Psoas group of muscle comprises of psoas major, minor, tertius, and qaudratus. Psoas major is the most constant and it is present in all individuals bilaterally and the rest are vestigial muscles present occasionally. The psoas group differs considerably in its morphology, origin, insertion and innervation [1,2]. Psoas major is a long fusiform obligatory muscle. It takes origin from the anterior surfaces of the upper four lumbar transverse processes, from the sides of the last thoracic and upper four lumbar intervertebral discs, adjacent margins of the vertebral bodies and from the tendinous arches which unite these margins. The nerve supply is by the ventral rami of L2-L4 and the femoral nerve. Its prime function is flexion of hip joint and lateral flexion of the lumbar spine [3].
Psoas minor is a small, flattened fusiform muscle. It is frequently a seat of variation. As per records, it is usually absent in trisomy 18 patients, since muscles which develop late in embryogenesis are usually affected in such patients [4]. It lies anteromedial to the psoas major. It may be unilateral or bilateral. Agenesis of this muscle is very common [5]. Psoas minor, Pyramidalis, Peroneus tertius, Palmaris longus and Plantaris are the five most common muscle to undergo agenesis. Psoas minor is the best example of a vestigial muscle [6]. Reports suggest the psoas minor has highest chances of being congenitally absent (56%) [7]. It most commonly takes origin from T12-L1 vertebra and the intervertebral disc between them. It ends in a slender, long tendon that attaches to the pecten pubis, iliopubic ramus and laterally to the iliac fascia. It is innervated by L1 ventral rami [8]. It assists in the hip joint stabilisation, flexion of the lumbar spine and a tensor of the fascia iliaca. Contraction of unilateral psoas minor causes sideway tilt of lumbar spine [7].
Clarkson RD, Rainy H, described muscle fibers from the tendon of psoas minor and merging with the psoas major and fascia iliaca [9]. This suggests the incomplete separation of psoas minor and major, during embryogenesis [5]. Psoas tertius and Psoas qaudratus could cause femoral nerve compression due to their proximity to the femoral nerve [10]. A novel psoas variant, named psoas quintus was also reported [10].
Variations with regard to its prevalence, laterality, size and variability of insertion has been noted. Its evolutionary and racial significance has also been documented. A thorough research of this small, vestigial but clinically significant muscle is indispensable. A comprehensive study of the variations in the psoas minor is vital for the radiological and clinical interpretations. It is of utmost importance for the surgeons to have an idea about the probable anomalies before operating in the defined area. Hence, the aim of this study was to investigate and study the psoas minor muscle, with regard to its frequency, agenesis, origin, insertion, morphological variations, its embryological basis and clinical significance.
Materials and Methods
This observational (cadaveric) study was carried out in the Department of Anatomy, Lady Hardinge Medical College, New Delhi (December 2018-May 2019), on cadavers used for the purpose of undergraduate teaching. The present study was based on routine dissection of the posterior abdominal wall on a total of nine cadavers (three females and six males).
The dissection process was as per the Cunningham’s Manual [3]. Once the anterior abdominal wall was dissected and all the organs were removed from the abdominal cavity, the posterior abdominal wall was dissected. To begin with, the presence of the muscle was established anterior to the psoas major muscle (when present). The Psoas minor muscle was cleaned starting from its origin upto its insertion. Any deviations of this muscle at the origin, insertion or along the entire length were noted. Photographs were taken when deemed necessary. The length and width of muscle belly as well as long tendon were gauged with the help of divider, inelastic thread, scale and digital vernier callipers. Three reading of each observation were taken and the mean of the three was taken as the final value. The laterality, morphological and other variations were noted.
Statistical Analysis
The data was tabulated and the mean, standard deviations and coefficient of correlations were calculated in Microsoft Excel.
Results
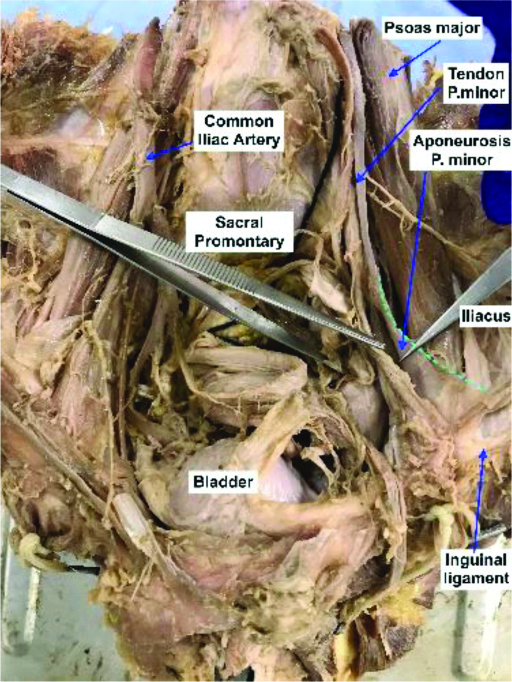
In the present study, Psoas minor muscle was present in 55.55% (5/9) cadavers. It was bilateral in 22.22% (2/9) cases (both male cadavers) and unilateral in 33.33% (3/9) cases [Table/Fig-1]. The muscle was found anteromedial to the psoas major muscle and lateral to the common iliac artery. In all the cases the muscle took origin from the T12-L1 vertebra and the intervertebral disc. However, the muscle showed a variation in its distal attachment in one of the cases.
