Collection of pus like material in hepatic soft tissue which is either due to microorganisms, fungal or mixed infection is known as liver abscess [1]. Liver abscess had been recognised as early as during the times of Hippocrates (400 BCE). In spite of all the advancements in modern practice, liver abscess if not treated on time can even lead to death, especially in tropical countries like India [2]. There are two liver abscess one is amoebic liver abscess due to Entamoeba histolytica and second is pyogenic liver abscess which is often polymicrobial [3]. In developed countries pyogenic liver abscess is more common, but in developing and underdeveloped countries like India, Bangladesh amoebic liver abscess is more likely to cause this disease [3]. The contributing factors are increased alcohol intake, malnutrition, poor personal hygiene, inadequate sanitary conditions and overcrowding which is more common in these areas [4]. Imaging techniques like USG or CT are useful in diagnosis of liver abscess. USG findings in pyogenic abscess are having irregular margins and a hypo echoic lesion. Gas within the abscess cavity is found and the presence of micro bubbles or diffuses hyper echoic spots [4-6]. For pyogenic liver abscess combination of both antibiotic therapies such as metronidazole, cephalosporins and adequate drainage are useful for the treatment. It can be done surgically either by laparoscopic, percutaneous or by open approach [6]. Patients with appropriate clinical condition and those who have a single lesion or micro abscesses of less than 2 cm in diameter are best managed conservatively. Antibiotics are to be continued for 4-6 weeks [2,4]. Drainage of the abscesses either by percutaneous needle aspiration or percutaneous catheter drainage is the mainstay of the treatment. “Source control” is an essential part of the surgical treatment of pyogenic liver abscess [6].
Rural areas have limited access to basic utilities such as electricity, running water and sewage. Therefore, this study was planned to analyse the occurrence of liver abscesses according to patient demographics. The study also aimed to identify a fast and a precise diagnosis of liver abscess and to evaluate the most effective treatment modality.
Materials and Methods
This prospective clinical study was done at rural tertiary care centre SGT Medical College, Gurugram, Haryana, India, from November 2018 to April 2020. A total of 60 patients were included in this study. All patients were admitted to the inpatient ward of General Surgery. Prior to any intervention informed written consent was taken. The Institutional Ethical Committee approval was obtained (IEC/FMHS/F/7/12/18-7). The diagnosis of liver abscess was made based on history, clinical features, laboratory investigations like Liver Function Tests (LFT), International Normalised Ratio (INR), imaging studies like chest X-ray, abdominal USG with or without CT scan of the abdomen [7]. Serological investigations included blood for antibody ELISA kit TechLab E. histolytica II kit and stool for routine microscopy for detecting the presence of trophozoites and cyst of Entamoeba histolytica, and culture from the aspirate of abscess [8]. Patients were treated with medical treatment with or without one of the following-percutaneous needle aspiration, percutaneous catheter drainage or open surgical drainage.
Inclusion criteria: All the patients with age more than 18 years and USG or CT findings consistent with liver abscess were included in the study.
Exclusion criteria: Exclusion criteria were the patients with malignant disease of hepatobiliary system, liver diseases like alcoholic hepatitis, viral hepatitis, pregnant women, patients with previous liver transplantation.
All patients with liver abscess were given parenteral Intravenous (IV) antibiotics prior to any procedure being undertaken, inj. metronidazole (400-800) mg IV eight hourly for antiamoebic coverage and inj. ceftriaxone 1 gm IV 12 hourly for five days or were administered with piperacillin tazobactum 4.5 gm IV eight hourly. Patients on inj. metronidazole were switched to oral route (tab metronidazole 400 mg eight hourly) at the time of discharge and were given for a total of 21 days.
