Monoclonal Gammopathy Presenting as Peripheral Neuropathy
Vishaka Agarwal1, Koukutla Soundarya Rajeshwari2, KT Jayakumar3, Satish4, Chetan Somu5
1 Postgraduate Student, Department of Internal Medicine, SRM Institute of Science and Technology, Chennai, Tamil Nadu, India.
2 Postgraduate Student, Department of Internal Medicine, SRM Institute of Science and Technology, Chennai, Tamil Nadu, India.
3 Professor, Department of Internal Medicine, SRM Institute of Science and Technology, Chennai, Tamil Nadu, India.
4 Resident, Department of Neurology, SRM Institute of Science and Technology, Chennai, Tamil Nadu, India.
5 Senior Resident, Department of Internal Medicine, SRM Institute of Science and Technology, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vishaka Agarwal, Flat No. 3133, Tower 3, Estancia Towers, Guduvanc Hery, Chennai, Tamil Nadu, India.
E-mail: vishaka.532494@gmail.com
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a disorder of peripheral nervous system, which presents with a long duration (eight weeks) of sensory and/or motor, symmetric/asymmetric symptoms. Aetiology ranges from infections, inflammations, autoimmune disorders, to vasculitis and malignancies. Hereby, authors report a case of a 40-year-old male patient who presented with complaints of bilateral lower limb numbness and weakness, and bilateral upper limb numbness, since two months, which was gradually progressive. On examination, he was found to have muscle wasting in his bilateral upper limb web spaces, left anterior thigh muscle, decreased tone in bilateral upper limbs and lower limbs, decreased power in both his upper limbs distally and decreased power in both his lower limbs (distal>>proximal) was seen. Superficial reflexes were normal with bilateral plantar being equivocal. Deep tendon reflexes were absent in bilateral upper and lower limbs. Tremors of bilateral upper limbs on extension were present. Loss of vibration sense throughout, loss of joint position sense at bilateral big toe and ankle joint and foot drop of his left lower limb were noticed. A diagnosis of CIDP with underlying plasma cell disorder was made after serum electrophoresis, immune-fixation and electrodiagnostic studies. The patient was started on prednisone 60 mg once daily, discharged and advised for monthly follow-up. Diagnosis of CIDP and the underlying cause is multifactorial, which can be misdiagnosed, presenting as a challenge. Hence, a detailed clinical examination, appropriate investigations are very crucial in diagnosing and treating a case of CIDP and its underlying cause.
Chronic inflammatory demyelinating polyradiculoneuropathy, Electrodiagnosis, Plasma cell dyscrasia
Case Report
A 40-year-old right handed male, presented with complaints of numbness in his bilateral lower limbs, difficulty in walking, and numbness of his bilateral distal upper limbs which was gradually progressive, since past two months. Numbness started in his left lower limb and progressed to his right lower limb over one week duration, followed by numbness of his bilateral distal upper limbs. Subsequently, he developed weakness of both lower limbs. He also complained of difficulty in getting up from squat position and climbing staircase. Initially, he was able to walk with support, but gradually developed weakness to such an extent that later he became bed bound. There were no complaint of truncal or bladder and bowel involvement. There was history of loss of weight (15 kilogram) in the past 3-4 months. His medical/surgical and family history was unremarkable. Patient had no addictions or toxin exposure.
On general examination, patient had bilateral lower limb painless, pitting oedema, extending up to his ankle joints. Skin changes like thickening of the skin, hyperpigmentation were not present. Vitals were stable. On Central Nervous System (CNS) examination, there was muscle wasting in his bilateral upper limb web spaces, left anterior thigh muscle, decreased tone in bilateral upper limbs and lower limbs and decreased power in bilateral upper limbs distally. In both the lower limbs, distal weakness was more prominent than proximal. Superficial reflexes were normal with bilateral plantar being equivocal. Deep tendon reflexes were absent throughout (both upper limbs and lower limbs). On extension of both upper limbs, tremor was noticed. There was loss of vibration sense throughout the body and loss of joint position sense of bilateral big toe and ankle joint. Foot drop of his left lower limb was noticed. There was no Autonomic Nervous System (ANS) involvement, and no cranial nerve involvement. Other systemic examination of cardiovascular system, respiratory system and abdomen were unremarkable.
