Use of Dexmedetomidine as an Adjuvant to Propofol along with Neurophysiological Monitoring of the Seventh Cranial Nerve during Cerebello- Pontine Tumour Excision Surgery
Pooja Arpan Shah1, Gayatri Vasagadekar2, Akhilesh Chhaya3
1 Assistant Professor, Department of Anaesthesiology, S.B.K.S.MI and RC, Sumandeep Vidyapeeth, Piparia, Vadodara, Gujarat, India.
2 Resident, Department of Anaesthesiology, S.B.K.S.MI and RC, Sumandeep Vidyapeeth, Piparia, Vadodara, Gujarat, India.
3 Professor, Department of Anaesthesiology, Gujarat Adani Institute of Medical Sciences, Bhuj, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Pooja Arpan Shah, A/105, Shreenathdeep Society, Near Poonam Complex, Waghodia Road, Vadodara, Gujarat, India.
E-mail: poojapatwa249@gmail.com
Cerebello-Pontine Angle (CPA) surgeries are very challenging for neurosurgeons as it lies very close to brain stem so various cranial nerves are at risk of damage. Generally, such surgeries require neuromuscular monitoring of various cranial nerves. For that we have to discontinue neuromuscular blocking agents and inhalational agents. Total Intravenous Anaesthesia (TIVA) avoids the use of neuromuscular blocking agents as well as inhalational agents. However, prolonged infusion of propofol is associated with risks, such as hypotension, delayed awakening, and metabolic acidosis, known as “Propofol Infusion Syndrome”. Dexmedetomidine now-a-days is used very commonly as an adjuvant to propofol and it significantly reduces the anaesthetic requirement. Addition of dexmedetomidine provides haemodynamic stability during such neurosurgeries. Here, authors have described anaesthetic management of a 46-year-old female patient posted for CPA excision along with seventh cranial nerve monitoring using dexmedetomidine with propofol.
Alpha-adrenergic agonist, Neurological monitoring, Posterior cranial fossa surgery
Case Report
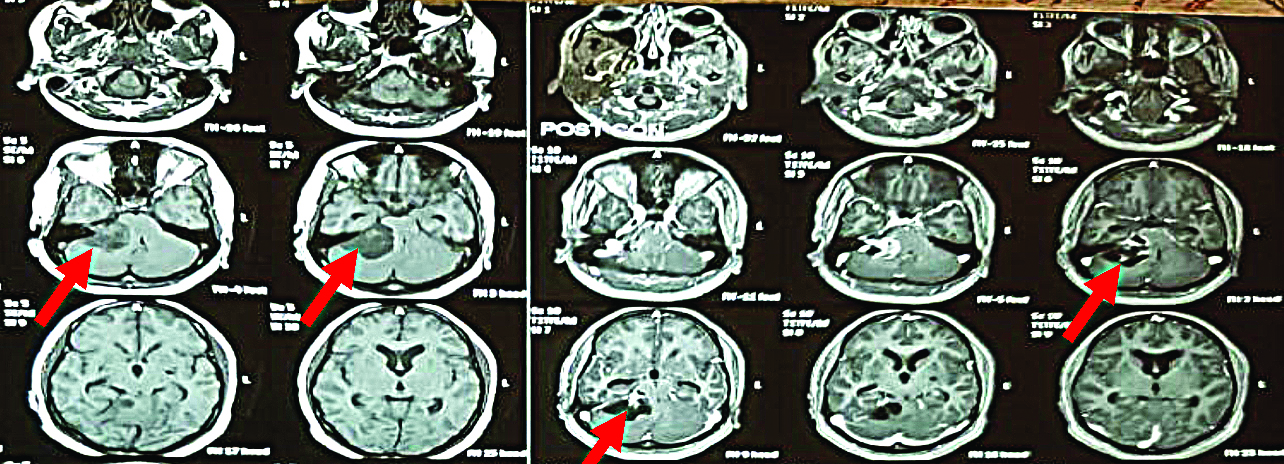
A 46-year-old female patient weighing 60 kilograms presented with dizziness and loss of hearing since 6 to 8 months and was diagnosed to have right CPA tumour (38×31×30 mm) [Table/Fig-1]. She was posted for right suboccipital craniotomy with tumour excision. There was no significant past, personal or family history. Cardiovascular and respiratory system examination was also normal. Central nervous system examination and cranial nerves examination were also normal. All the routine laboratory investigations and Electrocardiogram (ECG) were normal.