Depending upon the size of the abscess on USG, the patients were then given treatment based on the following protocol [9,10]:
i) Protocol 1: Abscess cavity <5 cm or volume of the cavity <100 cc (cubic centimetre), conservative treatment was given [9].
ii) Protocol 2: Abscess cavity >5 cm but <10 cm or volume of cavity >100-300 cc, percutaneous needle aspiration was done [10].
iii) Protocol 3: Abscess cavity >10 cm or volume of cavity >300 cc. Percutaneous pigtail catheter drainage was performed [10].
iv) Protocol 4: Ruptured liver abscess with peritonitis, laparotomy, evacuation of abscess cavity drainage of abscess cavity and peritoneal lavage [9].
Conservative management: All patients who had abscess size less than 5 cm or volume of cavity less than 100 cc were given inj. metronidazole (400-800) mg IV eight hourly for antiamoebic coverage and inj. ceftriaxone 1 gm IV 12th hourly for five days or were administered with inj. piperacillin tazobactum 4.5 gm IV eight hourly if they did not respond to the above treatment [9].
USG guided needle aspiration: In patients who had abscess size between 5-10 cm or volume of the cavity greater than 100 cc but less than 300 cc, USG guided percutaneous needle aspiration was done under the cover of above mentioned antibiotics and antiamoebics [10].
USG guided percutaneous catheter drainage: In patients who had an abscess size more than 10 cm or volume of the cavity greater than 300 cc, with coverage of antibiotics and antiamoebics, USG guided percutaneous catheter drainage of the abscess was done by placing 12 or 14 Fr pigtail catheter [10].
Surgery: In patients where the USG or CT showed ruptured liver abscess along with features of peritonitis, a midline laparotomy was done and the abscess cavity was then explored and evacuated. Thorough peritoneal lavage was then done and abscess cavity was drained [9].
Whenever the procedure yielded a specimen (pus during aspiration/ catheter drainage) it was promptly sent for assessing culture, sensitivity and microscopic examination.
Serial estimation of Complete Blood Count (CBC) and LFT was done if the initial reports were altered. This was continued till the reports normalised. Serial USG was done on D3, D7 and D15 and repeat intervention was done if the patient remained symptomatic along with increasing size of the abscess. The patients were discharged when they were relieved symptomatically and had a stable haemodynamic condition.
Irrespective of the day of discharge from the hospital, patients were called back and USG was repeated on D7, D15 and D30 from the day of last intervention.
Statistical Analysis
The means and standard deviations of the measurements per group were used for statistical analysis (SPSS 20.0 for windows; SPSS inc, Chicago, USA). Difference between two groups was determined using Chi-square test or Fischer-exact test and the level of significance was set at p<0.05.
Results
A total of 60 patients were included in this study. All study subjects belonged to either lower middle or lower socio-economic class with compromised hygienic environment.
The age of study population ranged from 18 to 90 years. Maximum subjects were from the age group of 41-50 years (40%). Mean age of the study subjects was 49.45±18.32 years [Table/Fig-1].
Age of population under study (N=60).
| Age group (in years) | N | % |
|---|
| 18-30 | 9 | 15 |
| 31-40 | 10 | 16.67 |
| 41-50 | 24 | 40 |
| 51-60 | 2 | 3.33 |
| >60 | 15 | 25 |
| Total | 60 | 100 |
| Age in years, Mean±SD | 49.45±18.32 |
| Median | 45.50 |
Male and female comprised of 48 (80%) and 12 (20%) of the subjects respectively, hence showing male dominance. The male: female ratio was 4:1.
Patients with liver abscess had the history of alcoholism 36 (60%) while 8 (13%) had diabetes mellitus type II and 8 (13%) were suffering from tuberculosis. Jaundice was found in 3 (5%) of the study subjects (Some study subjects had multiple co-morbidities).
In this study, pain abdomen 55 (91.67%) was the most common symptom especially in the right upper abdomen followed by fever 47 (78.33%) and vomiting 32 (53.33%) [Table/Fig-2].