Blood tests like complete blood count, serum electrolytes, kidney function tests, liver function tests, glucose panel were within normal limits, urine examination was normal with no proteinuria and urine Bence Jones proteins were negative. Hepatitis and Human Immunodeficiency Virus (HIV) results were negative. The thyroid profile suggested subclinical hypothyroidism. Other findings were hypocalcaemia, hypoalbuminemia and increased serum beta 2 microglobulin (3316 ng/mL).
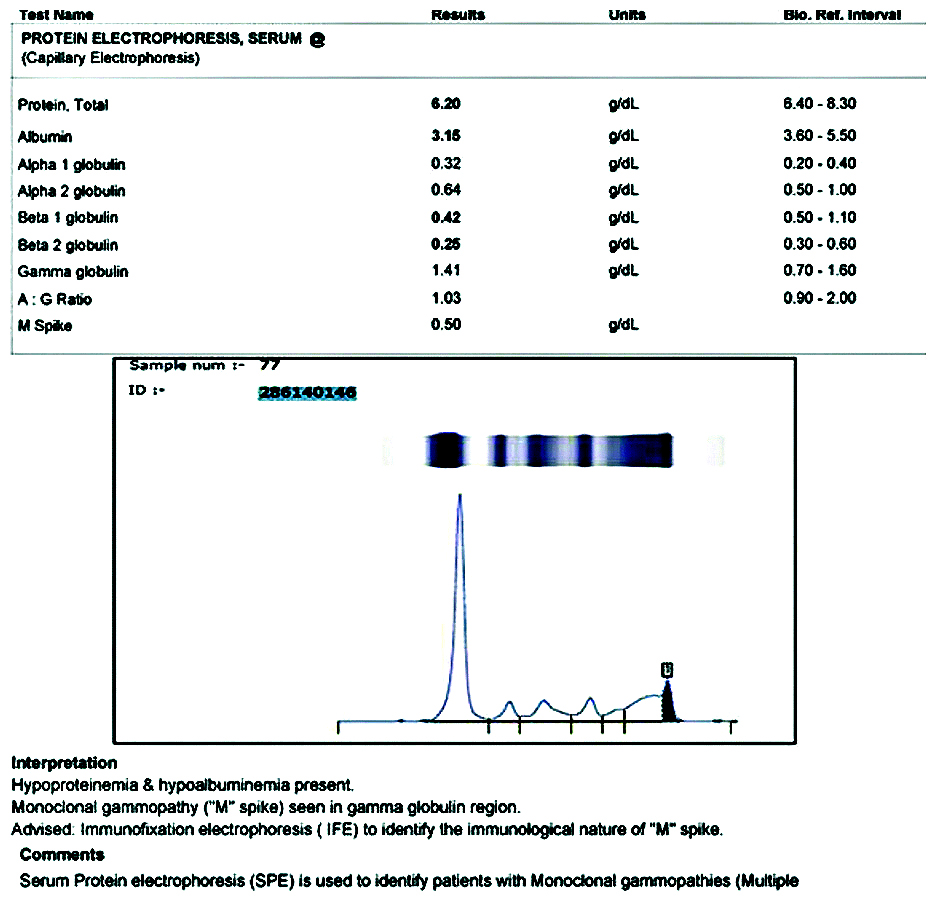
Cerebrospinal Fluid (CSF) analysis showed acellularity with an elevated protein level- 165 mg/dL. There was increased serum kappa free light chain (41.40 mg/L), lambda free light chain (79.60 mg/L) and kappa/lambda ratio (0.520). Protein electrophoresis showed hypoproteinemia (total protein- 6.20 g/dL; albumin- 3.15 g/dL). Serum protein profile, by high-resolution agarose gel electrophoresis, revealed the presence of a densely staining discrete protein band suggestive of ‘M’ spike in gamma globulin region [Table/Fig-1]. Immunofixation electrophoresis [Table/Fig-2] identified the ‘M’ spike as IgG, lambda. Electrodiagnostic studies of upper limbs showed prolongation of distal latency of bilateral median and ulnar nerves, bilateral median and ulnar conduction block of 25-50% at non-compressive sites, distal latency prolonged to >125% of upper limit normal, conduction velocity of bilateral median and ulnar nerve of >80% of lower limit normal, ‘F’ waves in both upper limbs were prolonged to >125% of upper limit normal. Electrodiagnostic studies of bilateral lower limbs showed absent Compound Muscle Action Potential (CMAP), and absent Sensory Nerve Action Potential (SNAP).
