33545/surgery.2020.v4.i3e.514 [Google Scholar] [CrossRef]
[3]. Kingsnorth A, LeBlanc K, Hernias: inguinal and incisionalLancet 2003 362(9395):1561-71.10.1016/S0140-6736(03)14746-0 [Google Scholar] [CrossRef]
[4]. Young J, Gilbert AI, Gilbert Technique: PHS Bilayer Repair: A Step-by-Step GuideIn: The Art of Hernia Surgery 2018 ChamSpringer International Publishing:285-99.10.1007/978-3-319-72626-7_29 [Google Scholar] [CrossRef]
[5]. Gilbert AI, Graham MF, Voigt WJ, A bilayer patch device for inguinal hernia repairHernia 1999 3(3):161-66.10.1007/BF01195319 [Google Scholar] [CrossRef]
[6]. Mahajan N, Sharma N, Gupta N, Inguinal hernia repair using prolene hernia system- A simplified technique for beginnersInt J Contemp Med Res [IJCMR] [Internet] 2020 7(1):A04-09.Available from: http://dx.doi.org/10.21276/ijcmr.2020.7.1.4710.21276/ijcmr.2020.7.1.47 [Google Scholar] [CrossRef]
[7]. Mottin CC, Ramos RJ, Ramos MJ, Using the Prolene Hernia System (PHS) for inguinal hernia repairRev Col Bras Cir 2011 38(1):24-27.10.1590/S0100-6991201100010000521537739 [Google Scholar] [CrossRef] [PubMed]
[8]. Callesen T, Bech K, Kehlet H, Prospective study of chronic pain after groin hernia repair: Chronic pain after groin hernia repairBr J Surg 1999 86(12):1528-31.10.1046/j.1365-2168.1999.01320.x10594500 [Google Scholar] [CrossRef] [PubMed]
[9]. Bringman S, Ramel S, Heikkinen TJ, Englund T, Westman B, Anderberg B, Tension-free inguinal hernia repair: TEP versus mesh-plug versus Lichtenstein: A prospective randomized controlled trialAnn Surg 2003 237(1):142-47.10.1097/00000658-200301000-0002012496542 [Google Scholar] [CrossRef] [PubMed]
[10]. Prosanta B, Surgical options in inguinal hernia: Which is the bestIndian Journal of Surgery (ISSN: 0972-2068) 2006 68(4):191-200. [Google Scholar]
[11]. EU Hernia Trialists CollaborationLaparoscopic compared with open methods of groin hernia repair: Systematic review of randomized controlled trialsBr J Surg 2000 87(7):860-67.10.1046/j.1365-2168.2000.01540.x10931019 [Google Scholar] [CrossRef] [PubMed]
[12]. Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Open mesh versus laparoscopic mesh repair of inguinal herniaN Engl J Med 2004 350(18):1819-27.10.1056/NEJMoa04009315107485 [Google Scholar] [CrossRef] [PubMed]
[13]. Solodkyy A, Feretis M, Fedotovs A, Di Franco F, Gergely S, Harris AM, Elective “true day case” laparoscopic inguinal hernia repair in a District General Hospital: Lessons learned from 1000 consecutive casesMinim Invasive Surg 2018 2018:712375410.1155/2018/712375429971162 [Google Scholar] [CrossRef] [PubMed]
[14]. Badkur M, Garg N, Comparative study of prolene Hernia System and Lichtenstein method for open inguinal hernia repairJ Clin Diagn Res 2015 9(6):PC04-07.10.7860/JCDR/2015/12177.600926266158 [Google Scholar] [CrossRef] [PubMed]
[15]. Shankar JCR, Hiregoudar AD, Comparative study between lichenstein mesh repair and prolene hernia system in the management of uncomplicated inguinal herniaIJSS 2016 2(5):05-11. [Google Scholar]
[16]. Sanjay P, Watt DG, Ogston SA, Alijani A, Windsor JA, Meta-analysis of Prolene Hernia System mesh versus Lichenstein mesh in open inguinal hernia repairSurgeon 2012 10(5):283-89.10.1016/j.surge.2012.06.00122824553 [Google Scholar] [CrossRef] [PubMed]
[17]. Gohel J, Patel U, Prolene hernia system in the tension-free repair of primary inguinal herniasNat J Med Res 2015 2(3):302-05. [Google Scholar]
[18]. Hebsur N, Shankar JCR, A study of short and long term complications of prolene hernia systemInt Surg J 2017 4(4):1167-70.10.18203/2349-2902.isj20170999 [Google Scholar] [CrossRef]