Injuries to the radial nerve can be divided into high or complete radial nerve injuries and low or Posterior Interosseous Nerve injury (PIN injury). Most injuries occur distal to the triceps muscle innervation [2]. Loss of radial nerve function results in deficient grip as a result of loss of extension of wrist, thumb and metacarpophalangeal joints of fingers [6]. Sensory loss is invariably confined to the skin over the anatomical snuffbox and rarely disturbs the patient unless a neuroma is formed [7].
Primary nerve repair or neurorrhaphy offer the patients the best chance to achieve good recovery. Alternative surgical procedures are indicated when direct nerve repair is not feasible owing to substantial gap between the nerve ends. The procedures are reverse interposition autologous nerve grafts or venous conduits. Subjects who present late in the disease, at about two years, may not have motor recovery as the axons of the proximal nerves fail to innervate the muscle. Moreover, if the patients presented earlier and the damaged radial nerve does not show neural recovery following conservative or surgical repair, tendon transfer is considered the standard treatment [6].
So, authors aim to study Zachary’s modification of Jones tendon transfer for high radial nerve palsy. Jones transfer used both Flexor Carpi Radialis (FCR) and FCU decreasing the flexion power of the wrist. Zachary’s modification involved motorisation of metacarpophalangeal (MCP) joint extensors only by FCU. The study also aimed to evaluate validity of the procedure, technical finesse along with the critical analysis of the procedure.
Materials and Methods
In this retrospective cohort study, the clinical records of three years (January 2017-December 2019) were explored and the files of patients with radial nerve palsy were sorted. The study was designed in the Department of Plastic Surgery of an Apex Trauma Centre in Eastern Uttar Pradesh. A total of 26 patients with isolated high radial nerve palsy formed the study sample and their detailed analysis was carried out. This research was conducted in accordance with the principles of the Declaration of Helsinki [8]. Due to the retrospective nature of the study, the ethical approval could not be obtained.
Patients either presented late in the disease or underwent primary surgery which eventually failed. The selection, therefore, depended on the requirement of tendon transfers.
Inclusion criteria