Magnetic Resonance Imaging (MRI) of the patient showing right Cerebello-Pontine Angle (CPA) tumour (38×31×30 mm) (Red arrows).
Procedure was explained and written informed consent was obtained. On arrival in operating room, standard monitors were attached and an 18-guage Intravenous (IV) line was secured, 500 mL normal saline solution was started. Patient was afebrile. Her heart rate was 76 bpm, blood pressure was 120/90 mmHg and Oxygen Saturation (SpO2) was 99% on room air.
Inj. Glycopyrrolate 0.2 mg, Inj. Midazolam 1 mg, Inj. Ondansetron 4 mg, Inj. Nalbuphine 10 mg was given intravenously as premedication. Patient was preoxygenated with 100% oxygen for three minutes with anatomical face mask. Induction done with Inj. Propofol 100 mg IV + Inj. Scoline 100 mg IV + Inj. Dexmedetomidine 75 mL/hr for 20 minutes IV (2g/cc). Orotracheal intubation was done with armoured endotracheal tube No 7.5 with the aid of macintosh blade No.3 and patient was given left lateral position [Table/Fig-2].
Left lateral position of patient given intraoperatively.

Intraoperative patient was maintained on oxygen and Inj. Propofol infusion which was titrated as per requirement (50-150 ug/kg/min IV). Dexmedetomidine infusion was started at the rate of 0.3 ug/kg/min IV.
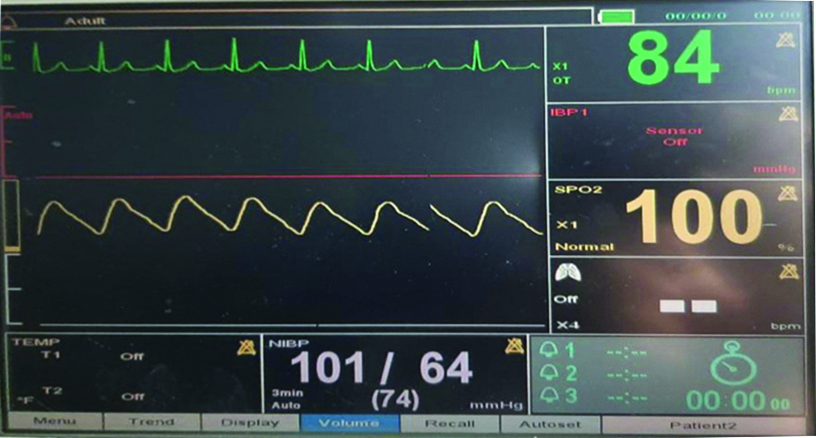
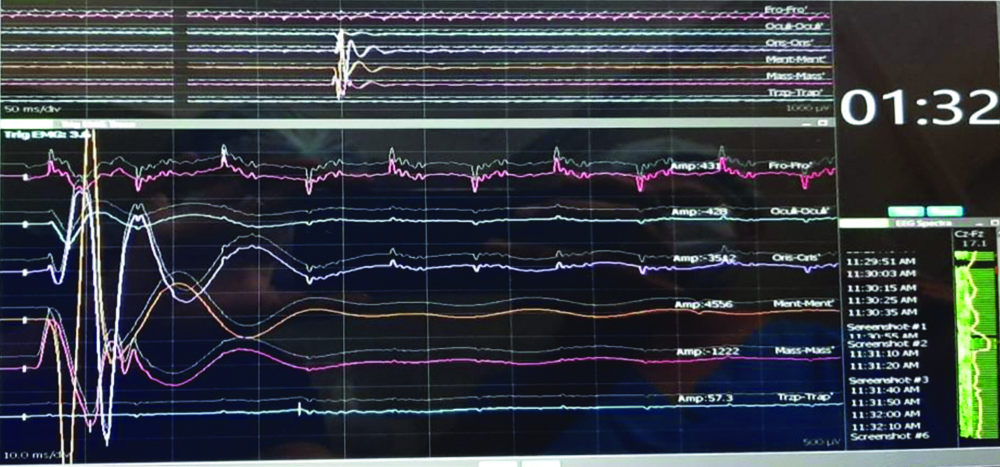
There was no non-depolarising muscle relaxant or any inhalational anaesthetic agent used for maintenance of anaesthesia. Patient was haemodynamically stable throughout the surgery [Table/Fig-3]. Electrodes were attached to various muscles of the face which were supplied by the lower cranial nerves and were monitored throughout the surgery [Table/Fig-4]. Patient was extubated without any complication and showed good postoperative recovery.
Showing intaoperative haemodynamic monitoring of the patient.
Showing monitoring of various lower cranial nerves.
Discussion
The goals of neurosurgery are to avoid increase in Intracranial Pressure (ICP), to prevent acute swelling of brain and to maintain stable cerebral haemodynamics [1]. Many neurosurgeries require intraoperative neurological monitoring. In such condition, rapid recovery from anaesthesia is required. Use of neuromuscular blocking agents does not allow monitoring of cranial nerves intraoperatively [2].