Agarose gel electrophoresis showing densely staining discrete protein band suggestive of ‘M’ spike in gamma globulin region.
T5: Bacteriophage; G: Immunoglobulin G; A: Immunoglobulin A; M: Immunoglobulin M; K: Kappa; L: Lambda
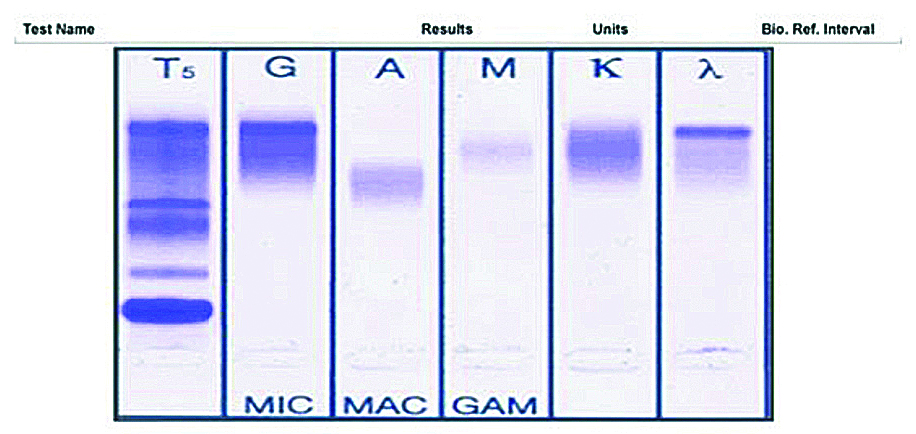
Serum protein electrophoresis showing M spike.
X-ray skull and spine were normal with no evidence of osteolytic lesions. Ultrasound abdomen was normal. Since the patient had no signs, symptoms and no clinical evidence suggesting Multiple Myeloma (MM), bone marrow examination was deferred and he was diagnosed with CIDP with Monoclonal Gammopathy of Undetermined Significance (MGUS). He was discharged on oral glucocorticoid (prednisone 60 mg once daily) and was advised regular follow-up to check for progression to MM.
Discussion
Monoclonal gammopathies consist of clonal plasma cell disorders like MGUS, MM and Waldenstrom’s Macroglobulinemia (WM), and CIDP has been associated with them [1]. The most common presentation of neuropathy in MM is a mild, symmetric sensory loss more than motor losses, distal involvement greater than proximal [1]. While IgG is the most common monoclonal gammopathy, as seen in the above case, IgM accounts for more than 50% of paraprotein-associated demyelinating neuropathies [1]. MGUS is associated with neuropathy, shows specific clinical, electrophysiologic and pathologic features [2]. About 5-10% of patients, with otherwise unexplained polyneuropathy, have a monoclonal gammopathy (mostly an IgM type). Neuropathy related to IgA or IgG MG is less common [3].
