Vernal Keratoconjunctivitis- A Survey on Practice Patterns and Perspectives of Indian Ophthalmologists
Shwetha N Chandranna1, Ratthiga Balagopal2, Santosh Achappa3, Kaushal Kumar4
1 Assistant Professor, Department of Ophthalmology, Dr Chandramma Dayananda Sagar Institute of Medical Education and Research, Ramanagara, Karnataka, India.
2 Junior Resident, Department of Ophthalmology, Rajarajeswari Medical College and Hospital, Bengaluru, Karnataka, India.
3 Associate Professor, Department of Community Medicine, Dr Chandramma Dayananda Sagar Institute of Medical Education and Research, Ramanagara, Karnataka, India.
4 Professor and Head, Department of Ophthalmology, Rajarajeswari Medical College and Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Shwetha N Chandranna, H. No. 7043, Ebony Block, Sobha Forest View, Off Kanakpura Road, Vajrahalli, Bengaluru, Karnataka, India.
E-mail: dr.shwethanc@gmail.com
Introduction
Vernal Keratoconjunctivitis (VKC) is a common chronic allergic condition mostly affecting children and their childhood. At present, the choice of medication varies greatly for the same severity of disease from one ophthalmologist to another. A standardised grading system and a comprehensive approach towards VKC including Quality of Life (QOL) assessment is the need of the hour.
Aim
To learn the practice patterns and perspectives of Indian Ophthalmologists in the management of VKC and to propose strategies for the holistic approach.
Materials and Methods
A cross-sectional survey was conducted in July 2020. A semi-structured questionnaire was sent via Google form to 200 ophthalmologists. Data was entered in excel and analysis was performed using the Statistical Package of Social Sciences (SPSS) software version 20.
Results
Out of 200 ophthalmologists, 146 (73%) participated in the survey. Among the participants, 43.8% used combination therapy in the management of VKC and 68.5% resorted to steroid therapy in severe cases. Tacrolimus (0.03%) was the most preferred immunomodulator among 56% ophthalmologists and only 11% assessed QOL in the patients periodically.
Conclusion
Majority (around 2/3rd) felt immunotherapy and vitamin D supplementation can be tried in the management of VKC and there was a consensus on administering a QOL questionnaire in all patients with VKC in future which would provide holistic care.
Immunotherapy, Immunomodulators, Quality of life, Vitamin D
Introduction
The Vernal Keratoconjunctivitis (VKC) is a chronic, allergic inflammation of the conjunctiva and cornea, more often seasonally exacerbated. It is a recurrent bilateral condition affecting predominantly boys in their first decade of life having an atopic background and usually resolves at the onset of puberty. The initial seasonal attacks in the spring turn into perennial disease after a few years requiring long term treatment. The prevalence of VKC is greater in the regions with hot and humid climate including the Indian sub-continent [1-6]. VKC was traditionally considered a type I hypersensitivity reaction. A horde of cells and mediators have been identified on the ocular surface which may have a role in the pathogenesis of the disease [7-12]. Diagnosis is based on typical clinical signs and symptoms, including intense itching, photophobia, characteristic stringy mucus discharge and giant papillae on the upper tarsal conjunctiva or at the limbus.
The hallmark of palpebral form of VKC is papillary hyperplasia in the upper tarsal conjunctiva [13]. The characteristic clinical sign in limbal VKC is infiltration of the limbal nodules and Horner-Trantas dots. Corneal involvement may be seen as punctate epithelial keratopathy leading to macro erosion and shield ulcers [14,15]. Recurrence of the disease is the most challenging task to deal with while treating a case of VKC [16]. Medical treatment options range from lubricants, antihistamines and mast cell stabilisers to topical steroids and steroid sparing agents like cyclosporine, tacrolimus and mitomycin C. At present, the choice of medication varies greatly for the same severity of disease from one ophthalmologist to another [17]. Though a few grading systems are available to classify the severity of VKC, there is no well-defined standardised guidelines to suggest appropriate therapy for different grades of VKC. Children with VKC also experience a negative impact on their QOL and functioning due to limitation of their preferred outdoor activities to avoid triggers and allergens [18]. This study aims to learn the perspectives, protocols and preferred practice patterns of Indian ophthalmologists in the management of VKC and propose strategies for holistic approach.