The patients with wrist and finger drop [Table/Fig-1] who were managed conservatively for three months to overcome the period of neuropraxia.
Hand drawn diagram depicting radial nerve palsy specially wrist drop and flexion at metacarpophalangeal joints.

Supple wrist and finger joints without contractures.
Any joint stiffness was managed by aggressive passive physiotherapy in order to maximise surgical outcome.
Exclusion criteria
Non-functioning donor tendons such as those found in global brachial plexus injury.
Concurrent median and ulnar nerve injury.
Absent Palmaris Longus (PL)- prompted the use of Flexor Digitorum Superficialis (FDS) of ring finger (FDS III) [4].
Weak FCU.
Pronator Teres (PT) injury in fractures around elbow or in forearm.
Children <10 years as they were not compliant to rigorous postoperative physiotherapy.
Stiff hand joints with no passive movements.
Uncontrolled diabetes mellitus or severe co-morbidities.
Anticoagulants, if any, were discontinued a week prior to operation.
Surgical Details of Zachary’s Tendon Transfer
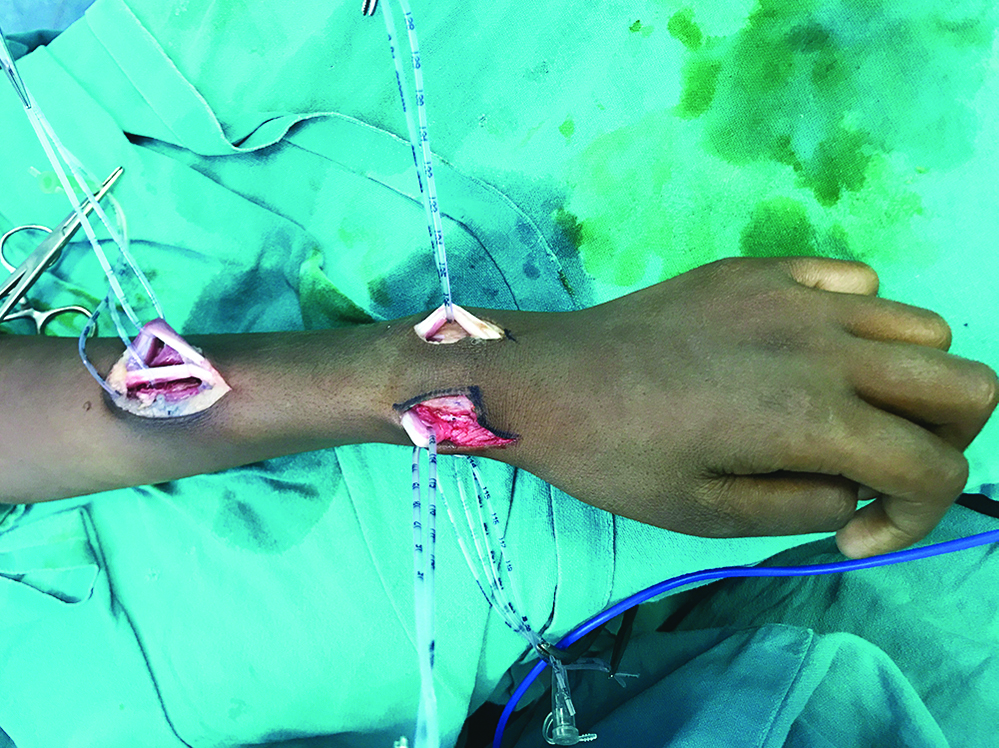
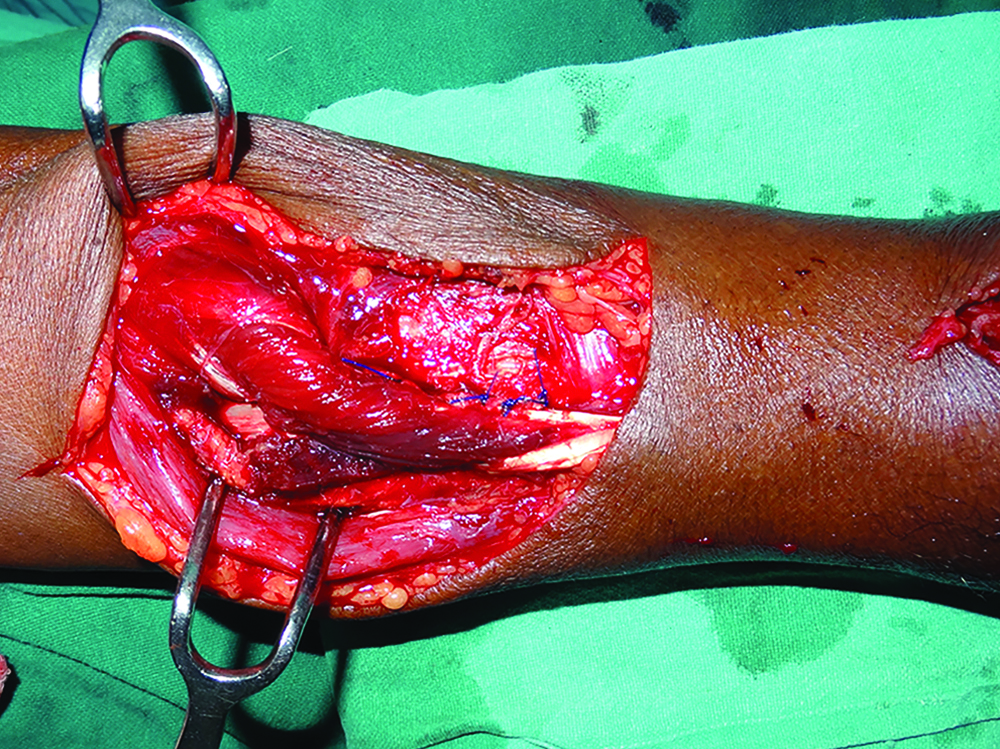
Surface marking and structural as well as functional identification of the tendons was an important aspect of preoperative planning. The patients were operated with arm abducted taking tourniquet control. The surgery was performed under magnification. A 6-8 cm lazy ‘S’ incision was given on the middle third of the lateral surface of the radius to expose the Pronator Teres (PT). The skin flaps were mobilised by undermining in the subcutaneous plane. Through the same incision Extensor Carpi Radialis Longus (ECRL) and Extensor Carpi Radialis Brevis (ECRB) were identified more posteriorly and dissected. Palmaris Longus (PL) was dissected by two small volar transverse or vertical incisions along the tendon. FCU was exposed by two tranverse incisions on the medial lower forearm. The FCU tendon identified and dissected over a pair of artery forceps upto the musculotendinous junction for adequate mobilisation but meticulously preserving ulnar nerve. The Extensor Pollicis Longus (EPL) and Extensor Digitorum Communis (EDC) were exposed by horizontal incisions in the distal forearm proximal to the extensor retinaculum and dissected upto the musculotendinous junction [Table/Fig-2,3]. Every effort should be made to clear the fascia surrounding extensor tendons while preserving extensor retinaculum. This exercise facilitated tendon gliding and prevented bowstringing.