Although inhalational anaesthetics are being widely used in anaesthetic management of neurosurgery, they reduce vascular resistance which lead to increase in cerebral blood flow and raised Intracranial Pressure (ICP) [2]. Raised cerebral blood flow makes the neurosurgery more difficult and raised ICP leads to ischaemic brain damage [1]. So, simultaneous use of propofol and dexmedetomidine reduces cerebral blood flow and ICP [1]. Using propofol and dexmedetomidine can avoid the usage of inhalational agents and neuromuscular blocking agents which makes the monitoring of cranial nerves very easy intraoperatively [3].
CPA tumour excision surgeries are very critical as they require adequate depth of anaesthesia [4]. Any change in haemodynamics can lead to rise in cerebral blood flow and rise in ICP. During such surgery many neurosurgeons monitor intracranial nerve functioning which require stoppage of neuromuscular blocking agents.
Here, authors have used propofol infusion for maintenance of anaesthesia. By using propofol infusion we can maintain adequate depth of anaesthesia and can avoid using nondepolarising neuromuscular blocking agents [5]. However, there are chances of propofol infusion syndrome, we have added dexmedetomidine infusion which decreases the requirement of propofol [6].
Dexmedetomidine is an α-2 adrenergic agonist having sympatholytic, antinociceptive, sedative, anaesthetic-sparing properties [6]. Dexmedetomidine is also having analgesic effects without significant respiratory depression. As dexmedetomidine provides good perioperative haemodynamic stability during critical moments of surgical manipulation specially posterior fossa tumour handling with decreased intraoperative anaesthetic drug requirements with rapid recovery at the end of surgery [5,7]. It might be the most suitable anaesthetic adjuvant for neurosurgical operations. It acts on central α and imidazoline receptors thus it augments the anaesthetic effect of most other anaesthetic agents [7].
Chances of adverse effects like bradycardia and hypotension can be higher with the use of dexmedetomidine as an anaesthetic adjuvant during intracranial procedures. However, it can be treated with inj. Atropine 0.6 mg IV.