Materials and Methods
The cross-sectional study was initiated in July 2020 and was carried out for five months. An Institutional Ethical Committee clearance was obtained prior to the study (RRMCH-IEC/17/2021). An online survey via Google forms to learn about practice patterns of Indian ophthalmologists regarding VKC was conducted. The study was conducted in strict adherence to the tenets of the Declaration of Helsinki. The survey invitation was sent out to 200 ophthalmologists who were registered members of state or all India ophthalmological society, across the country. The questionnaire was semi-structured and designed to understand ophthalmologists experience with VKC in their setting and included questions which aimed at assessing the knowledge and their practice patterns. Purpose of the study was stated in the questionnaire and participants who gave electronic consent were able to take part in the survey. The responses were collected and analysed.
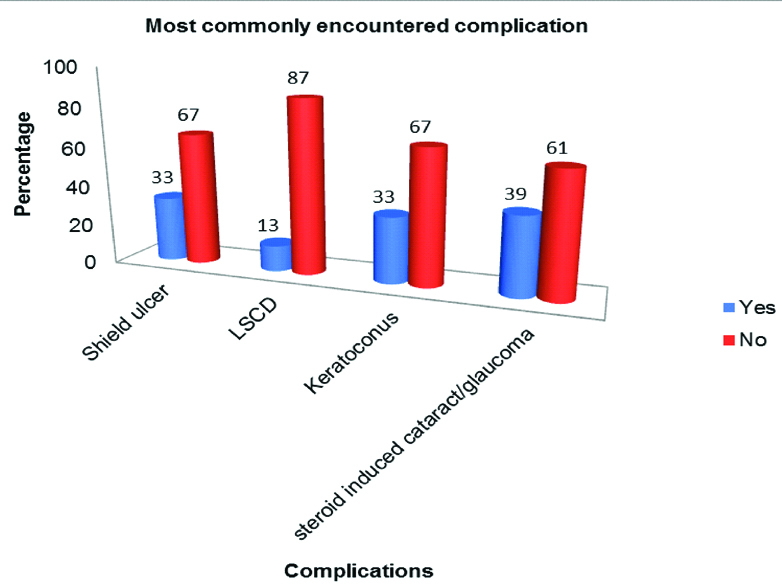
Sample size calculation: Nonprobability sampling technique (Convenience sampling)
Statistical Analysis
Data was entered in excel and analysis was performed using the SPSS software version 20. A p-value of <0.05 was considered statistically significant.
Results
Of the 200 survey invitations sent out, 146 ophthalmologists responded and completed the survey, bringing the response rate to 73%. According to the survey, 56 (38%) ophthalmologists treat around 10-25 cases in a month, 50 (34%) ophthalmologists treat 5-10 cases, 22 (15%) treat more than 25 per month and 12.3% of the doctors see less than five VKC cases in their OPD volume. Majority (70%) of the ophthalmologists opined that VKC predominantly affects boys and 40 (27%) of them did not see gender predilection. One hundred and two participants (70%) felt VKC resolves by puberty. The idea of IgE being the sole factor as the pathogenic mechanism is lost as 106 ophthalmologists (73%) answered “no” when they were asked “If IgE is wholly responsible for VKC?” Nearly half of the respondents which are 70 of them, (47.9%) found mixed form of VKC to be more prevalent and 52 respondents (35.6%) had opined palpebral form to be common and the rest thought bulbar form is more common. Majority (82%) of the respondents in the present study classified VKC based on clinical signs and symptoms without adopting any standard grading system, (8%) of the participants classified VKC based on subjective ocular symptoms. Rest of the participants followed the Gokhale grading system (7%) and 5-5-5 exacerbation grading scale (3%).
A greater part (89%) of the ophthalmologists reported the most effective management tool to be careful in history and examination, ten (7%) of the respondents used VKC-CLEK scoring, four (3%) used impression cytology to aid in management and 1% of them used IgE levels as the management tool. From the armamentarium of medications to treat VKC, 64 doctors (43.8%) used combination therapy as the first line of drug in a newly diagnosed case of VKC, 48 (33%) used dual and multi action drugs and the rest used mast cell stabilisers (11%) or topical antihistamines (12%). Tacrolimus 0.03% was the most popular immunomodulator preferred by 82 respondents (56%), followed by Cyclosporin A 0.5% preferred by 32 ophthalmologists (22%). Regarding the duration of usage 64 respondents (44%) reported usage of immunomodulators for three months, 52 ophthalmologists (36%) for six months and 14 (10%) of them continued immunomodulator therapy for one year. Despite on immunomodulator therapy, many patients have flare-ups and 102 respondents (70%) reported to have used rescue steroids once or twice in a year as an add on to immunomodulator therapy, 16 respondents (11%) did not see flare-ups in their patients during immunomodulator therapy avoiding rescue steroids altogether. Amongst the newer drugs, bepotastine is the most popular drug, preferred by 64 respondents (43.8%) followed by alcaftadine as voted by 42 participants (29%).