Anterior lower forearm with dissection of Palmaris Longus (PL) as well as Flexor Carpi Ulnaris (FCU) by a vertical incision.

Posterior forearm showing the dissected Pronator Teres (PT) more medially and also Extensor Carpi Radialis Brevis (ECRB) in the proximal half. Also dissected in the distal forearm are Extensor Pollicis Longus (EPL) and Extensor Digitorum Communis (EDC) by small longitudinal incisions.
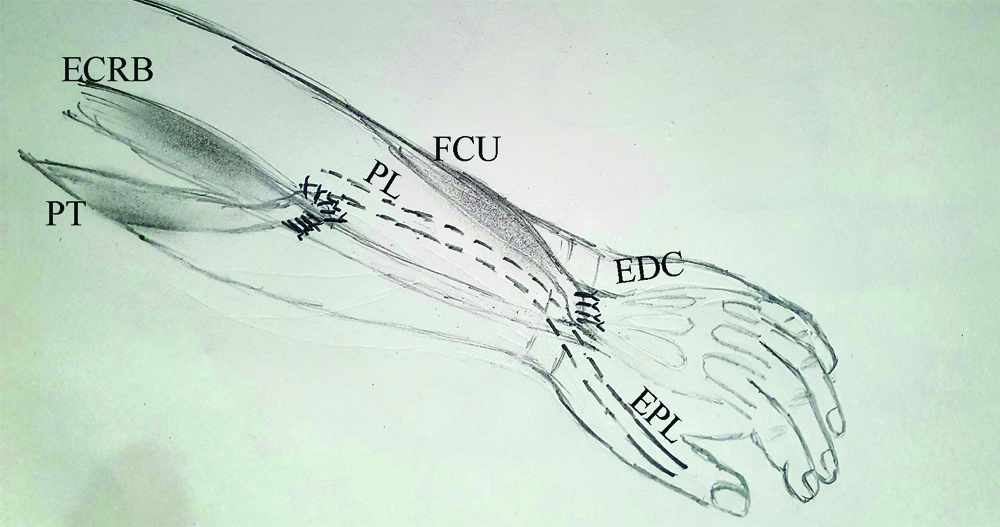
Following the dissection and mobilisation of donor tendons, the tendons were prepared for transfer. A 3-4 cm of periosteum was elevated along with dis-inserted PT as a single tendon unit and transferred end to side to ECRB, thus restoring wrist extension. PL was severed as far distally as possible and mobilised adequately. It was transferred to the re-routed EPL for thumb extension. FCU which was a bulky tendon had a tendency to retract. It was severed distally and mobilised proximally upto musculotendinous junction. This provided adequate length of tendon which was then re-routed through the ulnar aspect of forearm to the dorsal aspect and transferred to all the four slips of EDC and Extensor Indicis Proprius (EIP) [Table/Fig-4]. The tendons transferred were sutured by the Pulvertaft weave technique using 4/0 non-absorbable sutures [Table/Fig-5].
Schematic diagram describing the tendon transfer for radial nerve palsy. End to side suturing of PT-ECRB transfer. Rest of the tendons were transferred in the end to end fashion.
PL: Palmaris longus; FCU: Flexor carpi ulnaris; ECRB: Extensor carpi radialis brevis; PT: Pronator teres; EPL: Extensor pollicis longus; EDC: Extensor digitorum communis
Suturing of Pronator Teres (PT) to Extensor Carpi Radialis Brevis (ECRB) using the Pulvertaft technique.
Tension on the sutures was important as it determined the functional outcome of surgery. The wrist was kept in 30° extension with thumb and fingers just short of full extension. The forearm was immobilised in volar cast with elbow flexed and distal joints in maximal extension for a period 3 weeks, after which, assisted physiotherapy was started. A customised volar splint was fabricated to be used in the interval between the sessions of physiotherapy. At six weeks, assistance was sought from the physiotherapist and patients were advised to use splints only at night. Active movements of joints were permitted after 10-12 weeks which were monitored by fortnightly visits.