Symptoms among the study subjects (n=55).
| Symptoms | n | % |
|---|
| Abdominal pain | 55 | 91.67 |
| Fever | 47 | 78.33 |
| Vomiting | 32 | 53.33 |
| Diarrhea | 16 | 26.67 |
| Loss of appetite | 11 | 18.33 |
| Cough | 10 | 16.67 |
| Nausea | 7 | 11.67 |
| Breathlessness | 5 | 8.33 |
| Weight loss | 2 | 3.33 |
| Total | 60 | 100 |
Out of 55 subjects suffering from pain; dull and vague pain was revealed in 33 (60%) and 22 (40%) subjects, respectively [Table/Fig-3].
Pain characteristics among the study subjects (N=60).
| Variables | N | % |
|---|
| Pain duration (days) |
| 3-5 | 15 | 27.3 |
| 6-10 | 14 | 25.5 |
| 11-15 | 5 | 9 |
| 15 | 21 | 38.2 |
| Type of pain (n=55) |
| Dull | 33 | 60 |
| Vague | 22 | 40 |
Tenderness was one of the most important clinical sign observed in 44 (73.33%) especially in right hypochondriac region of study subjects and pyrexia was the second most common observation found in 43 (71.67%) on admission. The less common sign was rigidity in 9 (15%). This was seen in patients who had developed peritonitis secondary to complicated/ruptured liver abscess [Table/Fig-4].
Clinical signs among the study subjects (N=60).
| Signs | N | % |
|---|
| Tenderness | 44 | 73.33 |
| Raised temperature | 43 | 71.67 |
| Hepatomegaly | 38 | 63.33 |
| Guarding | 37 | 61.67 |
| Anaemia | 27 | 45 |
| Icterus | 15 | 25 |
| Rigidity | 9 | 15 |
CBC and LFT were done in all the patients. It was found that 48 of the patients had raised serum Alkaline phosphatase (>140 IU/L). A total of 19 had (Haemoglobin <10 gm/dL). Leukocytosis (>11000 U/L) was found in 44 cases and hyperbilirubinaemia (Serum bilirubin >1.2 mg/dL) in 13 patients. Raised INR (>1.5) was found in 11 cases [Table/Fig-5].
Laboratory investigations among the study subjects (N=60).
| Laboratory investigations | N | % |
|---|
| Serum Alkaline Phosphatase >140 IU/L | 48 | 80 |
| WBC >11000/cmm | 44 | 73.33 |
| Haemoglobin <10 g/L | 19 | 31.67 |
| Total Serum Bilrubin >1.2 mg/dL | 13 | 21.67 |
| INR >1.5 | 11 | 18.33 |
WBC: White blood cells; INR: International normalised ratio
Presence of trophozoites of Entamoeba histolytica in the stool specimens was the most definitive indicator of amoebic liver abscess. Otherwise absence of the same do not mean pyogenic liver abscess as shown in [Table/Fig-6].
Routine stool examination among the study subjects.
| Trophozoites | N=60 | % |
|---|
| Present | 20 | 33.33 |
| Absent | 40 | 66.67 |
Serum antilectin antibodies were found in 23% of patients with liver abscess. Absence of serum antilectin antibodies ELISA does not mean that the study subjects were not having amoebic liver abscess [Table/Fig-7].
Outcome of ELISA among the study subjects.
| ELISA | N | % |
|---|
| Present | 14 | 23.33 |
| Absent | 46 | 76.67 |
According to radiographs [Table/Fig-8,9], right sided pleural effusion, right side diaphragm dome elevation and both were reported in 10 (16.67%), 9 (15%) and 7 (11.67%) of the subjects, respectively. The radiograph revealed abnormality among 26 (43.33%) subjects.