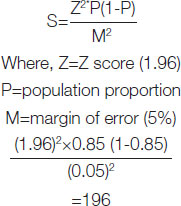
Next three questions had multiple options to select and multiple response analysis was performed. The drug preferred in recurrent cases is topical corticosteroids as reported by 72% of the ophthalmologists in the survey as shown in [Table/Fig-1]. The most commonly used steroid is loteprednol 0.5%, as voted by 51% of the participants and fluorometholone, chosen by the 40% of them, shown in [Table/Fig-2]. Steroid induced cataract/glaucoma is the most commonly encountered complication as per 39% of the respondents shown in [Table/Fig-3], followed by keratoconus (33%), shield ulcer (33%) and Limbal Stem Cell Deficiency (LSCD) (13%). Larger part of the respondents which is 90 of them (62%) expressed interest in trying out other modality of treatment like immunotherapy and 46 respondents (32%) believed immunotherapy can be a useful adjunct to topical therapy. Nearly, all respondents (n=142, 97%) felt it is important to assess QOL in children with VKC and 118 ophthalmologists (81%) expressed their interest in administering a QOL assessment questionnaire to all patients in future. More than 90% of the participants educate children with VKC and their parents about the triggers and the complications of VKC. When asked if the participants preferred to add Vitamin D supplementation in children with VKC, 67% of the participants indicated their interest in the therapy and 18% of them were already supplementing Vitamin D in deficient patients.
Showing the distribution of respondents based on drugs that are preferred in recurrent/severe Vernal Keratoconjunctivitis.
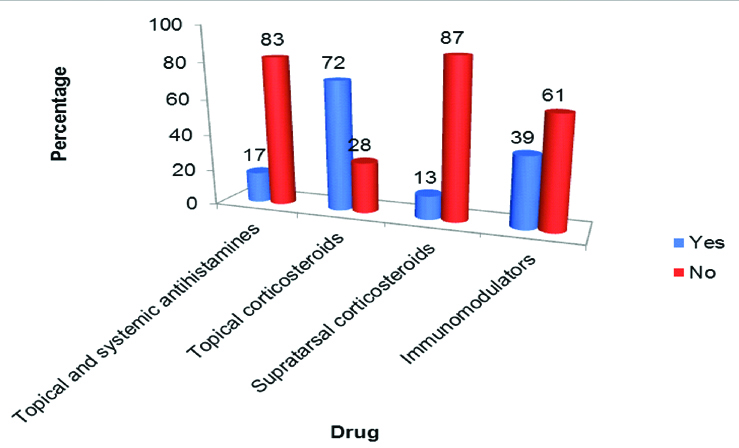
Showing the distribution of the respondents based on the most commonly used steroid in Vernal Keratoconjunctivitis.
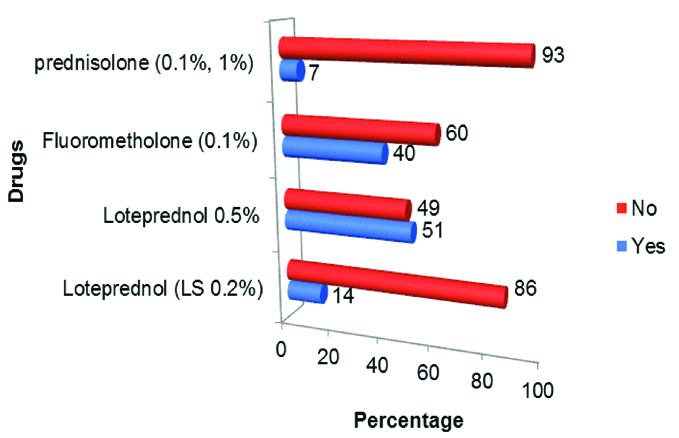
Showing the distribution of the respondents based on most commonly encountered complication in Vernal Keratoconjunctivitis.