The 26 patients who underwent Zachary’s tendon transfers were evaluated by Bincaz [9] scoring system which consisted of quantitative and qualitative variables. Qualitative outcome of the tendon transfer was assessed by subjective interpretation of results ranging from excellent to poor. Quantitative outcomes were studied by the degree of wrist movement, metacarpophalangeal joint extension of fingers and opening of first web space.
Statistical Analysis
For interpretation of the quantitative variables mean, standard deviation, minimum, and maximum values were used.
Results
A total of 26 patients with high radial nerve paralysis who required tendon transfers were studied in detail [Table/Fig-6]. Patients age range was between 18 to 63 years with average age 38±13.67 years. Half the patients were aged 36 years or less. Patients presented for plastic surgical consultation after 115.54±29.27 days and as late as even 172 days following injury. Only 6 patients consulted within three months of injury. Out of total, 21 patients (80.77%) who sustained high velocity trauma and subsequent humeral fracture, six had iatrogenic injury during open fixation of fractures while 15 patients sustained high radial nerve palsy resulting from the trauma itself. Five patients having compound fractures were treated by primary neurorrhaphy but were planned for tendon transfer owing to failure of nerve repair. Three patients sustained intermediate range firearm injury without fractures. Two patients had stab injury to the arm and were managed by primary nerve repair that failed. These patients were also considered for tendon transfer.
Demographic details and surgical outcome of 26 patients.
| Sl. No. | Age (years) | Laterality | Aetiology | Presentation (days) | Radial nerve repaired | Donor tendons | Bincaz score | Significant functional deficit |
|---|
| 1 | 34 | Right | Fracture shaft humerus | 169 | No | PT, FCU. PL | 9 | - |
| 2 | 52 | Left | Fracture shaft humerus | 156 | No | PT, FCU. PL | 7 | - |
| 3 | 43 | Right | Fracture shaft humerus | 108 | No | PT, FCU. PL | 8 | - |
| 4 | 39 | Right | Firearm injury | 112 | No | PT, FCU. FDS III | 4 | Significant loss of thumb extension |
| 5 | 53 | Left | Fracture shaft humerus | 150 | No | PT, FCU. PL | 7 | - |
| 6 | 24 | Left | Fracture shaft humerus | 116 | No | PT, FCU. PL | 8 | - |
| 7 | 48 | Right | Fracture shaft humerus | 117 | No | PT, FCU. PL | 7 | Moderate loss of thumb extension |
| 8 | 62 | Left | Fracture shaft humerus | 106 | No | PT, FCU. PL | 8 | - |
| 9 | 36 | Right | Fracture shaft humerus | 128 | No | PT, FCU. PL | 9 | - |
| 10 | 51 | Right | Fracture shaft humerus | 172 | No | PT, FCU. PL | 7 | - |
| 11 | 33 | Left | Fracture shaft humerus | 134 | No | PT, FCU. PL | 8 | - |
| 12 | 29 | Right | Fracture shaft humerus | 96 | Yes | PT, FCU. PL | 8 | - |
| 13 | 63 | Right | Stab injury | 64 | Yes | PT, FCU. PL | 9 | - |
| 14 | 26 | Right | Fracture shaft humerus | 116 | No | PT, FCU. PL | 7 | Extension loss of little finger |
| 15 | 48 | Right | Fracture shaft humerus | 78 | Yes | PT, FCU. FDS III | 8 | - |
| 16 | 59 | Left | Fracture shaft humerus | 72 | Yes | PT, FCU. PL | 5 | Limitation of wrist extension |
| 17 | 22 | Right | Fracture shaft humerus | 134 | No | PT, FCU. PL | 8 | |
| 18 | 43 | Left | Firearm injury | 89 | Yes | PT, FCU. PL | 9 | - |
| 19 | 18 | Left | Fracture shaft humerus | 168 | No | PT, FCU. PL | 8 | - |
| 20 | 27 | Right | Fracture shaft humerus | 86 | Yes | PT, FCU. FDS III | 8 | - |
| 21 | 34 | Right | Stab injury | 88 | Yes | PT, FCU. PL | 4 | Significant loss of thumb extension |
| 22 | 52 | Left | Fracture shaft humerus | 95 | No | PT, FCU. PL | 9 | |
| 23 | 22 | Left | Fracture shaft humerus | 131 | No | PT, FCU. PL | 7 | Moderate loss of thumb extension |
| 24 | 24 | Right | Fracture shaft humerus | 98 | No | PT, FCU. PL | 8 | - |
| 25 | 20 | Left | Fracture shaft humerus | 113 | No | PT, FCU. PL | 9 | - |
| 26 | 26 | Right | Firearm injury | 116 | No | PT, FCU. PL | 8 | |
FC: Flexor carpi ulnaris; PT: Pronator teres; PL: Palmaris longus; FDS III: Flexor digitorum superficialis III
Bincaz score was used for evaluation of results following Zachary’s tendon transfer [Table/Fig-7]. Seventeen patients rated the results as excellent, 6 had good results and 3 had fair results [Table/Fig-8,9]. The patients were cheerful with the tendon transfer as they obtained appreciable wrist extension of 42.6°±6.64° while incomplete extension (20°) was seen in only one patient. A summary of various movements of hand joints and their quantitative analysis has been summarised in [Table/Fig-10].