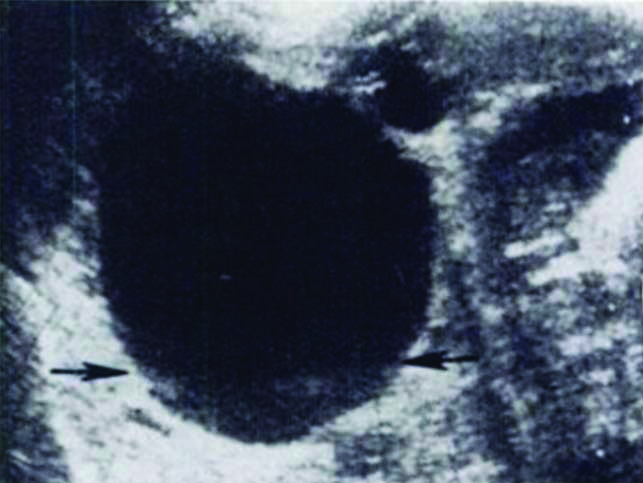
USG appearance of liver abscess with smooth, well-defined walls hypo echoic lesion and fluid-fluid interface.
CT scan appearance of liver abscess.
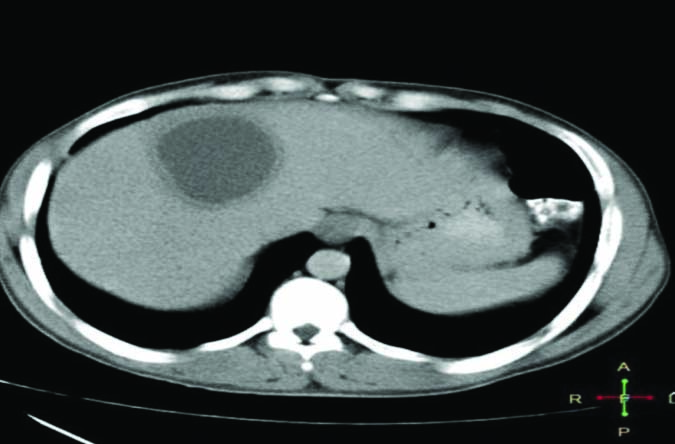
Liver abscess located in the right lobe was found in 48 (80%) of the patients. Six (10%) patients had abscess in the left lobe while 6 (10%) had the abscesses in both lobes.
In this study, 21 had (35%) abscesses size <5 cm, 23 (38%) had size >5 cm but <10 cm and 16 (27%) of the abscesses were >10 cm. Other findings that were noted in the USG included inflammation in 4 (7%) caecum and terminal ileum. A total of 21 (35%) of the patients also had pleural effusion in USG, whereas 17 (28%) had same findings in X-ray chest.
Death occurred in 2 cases (22.22%) out of nine ruptured liver abscess cases. Subjects with liver abscess up to 10 cm mostly underwent treatment for seven days while subjects, having abscess >10 cm, underwent percutaneous catheter drainage treatment for 15 days [Table/Fig-10].
Treatment outcome according to liver abscess protocol among the study subjects.
| No. of days of past treatment | Protocol |
|---|
| Protocol 1 (<5 cm) n=21 | Protocol 2 (5-10 cm) n=21 | Protocol 3 (>10 cm) n=9 | Protocol 4: Ruptured liver abscess n=9 |
|---|
| n | % | n | % | n | % | n | % |
|---|
| D3 | 4 | 19.05 | 5 | 23.81 | 0 | 0 | 0 | 0 |
| D7 | 5 | 23.81 | 12 | 57.14 | 0 | 0 | 0 | 0 |
| D15 | 9 | 42.86 | 3 | 14.29 | 7 | 77.79 | 6 | 66.67 |
| D30 | 3 | 14.29 | 1 | 4.76 | 2 | 22.22 | 1 | 11.11 |
| Death | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 22.22 |
| Fischer-exact test | 1.98 |
| p-value | 0.02* |
*statistically significant
In this study, amoebic and pyogenic liver abscess was found among 42 (70%) and 18 (30%) of the subjects respectively indicating that amoebic liver abscess is more common in this territory.
Out of 42, abdominal pain was present in 39 (92.9%) of patients with diagnosed amoebic liver abscess while 16 (88.9%) of patients with pyogenic liver abscess had abdominal pain. Fever with chills and rigors was present in 24 (57.1%) of patients with amoebic liver abscess while 9 (50%) of patients with pyogenic liver abscess had fever which was associated with chills and rigors. Blood mixed stool was found in 7 (16.7%) cases of amoebic liver abscess, while watery stool was found in 4 (22.2 %) cases of pyogenic liver abscess while mucous mixed stool was found in 3 (7%) and 2 (11%) patients with amoebic and pyogenic liver abscess, respectively with statistically significant difference.