Mathis S et al., have reported a case with mild distal motor deficit of the lower limbs (flexion and extension of feet and toes were weak) without amyotrophia. Deep tendon reflexes were absent at ankles and had no pyramidal or sphincter disturbance. Same was observed in the present case as the patient had distal motor weakness with absent deep tendon reflexes and no sphincter disturbance. The electrophysiological study of the above cited case report and the index patient showed a primary demyelinating sensorimotor polyneuropathy, with no SNAP and no CMAP in the lower limbs [3].
Colucci G et al., reported a similar case that had a 4-week history of progressive muscle weakness, gait ataxia, perioral paresthesia, and subjective swallowing difficulties. The neurologic examination revealed normal cranial nerves-proximal rather than distal paresis with diffusely absent reflexes and mild lower limb sensory deficiencies. CSF analysis showed increased protein and normal cell count, similar to the present case study [4].
The diagnostic tools are blood investigations, CSF analysis, radiological imaging and electrodiagnostic studies. In the above mentioned case, patients CSF analysis showed elevated protein levels with no cells and his electrodiagnostic study was conclusive of bilateral demyelinating type of sensory motor polyradiculopathy. While many patients respond to current immunosuppressive treatment, some do not, leading to lasting disability [5]. As second line therapy, biologicals like rituximab, immunosuppressant/immunomodulatory drugs may be considered when patients do not respond adequately to plasmapheresis/intravenous immunoglobulin (IV Ig) [6].
Conclusion(s)
Diagnosis of CIDP and its underlying cause depends on thorough clinical examination and varied investigations. Since, CIDP is associated with MM, MGUS and other paraproteinemias, clinically finding out this association is important. As in this case, the association of CIDP with MGUS was made and patient has been kept on follow-up to assess the progression of Monoclonal Gammopathy of Undetermined Significance (MGUS) to MM.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 14, 2020
Manual Googling: Jan 13, 2021
iThenticate Software: Feb 03, 2021 (9%)
[1]. Fasanya AA, Loncharich MF, Gandhi V, Rana S, Balaan M, Multiple myeloma associated chronic inflammatory demyelinating polyradiculoneuropathy: The importance of continued surveillanceCureus 2016 8(11):e899Published 2016 Nov 2810.7759/cureus.899 [Google Scholar] [CrossRef]
[2]. Ramchandren S, Lewis RA, An update on monoclonal gammopathy and neuropathyCurr Neurol Neurosci Rep 2012 12(1):102-10.10.1007/s11910-011-0237-422090258 [Google Scholar] [CrossRef] [PubMed]
[3]. Mathis S, Franques J, Richard R, Jean-Michel V, Monoclonal gammopathy of undeterminated significance and endoneurial IgG depositionMedicine 2016 95(36):e480710.1097/MD.000000000000480727603395 [Google Scholar] [CrossRef] [PubMed]
[4]. Colucci G, Pabst T, Bacher U, Maggioli C, Zecca C, Gobbi C, A case of CIDP concurrent with MGUS IgG kappa responsive to autologous stem cell transplantationNeurol Neuroimmunol Neuroinflamm 2020 7(6):e88810.1212/NXI.000000000000088832934013 [Google Scholar] [CrossRef] [PubMed]
[5]. Mathey EK, Park SB, Hughes RA, Pollard JD, Armati PJ, Barnett MH, Chronic inflammatory demyelinating polyradiculoneuropathy: From pathology to phenotypeJ Neurol Neurosurg Psychiatry 2015 86(9):973-85.10.1136/jnnp-2014-30969725677463 [Google Scholar] [CrossRef] [PubMed]
[6]. Roggenbuck JJ, Boucraut J, Delmont E, Conrad K, Roggenbuck D, Diagnostic insights into chronic-inflammatory demyelinating polyneuropathiesAnn Transl Med 2018 6(17):33710.21037/atm.2018.07.3430306076 [Google Scholar] [CrossRef] [PubMed]