Mounier-Kuhn Syndrome- A Rare Case Report
Yash Rana1, Ujwal Jain2, Saket Kumar3, Arti D Shah4, Kusum V Shah5
1 Assistant Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
2 Second Year PG Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
3 Third Year PG Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
4 Professor and Head, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
5 Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ujwal Jain, Room No. 104, Gargi Hostel, Sumandeep Vidyapeeth, Piparia, Vadodara, Gujarat, India.
E-mail: ujwalkashyap1994@gmail.com
Mounier-Kuhn Syndrome (M-K Syndrome) also known as Tracheobronchomalacia (TBM) often seen in middle aged and elderly people. Weakness of the tracheal and bronchial walls allows the posterior and anterior walls to draw nearer together during expiration and coughing, producing a varying obstruction. The main complaints are dyspnoea, cough, phlegm and haemoptysis. Acquired TBM often presents with recurrent respiratory tract infections and mistreated as chronic bronchitis, pneumonia and the dyspnoea, often treated as asthma, with poorer outcomes. Here, a case of 70-year-old male was presented with complaints of cough with expectoration since four months. Bronchoscopy, cineradiography, spirometry and intrabronchial pressure measurements are the diagnostic methods used. TBM is a progressive condition and to be considered in the diagnosis of obstructive pulmonary diseases and in the assessment of the functioning capacity of dyspneic patients. Treatment is conservative and symptomatic; in selected cases surgery may also be beneficial.
Obstructive pulmonary disorders, Recurrent respiratory tract infections, Tracheobronchomalacia
Case Report
A 70-year-old male, farmer, presented in Respiratory Medicine Outpatient Department (OPD) with complaints of cough with expectoration since four months. There was progressive breathlessness since four months, grade II Modified Medical Research Council (MMRC) which was not associated with orthopnoea and paroxysomal nocturnal dyspnoea, preferably more during morning and cold climate and relieving with medications. Patient also complaints of loss of weight, loss of appetite since three months and