Bincaz score for assessment of tendon transfers for radial nerve palsy.
| Points | 3 | 2 | 1 | 0 |
|---|
| Wrist extension | | >29° | 0-29° | <0° |
| Metacrpophalangeal joint extension | | Full | Extension loss <100 | Extension loss >100 |
| First web space opening | | >39° | Between 30=39° | <30° |
| Patient satisfaction | Excellent | Good | Fair | Bad |
Excellent ≥8, Good 6-7, Fair 4-5, Bad ≤3
Interpretation of the Bincaz score: If the patient is able to perform wrist extension >29°, full extension of metacarpophalangeal joint and first web space opening between 30 to 39°. He is fully satisfied with the outcome of the surgery and has already returned to work. These made the score is 8 points, showing the functional outcome is Excellent
Postoperative medial view showing good wrist extension (50°) and metacarpophalangeal joint extension (<10° deficient of full extension).
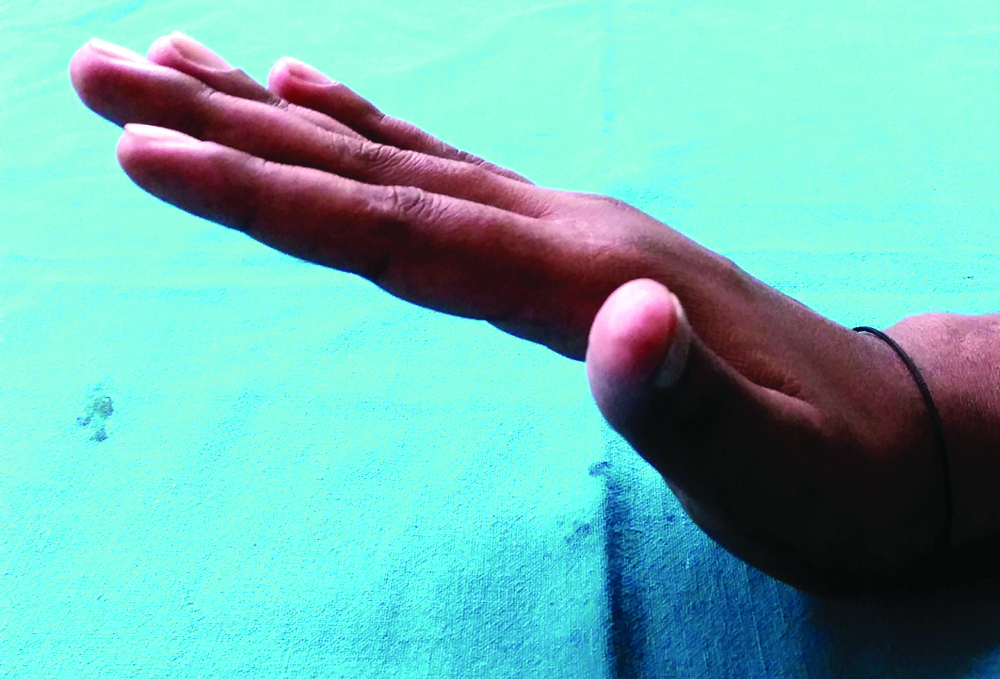
Postoperative photograph showing good thumb extension and first web space opening of 60°.