Discussion
This survey provides the much needed insight into the management practice patterns in VKC among Indian ophthalmologists. A comprehensive data on the epidemiology of VKC is not available from India due to lack of unanimity over its diagnostic criteria. The condition predominantly affects young boys with male to female ratio varying from 6.4:1 as seen in a study from India by Saboo US et al., [19] to 4:1 reported by Neumann E et al., in 1959 [20] to 2:1 before 20 years of age, after which there is no gender predilection as stated by Bonini S et al., [16]. In the present study, 70% of the ophthalmologists stated that VKC has male preponderance and resolves at the onset of puberty. Sacchetti M et al., demonstrated that boys with active VKC have different circulating sex hormone levels as compared to healthy subjects, and hence strengthening the hypothesis of possible protective function of androgens at the onset of puberty [21]. Larger part of our respondents, about 73% believed that IgE is not a solitary causative factor of VKC and rather a complex interplay between the nervous, endocrine and immune system as reported by Bonini S et al., [3]. Close to half of the participants (47.9%) opined mixed form of VKC to be more common in our population. A study by Saboo US et al., also reported mixed variant of VKC to be more prevalent in tropical Indian sub-continent [19]. Bulbar/limbal VKC is more common in the Asian and African population and the palpebral form in Europe and the United States [22].
Typical clinical presentation of VKC makes the diagnosis fairly straightforward. Most of the participants (82%) in the present study classified VKC based on clinical signs and symptoms like Saboo US et al., [19]. Gokhale NS proposed a simple and easy grading system for VKC considering two important things- severity of clinical signs and frequency of symptoms, both of which are crucial in the management of this condition [17], which was used by ten (7%) of our ophthalmologists. Other grading systems are Bonini grading and 5-5-5 exacerbation grading scale. A large number of respondents (89%) chose “careful history and examination” as the most effective management tool for this condition. Immunological tests are not indicated routinely and are performed as a part of research for developing new diagnostic tools and therapies; explain Singhal D et al., [12].
In this survey, the popular choice for first line of drug in a case of newly diagnosed VKC is combination therapy as voted by 44% of the respondents, followed by dual and multi action drugs preferred by 33% of the doctors and the remainder used mast cell stabilisers (11%) or topical antihistamines (12%). Mantelli F et al., made an assessment of efficacy of topical drugs for VKC through a meta-analysis of Randomised Clinical Trials (RCTs). Their study had a systematic review of 27 RCTs on topical drugs for the treatment of VKC. The topical drugs evaluated were mast cell stabilisers, immunomodulators, nonsteroidal anti-inflammatory drugs, and antimitotic agents. This systematic review revealed that all the drugs are safe, well tolerated, and effective in controlling signs and symptoms of patients with acute VKC [23]. Top ranking immune-modulator amongst our respondents was tacrolimus 0.03% (56%) preferred by more than half of them, followed by cyclosporine A 0.5% (22%). Chatterjee S and Agrawal D studied the efficacy of 0.03% tacrolimus ointment in steroid-refractory patients with VKC and found that only four patients out of 23 required adjunct corticosteroid therapy after four weeks of tacrolimus therapy [24]. Keklikci U et al., in their placebo-controlled, randomised prospective study, successfully treated 62 patients of VKC with Cyclosporine A (CsA) 0.05% Quater In Die (QID) [25]. Yücel OE and Ulus ND evaluated the safety and efficacy of topical Cyclosporine A 0.05% QID in refractory VKC patients [26]. The use of CsA 0.05% resulted in reduced steroid demand and demonstrated good safety profile. Higher concentrations of CsA 1%, 2% have also been studied in the treatment of VKC and proven to be safe but should be extemporaneously compounded.
Gokhale NS et al., successfully treated a patient with severe, vision threatening VKC with oral cyclosporine therapy [27]. The use of CsA 0.1% in VKC has been approved in Japan, and is off-licensed in most of the countries [28]. Tacrolimus 0.03% has been a popular choice of immune-modulator recently. There is paucity of data to prove its safety as an ophthalmic suspension for long-term use in VKC. The risk of malignancy associated with long-term use of tacrolimus topical formulation as highlighted by the public health advisory in the US should not be ignored [29]. The drug of choice for recurrent or severe cases of VKC is topical corticosteroids among our respondents and for various authors across the world. Low potency steroids like loteprednol 0.5% and fluorometholone acetate 0.1% are the first line of steroids as they are associated with lesser side-effects. Respondents in this study also picked loteprednol 0.5% and fluorometholone 0.1% as their go-to-steroid. High potency steroids like prednisone acetate 1% and dexamethasone should be used when low potent steroids are ineffective. Long term administration entails sight threatening complications such as cataract and glaucoma, thereby not recommended [12]. Newer drugs with dual action such as bepotastine and alcaftadine have been used in recent times and are faring well. Our respondents too found Bepotastine and alcaftadine to be beneficial in their practice.