leg ulcer over right ankle since 15 days. Patient was an ex-smoker- (5 beedis per day) with a Smoking Index of 40 and he quit smoking since last 30 years. Patient had frequent consultations for similar complaints since past four months and being treated symptomatically with antibiotics, bronchodilators. No other significant past history was presented. Family history was not significant.
On physical examination, patient was hyposthenic, poorly nourished. Pallor and clubbing (Grade II) was also present. Systemic examination revealed drooping of shoulder present on right-side with decreased movement on right side and bronchial breathing in infrascapular area with infrascapular and infraaxillary coarse crepts with increased tactile vocal resonance on right infrascapular, infra-axillary area.
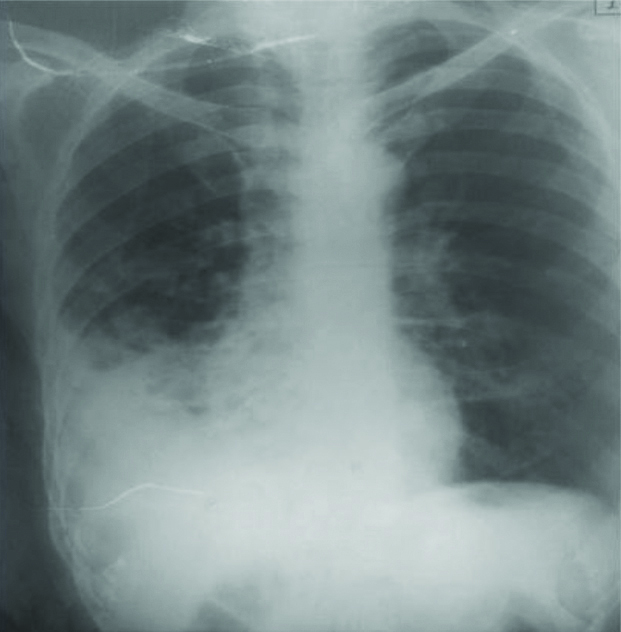
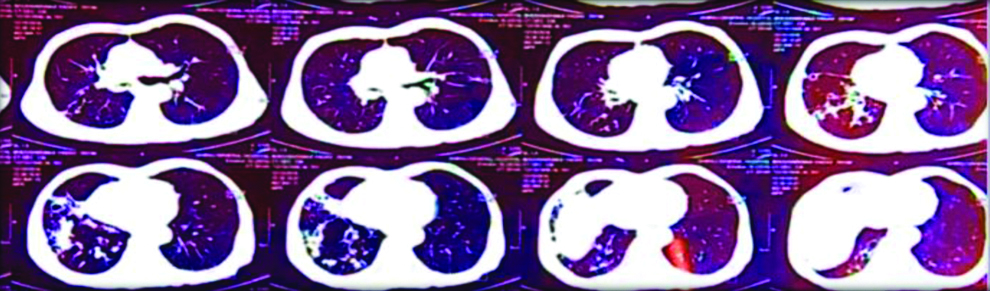
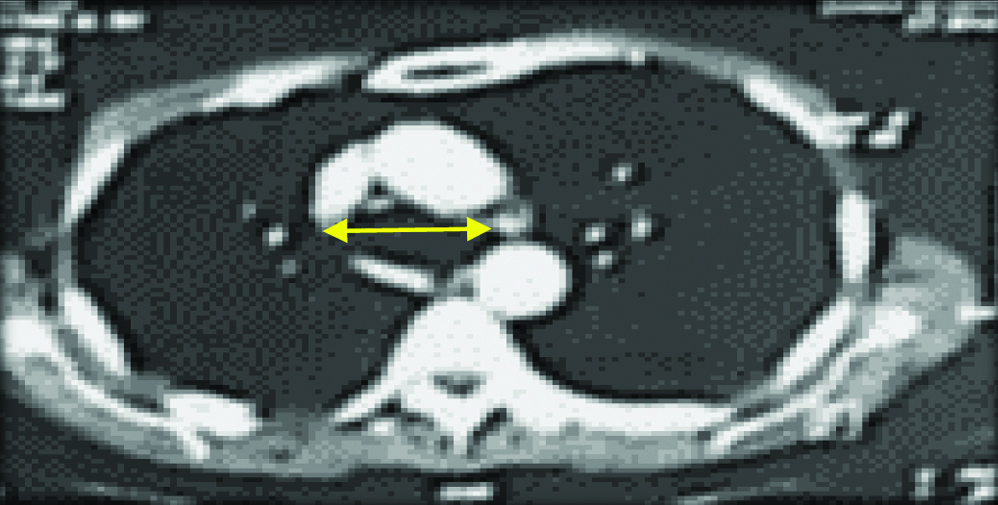
Laboratory investigations revealed Haemoglobin (Hb or Hgb) was 8.7 g/dL, Total Count (TC) was 10,700, Differential Leucocyte Count (DLC)-Neutrophils/Lymphocytes/Eosinophils/Monocyte (N/L/E/M) was 75/16/04/05, Erythrocyte Sedimentation Rate (ESR) was 76 mm/hr. Current X-ray chest was suggestive of right lower zone homogenous opacity [Table/Fig-1]. Computed Tomography (CT) thorax suspected of multiple nodular opacities in both lung fields predominantly posterior segment of right upper lobe, bronchiectactic changes in bilateral upper lobes and superior segment of bilateral lower lobes. Tracheal diameter measures approx. 22 mm Anteroposterior (AP) and 34 mm transverse (Max. luminal- ML) just above the carina and right main bronchus measures 28 mm suggestive of mildly dilated trachea and right main bronchi [Table/Fig-2a,b,3 and 4].
Chest X-ray-PA showing non homogenous opacity in right lower zone with reticular opacities in bilateral lung fields.
CT Thorax (Lung window) showing multiple nodular opacities and bronchiectatic changes in bilateral lung fields especially in the posterior aspect of upper segment and superior segment of bilateral lower lobe respectively.
CT thorax (Mediastinal window) at the level of aortic arch- showing dilated trachea (yellow arrow) and right main bronchus.