Results of our study involving Zachary’s modification of Jones tendon transfers for radial nerve palsy.
| Function | Result | Range |
|---|
| Wrist extension with MCP joints extended | 48.6°±9.64 | 20°-60° |
| Wrist flexion with clenched fist | 54.8°±10.25 | 30°-70° |
| Deficit in MCP joints extension | 18°±6.78 | 10°-40° |
| Radial extension of thumb at the basal joint | 37.6°±7.51 | 14°-45° |
| Palmar abduction and interphalangeal joint extension of thumb | No deficit | Normal |
Short term complications such as wound infection and suture line necrosis were seen in two patients. A tight PT-ECRB transfer restricted wrist flexion in two patients. The most common functional complication was incomplete thumb extension of varied severity in four patients. In addition, MCP joint extension loss of little digit was observed in one patient while wrist extension of only 20° was seen in one patient. Patients with functional deficits improved on physiotherapy to a large extent. Surgery was required if unsatisfactory progress was observed in thumb extension and consisted of PL-EPL plication. Average follow-up was 33.2±2.11 (22-41 months) in patients on regular visits for possible complications.
Discussion
Tendon transfer for radial nerve palsy was described by Jones R, over 100 years ago who described the entity as “fingers to curl into the palm, and the hand to become useless” [10]. It consisted of the transfer of PT into the radial extensors of the wrist, FCU into the extensors of the third, fourth, and fifth digits, and FCR into EPL and extensor indicis. The use of both FCR and FCU decreased the flexion power of the wrist as well as excessive dorsiflexion of wrist on extension of the fingers. It relies on the long flexors of the fingers that can act as flexors of the wrist. These disadvantages forced the researchers to finally give up Jones transfer. Zachary modified Jones transfer and underlined the importance of preserving an active wrist flexor to stabilise the wrist. Failure to practice these basics often leads to incomplete extension of the fingers and unnecessarily weakens or abolishes the power of wrist flexion. Preserving FCR may actually prevent these sequelae [11].
The customary tendon transfers for management of radial nerve palsy are FCR transfer (Brand), the FCU transfer (Zachary) and the superficialis transfer (Boyes). All three transfers use the PT to ECRB transfer to restore wrist extension, but vary in the transfers used to restore finger and thumb extension. Boyes also practiced transfer of FCR to APL and EPB to render independent thumb movements [12]. Merle d’Aubigne used FCU to power the EPL and EDC together and Palmaris Longus (PL) is transferred to the EPB and APL to provide thumb abduction [13]. Sammer DM and Chung KC, were of the opinion that all the transfers had good and reliable results and it was futile to compare one procedure with the other [14].
The PT tendon should be divided at its distal insertion with generous strip of periosteum from the radius to lengthen the PT [15] as well as strengthen the transfer to ECRB. This would also prevent the transfer from getting lax and subsequent loss of the vital wrist extension. Dawson CK and Mudgal CS, reported donor tendon lengthening by local harvested strips of dorsal forearm fascia [16]. PT can be sewn to ECRB end to end or end to side which depended on expected reinnervation of the radial nerve. Repair of the radial nerve increases the chances of ECRB reinnervation and this can be facilitated by end-to-side transfer. The emphasis on end to end transfer can be viewed in light of the fact that excellent results were obtained even with end to side PT-ECRB transfer as found in the present study. Chuinard RG et al., also got exuberant results with end to side transfer [17]. They evaluated with their own evaluation scheme and achieved wrist extension of >50° in 50% patients.
Boyes’ superficialis transfer to ECRB as well as ECRL caused too much radial deviation and should be avoided [14]. ECRB enjoys supremacy over ECRL as a recipient muscle for wrist extension owing to ECRL tendon insertion about 1.5 cm lateral to the ECRB resulting in moderate lateral deviation of the extended wrist [18]. The moment of arms for extension of the wrist are 16.30 mm for the ECRB and only 12.50 mm for the ECRL [19]. Thus, ECRB is the most effective extensor of the wrist. ECRL becomes a wrist extensor only after radial deviation is balanced against the ulnar forces of the ECU which is itself paralysed.