VKC is associated with complications due to chronicity of the condition and adverse effects of the drugs used in its management. Common complications encountered by the Ophthalmologists in the survey are steroid induced glaucoma/cataract (39%), keratoconus and shield ulcers (33%). Totan et al studied the incidence of keratoconus in VKC by videography and found 27% of the patients to have keratoconus [30]. Bonini S et al., reported 2% incidence of steroid induced glaucoma and no incidence of cataract in their largest case series. They found corneal involvement in 50% of the patients with palpebral form which results in complications such as shield ulcer and neovascularisation of the cornea [16]. A study by Saboo US et al., reported peripheral corneal neovascularisation in 7.26% and LSCD was in 1.2% of the patients [19]. A close follow-up is mandated to allow early detection of the complications and management.
The survey participants indicated an interest in adjunction or substituting topical therapy with allergen immunotherapy. A study by Mahdy RA et al., demonstrated treatment by subcutaneous immunotherapy to be more effective in improving the clinical symptoms and reducing the serum IgE than topical treatment [31]. The assessment of QOL helps us to understand the impact of the disease on the activities of daily living of individuals and also to determine the effect of various therapies, thereby helping ophthalmologists to make correct clinical decisions. There was a consensus (97%) among our respondents to administer a QOL questionnaire in all VKC patients. Children with VKC also suffer from Vitamin D deficiency, likely due to avoidance of outdoors activities and hence deprived of sun exposure. Significant correlations have been found between vitamin D level and the severity of the disease in a study by Zicari AM et al., [32]. Vitamin D supplementation should be part of VKC treatment. Education of patients and/or their parents regarding the recurrent nature of the disease, the triggers and the complications from long term therapy or the disease per se cannot be overemphasised.
Limitation(s)
Though the response rate for this study was 73%, to obtain generalisable results future similar studies with more open ended questions in the survey need to be planned for a larger group of subjects.
Conclusion(s)
This survey provides the bird’s eye view of VKC in India, practices of Indian ophthalmologists and their perspectives. VKC in its severe form can be sight-threatening and life-altering. The Holistic approach is the best way forward to combat this serious entity. Standardised grading systems help to decide appropriate therapy and identify patients with higher risk for recurrences. The end point of appropriate treatment should be alleviation of symptoms and improvement in QOL of the child. QOL assessment should be done periodically by incorporating a QOL assessment questionnaire in all patients. It is critical that patients adhere to their long-term treatment regimen which can be achieved by counseling and educating them. Vitamin D supplementation should be integrated in the treatment plan in vitamin D deficient VKC patients. Collaboration between the ophthalmologist, immunologist, paediatrician and constant care and support from parents help children with VKC live life to full. Comprehensive care is what a child with VKC needs. Can we deliver that?