Raised Total Leukocyte Count (TLC) was reported more in pyogenic liver abscess 16 (88.9%) as compared to amoebic liver abscess cases [Table/Fig-11].
Distribution of liver abscess among the study subjects according to total leukocyte count.
| Type | | Total leukocyte count | Total |
|---|
| Normal | Raised |
|---|
| Amoebic liver abscess | n | 14 | 28 | 42 |
| % | 33.3 | 66.7 | 100 |
| Pyogenic liver abscess | n | 2 | 16 | 18 |
| % | 11.1 | 88.9 | 100 |
| Chi-square | 3.18 |
| p-value | 0.07 |
No microorganism was reported among cases of amoebic liver abscess while Escherichia coli, Klebsiella pneumoniae and Staphylococcus aureus was reported in 4 (22.2%), 3 (16.7%), and 7 (38.9%) of the subjects belonging to pyogenic liver abscess, respectively while 4 (22.2%) showed no growth.
Positive ELISA test and trophozoites was found only in cases of amoebic liver abscess i.e., 14 (33.33%) and 20 (47.61%) respectively [Table/Fig-12].
Distribution of liver abscess among the study subjects according to ELISA and Stool for Routine Microscopy.
| Symptoms | Amoebic liver abscess (n=42) | Pyogenic liver abscess (n=18) | p-value (Chi-square) |
|---|
| n | % | n | % |
|---|
| ELISA | 14 | 33.33 | Nil | 0 | <0.01* |
| Stool for routine microscopy (Trophozoites) | 20 | 47.61 | Nil | 0 | <0.01* |
*statistically significant
Death was reported in subjects with amoebic liver abscess in only i.e., 2 cases. Days taken for resolution of symptoms were comparable in subjects with amoebic as well as pyogenic liver abscess (p>0.05) [Table/Fig-13].
Distribution of liver abscess among the study subjects according to resolution of symptoms.
| Type | | Resolution of symptoms (in days) |
|---|
| Death | 3 Days | 7 Days | 15 Days | 30 Days |
|---|
| Amoebic liver abscess | n | 2 | 7 | 9 | 20 | 4 |
| % | 4.8 | 16.7 | 21.4 | 47.6 | 9.5 |
| Pyogenic liver abscess | n | 0 | 1 | 8 | 6 | 3 |
| % | 0 | 5.6 | 44.4 | 33.3 | 16.7 |
| Chi-square | 5.52 |
| p-value | 0.36 |
Discussion
Liver abscess is a common disease that is encountered in surgical Out Patient Department (OPD) and emergencies situated in outskirts of Haryana due to its variable presentations and hence pose a challenge. Liver abscess is associated with up to 20% mortality. Interestingly, in developing nations, amoebic liver abscess is more common [11].
In this study, amoebic liver abscess was reported among 42 (70%), and rest were pyogenic and were more common in right lobe of liver. Similarly Jha AK et al., revealed that out of the total 125 patients screened, 110 (88%) had amoebic liver abscess and 15 (12%) had pyogenic liver abscess [12]. These results were consistent with the previous reports by Sharma N et al., and Mukhopadhyay M et al., on amoebic liver abscess [13,14].
Age: In present study, maximum subjects belonged to the age group of 41-50 years (40%) followed by >60 years (25%). Verma M and Arora BK in their study too found that maximum subjects were in the age group of 40-49 years [15].
Gender: Male and female patients comprised of 80% and 20% of the subjects respectively, hence showing male dominance in the present study, which has been globally observed [2]. In a study by Verma M and Arora BK, 32 cases were male and three cases are female and sex incidence, ratio being, male: female was 10.6:1 [15].