CT Thorax (mediastinal window coronal cuts) showing dilated trachea (yellow arrow) and right main bronchus. (red arrow)
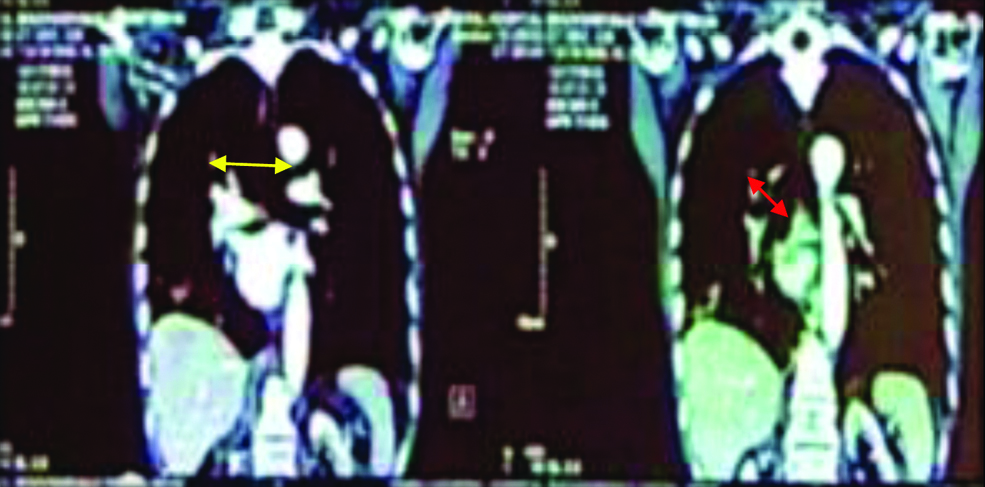
CT Thorax (Lung window-coronal cuts) showing dilated dilated trachea (yellow arrow) and right main bronchus (red arrow) suggestive of TBM.
Sputum was negative for Acid Fast Bacilli (AFB). Bronchoscopy was done and Bronchial Alveolar Lavage (BAL) was negative for AFB and hence Tuberculosis (TB) was ruled out. BAL Gram stain showed few gram positive cocci and BAL fluid Negative for fungal (KOH) stain. Patient also had a deep punched out ulcer in posterior aspect of right ankle for which pus was negative for AFB. Based on above findings, patient was diagnosed as Mounier-Kuhn syndrome with Right lower lobe pneumonia with right leg ulcer under investigation.
Patient was treated conservatively with Steam inhalation, Chest physiotherapy, antibiotics-Amoxicillin and clavulanic acid and Metronidazole, bronchodilators (levosalbutamol+Ipratropium bromide), T-Bact ointment for local application over the ulcer and discharged after stabilisation. Patient was on regular follow-up and symptomatically improved. No complications or exacerbation encountered during six months follow-up.
Discussion
M-K Syndrome is an airway disorder that causes variable airway dilatation or enlargement. It is a rare condition that occurs when the airway wall elasticity is lost or reduced and the walls specifically the trachea and bronchi become weak leading to airway narrowing or collapsibility [1,2]. The incidence of TBM varies from 4% to 23% in patients with various respiratory symptoms undergoing bronchoscopy [3].
TBM is often a missed condition. Most of the TBM cases are acquired forms, but there are a smaller subset of adult patients who have congenital TBM. Congenital anomalies usually are seen with connective tissue diseases like Marfan Syndrome, Ehlers-Danlos syndrome, Cutis laxa. Aqcuired TBM usually seen in later decades of life secondary to progressive weakning of airway smooth muscles and loss of elastic fibres [4]. The incidence of TBM varies from 4% to 23% in patients with various respiratory symptoms undergoing bronchoscopy. The exact cause of TBM is unknown in adults and is often associated with insult to the airways via external compression, trauma or chronic inflammation of the airways. The diagnosis of TBM is quiet challenging clinically as the symptoms closely resemble obstructive airway diseases and parenchymal infections and often requires radiological assistance. TBM is considered mild, if the trachea narrows to 50% of its initial size while the affected person is breathing out, moderate if it narrows to 25%, and severe if the walls of the trachea touch [3].
Patients have symptoms such as shortness of breath, cough, sputum retention (inability to clear mucus from the respiratory tract), and wheezing or stridor with breathing. Symptoms worsen during periods of stress (i.e., illness), when lying down or during forceful coughing. Treatment is advised, only if significant signs and symptoms are present, or if there is complete or near-complete collapse of the airway. Depending on severity, treatment options may include continuous Positive Airway Pressure (CPAP), stenting, surgical correction (tracheobronchoplasty), and tracheostomy. Treatment is conservative and symptomatic; in selected cases surgery may also be beneficial [5]. The author presented a case report of a patient who presented with TBM as an unusual finding.