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 28, 2021
Manual Googling: Mar 05, 2021
iThenticate Software: Mar 30, 2021 (18%)
[1]. Kumar S, Vernal keratoconjunctivitis: A major review 2020 [Google Scholar]
[2]. Leonardi A, Secchi AG, Vernal keratoconjunctivitisInt Ophthalmol Clin 2003 43(1):41-58.10.1097/00004397-200343010-0000712544394 [Google Scholar] [CrossRef] [PubMed]
[3]. Bonini S, Coassin M, Aronni S, Lambiase A, Vernal keratoconjunctivitisEye (Lond) 2004 18(4):345-51.10.1038/sj.eye.670067515069427 [Google Scholar] [CrossRef] [PubMed]
[4]. Leonardi A, Busca F, Motterle L, Cavarzeran F, Fregona IA, Plebani M, Case series of 406 vernal keratoconjunctivitis patients: A demographic and epidemiological studyActa Ophthalmol Scand 2006 84(3):406-10.10.1111/j.1600-0420.2005.00622.x16704708 [Google Scholar] [CrossRef] [PubMed]
[5]. Lambiase A, Minchiotti S, Leonardi A, Secchi AG, Rolando M, Calabria G, Prospective, multicenter demographic and epidemiological study on vernal keratoconjunctivitis: A glimpse of ocular surface in Italian populationOphthalmic Epidemiol 2009 16(1):38-41.10.1080/0928658080257317719191180 [Google Scholar] [CrossRef] [PubMed]
[6]. Tabbara KF, Ocular complications of vernal keratoconjunctivitisCan J Ophthalmol 1999 34(2):88-92.10321319 [Google Scholar] [PubMed]
[7]. Bonini S, Bonini S, IgE and non-IgE mechanisms in ocular allergyAnn Allergy 1993 71(3):296-99. [Google Scholar]
[8]. Irani AM, Butrus SI, Tabbara KF, Schwartz LB, Human conjunctival mast cells: Distribution of MCT and MCTC in vernal conjunctivitis and giant papillary conjunctivitisJ Allergy Clin Immunol 1990 86(1):34-40.10.1016/S0091-6749(05)80120-4 [Google Scholar] [CrossRef]
[9]. Abelson MB, Madiwale N, Weston JH, Conjunctival eosinophils in allergic ocular diseaseArch Ophthalmol 1983 101(4):555-56.10.1001/archopht.1983.010400105550026838412 [Google Scholar] [CrossRef] [PubMed]
[10]. Fujishima H, Takeuchi T, Shinozaki N, Saito I, Tsubota K, Measurement of IL-4 in tears of patients with seasonal allergic conjunctivitis and vernal keratoconjunctivitisClin Exp Immunol 1995 102(2):395-98.10.1111/j.1365-2249.1995.tb03796.x7586697 [Google Scholar] [CrossRef] [PubMed]
[11]. Abu El-Asrar AM, Geboes K, Al-Kharashi S, Tabbara KF, Missotten L, Desmet V, Adhesion molecules in vernal keratoconjunctivitisBr J Ophthalmol 1997 81:1099-06.10.1136/bjo.81.12.10999497473 [Google Scholar] [CrossRef] [PubMed]
[12]. Singhal D, Sahay P, Maharana PK, Raj N, Sharma N, Titiyal JS, Vernal KeratoconjunctivitisSurv Ophthalmol 2019 64(3):289-311.10.1016/j.survophthal.2018.12.00130550738 [Google Scholar] [CrossRef] [PubMed]
[13]. Beigelman MN, Vernal Conjunctivitis 1950 Los AngelesUniversity of Southern California Press [Google Scholar]
[14]. Tuft SJ, Dart JK, Kemeny M, Limbal vernal keratoconjunctivitis: Clinical characteristics and immunoglobulin E expression compared with palpebral vernalEye (Lond) 1989 3(4):420-27.10.1038/eye.1989.632606216 [Google Scholar] [CrossRef] [PubMed]
[15]. Cameron JA, Shield ulcers and plaques of the cornea in vernal keratoconjunctivitisOphthalmology 1995 102(6):985-93.10.1016/S0161-6420(95)30925-6 [Google Scholar] [CrossRef]
[16]. Bonini S, Bonini S, Lambiase A, Marchi S, Pasqualetti P, Zuccaro O, Vernal keratoconjunctivitis revisited: A case series of 195 patients with long-term follow upOphthalmology 2000 107(6):1157-63.10.1016/S0161-6420(00)00092-0 [Google Scholar] [CrossRef]
[17]. Gokhale NS, Systematic approach to managing vernal keratoconjunctivitis in clinical practice: Severity grading system and a treatment algorithmIndian J Ophthalmol 2016 64:145-48.10.4103/0301-4738.17972727050351 [Google Scholar] [CrossRef] [PubMed]