Personal history: History of alcohol intake was found among 60% of the subjects respectively in the present study. Alcohol has been identified as a major predisposing factor in the pathogenesis of amoebic liver abscess. Similar study conducted by Siroliya A et al., showed that around 68% of study subjects had history of alcoholism thus, it came out to be major predisposing factor for the liver abscess [7]. Similar observations were reported by Ramani A et al., and various other researchers [16]. Jha AK et al., reported 33.64% of the amoebic liver abscess and 60% of the pyogenic liver abscess patients were diabetic [12]. Among this patient group, the higher frequency of liver abscesses in diabetics could be attributed to lower immunity. While in this study 14.28% of amoebic liver abscess and 11.11% of pyogenic liver abscess had diabetes mellitus type II.
Symptoms: In the present study abdominal pain and fever with chills and rigors was comparable among subjects with amoebic and pyogenic liver abscess, though both symptoms were slightly more in subjects with amoebic liver abscess. Stools mixed with blood was found in cases of amoebic liver abscess, while watery and mucoid discharge was reported in cases of pyogenic liver abscess with statistically significant difference (p-value <0.005). Similarly the study conducted by Siroliya A et al., showed that pain abdomen was more (90%) in patients with amoebic liver abscess and (70%) as compare to the patients with pyogenic liver abscess while fever was present in 92% and 88%, respectively [7].
Clinical signs: In this study, tenderness, pyrexia was reported among 73.33%, 71.67% of the subjects, respectively. Siroliya A et al., in their study revealed that tenderness and pyrexia were the most common clinical signs [7].
Laboratory investigations: Serum alkaline phosphatase >140 IU/L, WBC >11000/cmm, haemoglobin <10 gm%, Total Serum Bilirubin >1.2 mg/dL and INR >1.5 was found among 80%, 73.33%, 31.67%, 21.67% and 18.33% of the subjects, respectively in this study. In this study, raised TLC was reported more in pyogenic liver abscess (88.9%) as compared to amoebic liver abscess cases. Similarly Jha AK et al., in their study reported that leukocytosis (TLC >10,000/cumm) was present in all the cases of pyogenic liver abscess [12]. Siroliya A et al., in their study reported that leukocytosis (TLC >11,000/cumm) was present in around 73% of their subjects, anaemia (Hb <8 gram%) present in 72% of their subjects, Serum alkaline phosphatase was raised (>120 IU) present in 75% of cases, raised Bilirubin (>1.5 mg/dL) was present in 13% of subjects [7].
Trophozoites: In this study, according to stool examination, trophozoites were present in 20 (47.16%) out of 42 patients with diagnosed amoebic liver abscess but no results were found out to be positive in patients having pyogenic liver abscess. Sayek I and Onat D (2001) found that trophozoites were present in 25% of the patients [2].
ELISA test: ELISA for the demonstration of antiamoebic antibody in titres greater than 1:400 is considered strong evidence of amoebic liver abscess. ELISA test was positive among 14 (33.33%) out of 42 subjects in the present study but no results were found out to be positive in patients having pyogenic liver abscess. In other study conducted by Haque R et al., reported that 13/23 patients diagnosed amoebic liver abscess were tested positive against serum antilectin antibody without prior treatment with metronidazole [8]. In contrary to present study blood ELISA for antibody Entamoeba histolytica is not in favour of diagnosing amoebic liver abscess patients as antilectin antibodies were not formed in the present study population and those with positive results had taken the treatment for liver abscess prior to admission in the hospital which responded to treatment with metronidazole and developed the antibodies against the disease. Jha AK et al., revealed similar findings in their study [12].
Pus culture sensitivity: In the present study, no microorganism was reported among amoebic liver abscess while Escherichia coli, Klebsiella, and Staphylococcus aureus were reported in 22.2%, 16.7% and 38.9% of the subjects, respectively. In a study by Siroliya A et al., pus culture was positive in around 70% of cases of pyogenic liver abscess respectively, Escherichia coli and Klebsiella were the most common organisms cultured and of which Escherichia coli was more common than Klebsiella [7]. Jha AK et al., in their study found that the main aetiology of pyogenic liver abscess in their study was E. coli (60% cases) while in other studies Klebsiella pneumoniae was most common organism [12].