A similar case was presented by Sivanmani K, in 2017 where a 70-year-old male presented with progressive breathlessness since two months and CXR showed bilateral lower zone reticular opacities which favoured interstitial lung disease but on CT was confirmed as bronchiectasis. Tracheal diameter was 3.8 cm, and right main bronchus and left main bronchus measured 2.9 cm and 2.8 cm which was confirmed via bronchoscopy as TBM [6]. In present case, patient was presented with similar complaints and CT thorax suggestive of- multiple nodular opacities in both lung fields predominantly posterior segment of right upper lobe favoring infective aetiology active tuberculosis which is ruled out as BAL was Negative for AFB. On CT scan- transverse diameter of trachea >3 cm and that of right and left main bronchi >2.4 cm and >2.3 cm suggestive of TBM [4]. In present case tracheal diameter measures approx. 22 mm (AP) and transverse diameter (ML) measures 34 mm just above the carina and right main bronchus measures 28 mm, hence suggested of TBM. Often TBM is associated with other tracheal anomalies like tracheal diverticulas, fistulas which were absent in this patient.
Bronchoscopy supports the diagnosis of traceobronchomalcia. No other tracheal anomalies seen. Based on the presence of characteristic signs and symptoms and abnormal findings, patient was diagnosed as Mounier-Kohn syndrome with right lower zone pneumonia with right leg ulcer. Usual management with antibiotics, bronchodilators and expectorants. Patient was kept on serial follow-up to look for severity of symptoms and airway collapsibility via CT scans [7]. TBM, even in the early stages of the disease (TBM) in presence of underlying co-morbidities increases the susceptibility to more recurrent and severe respiratory infections [8], hence prompting serial CT evaluation and appropriate treatment. Newer treatment modalities have led to improvement in prognosis and quality of life. TBD can cause acute airway collapse, and can be life-threatening [9].
Conclusion(s)
Acquired TBM usually a progressive condition and tends to worsen with time in most of patients. TBM is associated with reduced quality of life. TBM has also been associated with severe form of COVID-19.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 07, 2020
Manual Googling: Nov 21, 2020
iThenticate Software: Mar 30, 2021 (20%)
[1]. Buitrago DH, Wilson JL, Parikh M, Majid A, Gangadharan SP, Current concepts in severe adult tracheobronchomalacia: Evaluation and treatmentJournal of Thoracic Disease 2017 9(1):E57-66.10.21037/jtd.2017.01.1328203438 [Google Scholar] [CrossRef] [PubMed]
[2]. Celik B, Bilgin S, Yuksel C, Mounier-Kuhn syndrome: A rare cause of bronchial dilationTexas Heart Institute Journal 2011 38(2):194-96. [Google Scholar]
[3]. Cordier JF, Cottin V, Lazor R, Prevot G, Mounier-Kühn syndromeOrphanet 2014 [Google Scholar]
[4]. Carden KA, Boiselle PM, Waltz DA, Ernst A, Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth reviewChest 2005 127(3):984-1005.10.1378/chest.127.3.98415764786 [Google Scholar] [CrossRef] [PubMed]
[5]. Nuutinen J, Acquired tracheobronchomalaciaEur J Respir Dis 1982 63(5):380-87. [Google Scholar]
[6]. Sivanmani K, A case report of Mounier-Kuhn syndromeJ Assoc Chest Physicians 2017 5:39-41.10.4103/2320-8775.196655 [Google Scholar] [CrossRef]
[7]. López-Padilla D, García-Luján R, Puente Maestu L, de Miguel Poch E, Tracheobronchomalacia treatment: How far have we come?Journal of Thoracic Disease 2016 8(12):3490-93.10.21037/jtd.2016.12.9128149540 [Google Scholar] [CrossRef] [PubMed]
[8]. Jafari R, Cegolon L, Dehghanpoor F, Javanbakht M, Izadi M, Saadat SH, Early manifestation of ARDS in covid-19 infection in a 51-year-old man affected by Munier-Kuhn syndromeHeart and Lung 2020 49(6):85510.1016/j.hrtlng.2020.05.00532425272 [Google Scholar] [CrossRef] [PubMed]
[9]. Ma W, Liu A, Liu X, Bao F, An accidental discovery of trachebronchomegaly: A Case reportIndian J Surg 2020 https://doi.org/10.1007/s12262-020-02666-1 [Google Scholar]