Maintenance of anaesthesia during posterior cranial fossa surgeries is a challenge to the anaesthesiologist as neuromuscular blocking drugs were excluded after the intubating dose was administered [6]. Additionally inhalational anaesthetics such as nitrous oxide and isoflurane were also avoided so as to reduce life threatening complications such as venous air embolism, heart failure, cardiac arrest, pneumocephalus and neurological complication related to increase ICP & Cerebral Perfusion Pressure (CPP). TIVA with propofol infusion is used in such cases and dexmedetomidine is used as an adjuvant reduces the anaesthetic requirement of propofol [6,7], additionally helps provide the much needed haemodynamic stability during neurosurgery.
Dexmedetomidine, a specific α(2) agonist, has an analgesic-sparing effect and reduces emergence agitation, reduces perioperative opioid use and decreases emergence agitation in children (age 2 to 10 years) posted for various surgeries like adenoidectomy, tonsillectomy, congenital hernia repair, epilepsy surgery, various orthopaedic, neurological surgeries.
A low-dose bolus of dexmedetomidine (0.5 μg/kg) used as an adjuvant can decrease the propofol requirement for children undergoing sedation for Magnetic Resonance Imaging (MRI). This may decrease the need for airway support and contribute to improved haemodynamic stability without prolonging recovery time.
Conclusion(s)
Dexmedetomidine and propofol combination provides better anaesthesia during cerebello-pontine neurosurgical procedures with respect to anaesthetic and recovery characteristics. Dexmedetomidine as an anaesthetic adjuvant improves haemodynamic stability and decreases anaesthetic requirements in patients undergoing posterior cranial fossa surgery.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 30, 2020
Manual Googling: Mar 04, 2021
iThenticate Software: Jan 16, 2021 (5%)
[1]. Andleeb R, Jain PK, Doley S, Barik AK, Safe and effective use of dexmedetomidine in anaesthetic management of a pregnant patient with posterior fossa tumor posted for ventriculoperitoneal shuntIndian Anaesth Forum 2019 20:46-47.10.4103/TheIAForum.TheIAForum_7_19 [Google Scholar] [CrossRef]
[2]. Varma M, Dubey RK, Giri MK, Mishra LD, Bis guided comparative study of dexmedetomidine and midazolam as premedicant in posterior fossa surgeriesInternational Journal of Scientific Research 2017 6(8):308-11. [Google Scholar]
[3]. Prathapadas U, Hrishi AP, Appavoo A, Vimala S, Sethuraman M, Effect of low-dose dexmedetomidine on the anesthetic and recovery profile of sevoflurane-based anesthesia in patients presenting for supratentorial neurosurgeries: A randomized double-blind placebo-controlled trialJ Neurosci Rural Pract 2020 11(2):267-73.10.1055/s-0040-170396832367982 [Google Scholar] [CrossRef] [PubMed]
[4]. Miller RD, Cucchiara RF, Miller ED, Anesthesia 2000 25th edPhiladelphiaChurchill Livingstone:2053-55. [Google Scholar]
[5]. Cole CD, Gottfried ON, Gupta DK, Couldwell WT, Total intravenous anesthesia: Advantages for intracranial surgeryNeurosurgery 2007 61:369-77.10.1227/01.neu.0000303996.74526.3018091252 [Google Scholar] [CrossRef] [PubMed]
[6]. Tanskanen PE, Kyttä JV, Randell TT, Aantaa RE, Dexmedetomidine as an anaesthetic adjuvant in patients undergoing intracranial tumour surgery: A double-blind, randomized and placebo-controlled studyBr J Anaesth 2006 97:658-65.10.1093/bja/ael22016914460 [Google Scholar] [CrossRef] [PubMed]
[7]. Sturatis M, Kroin J, Swamidoss CS, Moric M, Effect of intraoperative dexmedetomidine infusion on hemodynamic stability during brain tumor resectionAnesthesiology 2002 97:A31010.1097/00000542-200209002-00310 [Google Scholar] [CrossRef]