Radiograph diagnosis: According to radiograph diagnosis, right dome elevation, right pleural effusion and both was reported in 15%, 16.67% and 11.67% of the subjects, respectively. Radiograph chest revealed abnormality among 26 (43.33%) subjects in this study. Similar findings were reported by Verma M et al., i.e., 16 (45.71%) cases had elevated right dome of the diaphragm with restricted movements. Sixteen (45.71%) cases had right side pleural effusion [15].
Size of abscess: Size of abscess <5 cm, 5-10 cm and >10 cm was reported among 35%, 38% and 27% of the subjects, respectively in this study. Similar study conducted by Khan R et al., reported that size of abscess cavity <5 cm was present in 34% of the study subjects while >5 cm was present in 66% [17].
Treatment outcome: In this study death was reported among 2 cases (22.22%) out of nine ruptured liver abscess cases. Subjects with liver abscess upto 10 cm were mostly treated for seven days while subjects having abscess >10 cm, underwent treatment for 15 days. When treatment outcome was compared according to the size of liver abscess, it was found to be statistically significant (p<0.05) in this study. Death was reported only in subjects with ruptured amoebic liver abscess i.e., two cases. Time taken for resolution of symptoms were comparable in subjects with amoebic as well as pyogenic liver abscess as p>0.05. In a study by Siroliya A et al., mortality rate was 8%. Mortality rate was more in case of pyogenic liver abscess (15%) as compared to that of amoebic liver abscess (5%) as the associated risk factors are also more common in case of pyogenic liver abscess [7]. These findings are contrary to present finding as no death occured in pyogenic liver abscess in present study. Jha AK et al., showed that 103 patients with amoebic liver abscess (93.63%) were treated successfully. Mortality was there in seven patients (6.36%) [12]. Interestingly, all patients with pyogenic liver abscess were treated successfully and subsequently discharged. Similarly, in this study 40 patients with amoebic liver abscess (95.23%) were treated successfully and mortality was there in two cases and all patients with pyogenic liver abscess were treated successfully.
Initially, open procedures such as laparotomy was the main stay of treatment in patients diagnosed with liver abscess but with rise in imaging as well as microbiological investigations and antibiotics shifted the approach more towards conservative as well as in the favour of minimal invasive procedures. USG guided aspiration or pig tail catheter drainage of these abscesses has replaced surgical intervention as the procedure of choice if performed carefully and most of the patients in which needle aspiration was performed had decreased hospital stay in comparison to Percutaneous Catheter Drainage (PCD) and laparotomy was performed. Laparotomy should only be reserved for those who developed peritonitis.
Limitation(s)
This was a short study conducted over a shorter span and there was no definitive test to diagnose various types of liver abscesses. Many a time one has to depend on the clinical history and physical appearance of the pus to start the treatment.
Conclusion(s)
Liver abscess is a common problem especially in middle age population and is more common in men. Imaging modalities like CT scan, abdominal sonography along with history and clinical examination has led to an early diagnosis of liver abscess. Microscopic examination of stool is useful in detecting trophozoites in amoebic liver abscess. In endemic countries like India, blood antibody ELISA for Entamoeba histolytica is not in favour of diagnosing amoebic liver abscess patients as antilectin antibodies were not formed in the present study population and those with positive results had taken the treatment for liver abscess prior to admission in the hospital which responded to treatment with metronidazole and developed the antibodies against the disease. Conservative management is suitable for minor abscesses. However, medical management plus intervention such as catheter drainage (compared to needle aspiration) results in high cure rates for larger abscesses (>300 cc) and left lobe abscesses, while the surgical intervention reserved for complications such as peritonitis.
WBC: White blood cells; INR: International normalised ratio
*statistically significant
*statistically significant