[18]. Sacchetti M, Baiardini I, Lambiase A, Aronni S, Fassio O, Gramiccioni C, Development and testing of the quality of life in children with vernal keratoconjunctivitis questionnaireAm J Ophthalmol 2007 144(4):557-63.10.1016/j.ajo.2007.06.02817693381 [Google Scholar] [CrossRef] [PubMed]
[19]. Saboo US, Jain M, Reddy JC, Sangwan VS, Demographic and clinical profile of vernal keratoconjunctivitis at a tertiary eye care center in IndiaIndian J Ophthalmol 2013 61(9):486-89.10.4103/0301-4738.11943124104706 [Google Scholar] [CrossRef] [PubMed]
[20]. Neumann E, Gutmann MJ, Blumenkrantz N, Michaelson IC, A review of four hundred cases of vernal conjunctivitisAm J Ophthalmol 1959 47(2):166-72.10.1016/S0002-9394(14)76417-7 [Google Scholar] [CrossRef]
[21]. Sacchetti M, Lambiase A, Moretti C, Mantelli F, Bonini S, Sex hormones in allergic conjunctivitis: Altered levels of circulating androgens and estrogens in children and adolescents with vernal keratoconjunctivitisJ Immunol Res 2015 2015:94531710.1155/2015/94531725756057 [Google Scholar] [CrossRef] [PubMed]
[22]. Bremond-Gignac D, Donadieu J, Leonardi A, Pouliquen P, Doan S, Chiambarretta F, Prevalence of vernal keratoconjunctivitis: A rare disease?Br J Ophthalmol 2008 92(8):1097-102.10.1136/bjo.2007.11781218356259 [Google Scholar] [CrossRef] [PubMed]
[23]. Mantelli F, Santos MS, Petitti T, Sgrulletta R, Cortes M, Lambiase A, Systematic review and meta-analysis of randomised clinical trials on topical treatments for vernal keratoconjunctivitisBr J Ophthalmol 2007 91(12):1656-61.10.1136/bjo.2007.12204417588996 [Google Scholar] [CrossRef] [PubMed]
[24]. Chatterjee S, Agrawal D, Tacrolimus in corticosteroid-refractory vernal keratoconjunctivitisCornea 2016 35(11):1444-48.10.1097/ICO.000000000000091827310883 [Google Scholar] [CrossRef] [PubMed]
[25]. Keklikci U, Dursun B, Cingu AK, Topical cyclosporine a 0.05% eyedrops in the treatment of vernal keratoconjunctivitis- Randomised placebo-controlled trialAdv Clin Exp Med 2014 23(3):455-61.10.17219/acem/3714524979519 [Google Scholar] [CrossRef] [PubMed]
[26]. Yücel OE, Ulus ND, Efficacy and safety of topical cyclosporine A 0.05% in vernal keratoconjunctivitisSingapore Med J 2016 57(9):507-10.10.11622/smedj.201516126768065 [Google Scholar] [CrossRef] [PubMed]
[27]. Gokhale NS, Samant R, Sharma V, Oral cyclosporine therapy for refractory severe vernal keratoconjunctivitisIndian J Ophthalmol 2012 60:220-23.10.4103/0301-4738.9587822569387 [Google Scholar] [CrossRef] [PubMed]
[28]. Takamura E, Uchio E, Ebihara N, Okamoto S, Kumagai N, Shoji J, A prospective, observational, all-prescribed-patients study of cyclosporine 0.1% ophthalmic solution in the treatment of vernal keratoconjunctivitisNippon Ganka Gakkai Zasshi 2011 115(6):508-15. [Google Scholar]
[29]. Siegfried EC, Jaworski JC, Hebert AA, Topical calcineurin inhibitors and lymphoma risk: Evidence update with implications for daily practiceAm J Clin Dermatol 2013 14(3):163-78.10.1007/s40257-013-0020-123703374 [Google Scholar] [CrossRef] [PubMed]
[30]. Totan Y, Hepşen IF, Cekiç O, Gündüz A, Aydin E, Incidence of keratoconus in subjects with vernal keratoconjunctivitis: A videokeratographic studyOphthalmology 2001 108(4):824-27.10.1016/S0161-6420(00)00664-3 [Google Scholar] [CrossRef]
[31]. Mahdy RA, Nada WM, Marei AA, Subcutaneous allergen-specific immunotherapy versus topical treatment in vernal keratoconjunctivitisCornea 2012 31(5):525-28.10.1097/ICO.0b013e3181eae27022314814 [Google Scholar] [CrossRef] [PubMed]
[32]. Zicari AM, Cafarotti A, Occasi F, Lollobrigida V, Nebbioso M, Pecorella I, Vitamin D levels in children affected by vernal keratoconjunctivitisCurr Med Res Opin 2017 33(2):269-74.10.1080/03007995.2016.125460227786545 [Google Scholar] [CrossRef] [PubMed]