Controversy shrouds over using FCU or FCR for transfer to motorise EDC for MCP extension. FCU supposed to be a strong wrist flexor, has been a tagged as a poor choice in many studies. However, author did not encounter any trouble or grave complication while using FCU transfer in this study. Deficit of only 18°±6.78° (range 10°-40°) was observed in complete MCP joints extension [Table/Fig-3]. On the contrary, Zachary RB, studied 22 patients using both FCR and FCU and reported 30° and 60° respectively of the defective range of extension of the fingers [11]. Al Qattan MM also demonstrated extension deficits of the MP joints of the fingers within 7° [20]. The four EDC tendons should be divided just distal to their musculo-tendinous junction which is well proximal to the extensor retinaculum. This helps in smooth gliding and prevent bow-stringing that occurs on dividing the extensor retinaculum [14]. The usual route of FCU transfer is subcutaneous along the medial border of ulna. FDS to long finger is also an excellent choice to motorise the EDC and has been implicated as more effective when taken through the interosseous membrane [12]. The interosseous route is more superfluous than necessity and therefore author still vote in favour of the subcutaneous route for transfer of FCU.
Starr CL in 1922 introduced the PL muscle for thumb extension [21]. In the present study too, PL used to power the EPL, was dissected by two small vertical incisions and divided as distally as possible at the wrist. At the same time, EPL divided near its musculo-tendinous junction is taken out of the third extensor compartment and transposed radial to Lister’s tubercle. This allows a straighter line of pull for thumb extension as well as radial abduction of the thumb to the extent of 37.6°±7.51° (14°-45°). Al Qattan MM described excellent results with thumb abduction of 55° (range 50-60°) [20]. Ochi K et al., described a modification of the standard procedure in which PL was lengthened with an extension of the palmar aponeurosis raised in continuity with PL. They also had woven PL into the undivided EPL tendon to preserve it for possible future recovery [22].
After tendon transfer, Smith RJ advised to set the tension of the donor muscle on the high side at approximately 75% of maximal excursion [23]. It was also advised that appropriate tension should extend all 4 fingers synchronously and adequately when the wrist is flexed.
Several schemes have been published to evaluate the results of tendon transfers in radial nerve palsy [24]. Zachary, “too rigid and simplistic”, only evaluates the ability to flex to a neutral position [25]. Being more subjective, the Zachary method paid little attention to functional results from the perspective of the patients [26]. Chuinard RG, reported results in 22 patients undergoing FDS tendon transfer over a 20-year period and offered his own evaluation scheme [17]. Tajima evaluation score is extremely arbitrary, vague and prone to be biased by the examining surgeon. Various other evaluation schemes include Disabilities of the Arm, Shoulder and Hand (DASH) score and Neumann Pertecke evaluation scheme (modified Zachary scheme) with their own set of advantages and disadvantages. Bincaz scoring was selected to evaluate the patients as it is more simple, logical and quantitative compared to other scoring systems [Table/Fig-7] [9].
Tendon transfers are useful in restoring hand functions but compromises the strength of donor tendons. Despite the less popular and controversial FCU based tendon transfers for radial nerve palsy [27], authors have obtained good results with the Zachary’s tendon transfer coupled with aggressive physiotherapy of hand joints. Painful neuromas [7] can be managed by anaesthetic injection, proximal transection or cauterising and burying the end within muscle or other soft tissue [28].
Limitation(s)
The present work, being retrospective, lacks control population. The study does not compare different methods of tendon transfers for radial nerve palsy. FCR as a donor tendon and its utility as MCPJ extensor has neither been carried out or discussed.
The future work would benefit from multicentric study and comparative evaluation of different surgical techniques like FCR vis-a-vis FCU for MCP joint extension. The possible role of brachioradialis instead of PT as a donor tendon to motorise ECRB for wrist extension may be explored to open newer dimensions.
Conclusion(s)
Flexor Carpi Ulnaris (FCU) based Zachary’s modification of Jones tendon transfer yields gratifying functional results in patients with isolated high radial nerve palsy. All patients regained thumb extension up to 45°, the ability to extend, flex the wrist, good extension of the digits as well as good patient satisfaction through Bincaz score. Intervention was recommended if there was no recovery at three months while postoperative outcome depended on strict rehabilitation protocol. Adherence to basic principles of tendon transfer techniques was vital to minimise undesirable complications.
FC: Flexor carpi ulnaris; PT: Pronator teres; PL: Palmaris longus; FDS III: Flexor digitorum superficialis III
Excellent ≥8, Good 6-7, Fair 4-5, Bad ≤3
Interpretation of the Bincaz score: If the patient is able to perform wrist extension >29°, full extension of metacarpophalangeal joint and first web space opening between 30 to 39°. He is fully satisfied with the outcome of the surgery and has already returned to work. These made the score is 8 points, showing the functional outcome is Excellent