Shows the morphometric data- the length and diameter of the muscle belly and muscle tendon.
| Psoas minor | Length | Maximum width |
|---|
| Right | Left | Right | Left |
|---|
| Cases | Gender | Present | Belly | Tendon | Belly | Tendon | Belly | Tendon | Belly | Tendon |
|---|
| 1 | Male | Bilateral | 144.8 | 102.5 | 103.4 | 115.3 | 36 | 20 | 34 | 22 |
| 2 | Female | Absent | - | - | - | - | - | - | - | - |
| 3 | Male | Bilateral | 106.1 | 144.8 | 108.2 | 144.3 | 26 | 18 | 28 | 18 |
| 4 | Female | Unilateral | - | - | 144.8 | 106.1 | | | 30 | 13 |
| 5 | Female | Unilateral | 102.9 | 135.0 | | | 24 | 18 | - | - |
| 6 | Male | Absent | - | - | - | - | - | - | - | - |
| 7 | Male | Unilateral | 116.1 | 125.8 | | - | 33 | 20 | - | - |
| 8 | Male | Absent | - | - | - | - | - | - | - | - |
| 9 | Male | Absent | - | - | - | - | - | - | - | - |
In one of the cadavers, the muscle belly was extremely short and slender, with a long tendon expanding into a triangular aponeurosis and attaching to the fascia iliac fascia, obturator internus and the medial end of inguinal ligament [Table/Fig-2]. The mean length of fleshy belly was right (Rt)-117.5 mm (with standard deviation of 19.0 mm) and left (Lt)-118.8 mm (with a standard deviation of 22.7 mm) and that of tendon was Rt-127.0 mm (with standard deviation of 18.1 mm) and Lt-121.9 mm (with a standard deviation of 19.9 mm) [Table/Fig-3].
Shows the slender tendon of Psoas Minor (P. Minor) on the left (lt) side. The P. Minor aponeurosis merging with the fascia over the Psoas Major and Fascia Iliaca as well as the Inguinal Ligament can also be seen. The margins of the Aponeurosis have been marked by green broken lines.
Descriptive statistics of the sample where psoas minor is present.
| Psoas minor | Length | Maximum width |
|---|
| Right | Left | Right | Left |
|---|
| Belly | Tendon | Belly | Tendon | Belly | Tendon | Belly | Tendon |
|---|
| Count | 4.0 | 4.0 | 3.0 | 3.0 | 4.0 | 4.0 | 3.0 | 3.0 |
| Mean (mm) | 117.5 | 127.0 | 118.8 | 121.9 | 29.8 | 19.0 | 30.7 | 17.7 |
| Standard error (mm) | 9.5 | 9.1 | 13.1 | 11.5 | 2.8 | 0.6 | 1.8 | 2.6 |
| Standard deviation (mm) | 19.0 | 18.1 | 22.7 | 19.9 | 5.7 | 1.2 | 3.1 | 4.5 |
| Coefficient of variation | 0.2 | 0.1 | 0.2 | 0.2 | 0.2 | 0.1 | 0.1 | 0.3 |
*Calculations made using excel formula
The mean maximum width of fleshy belly was found to be Rt-29.8 mm (with standard deviation of 5.7 mm) and Lt-30.7 mm (with a standard deviation of 3.1 mm) and that of tendon was Rt-19 mm (with standard deviation of 1.2 mm) and Lt-17.7 mm (with a standard deviation of 4.5 mm) [Table/Fig-3].
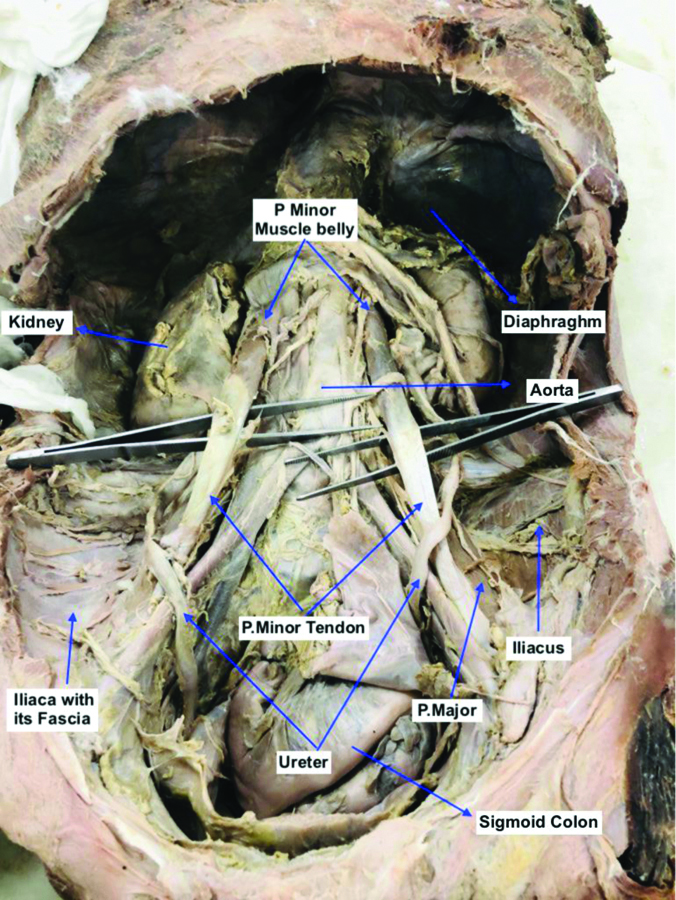
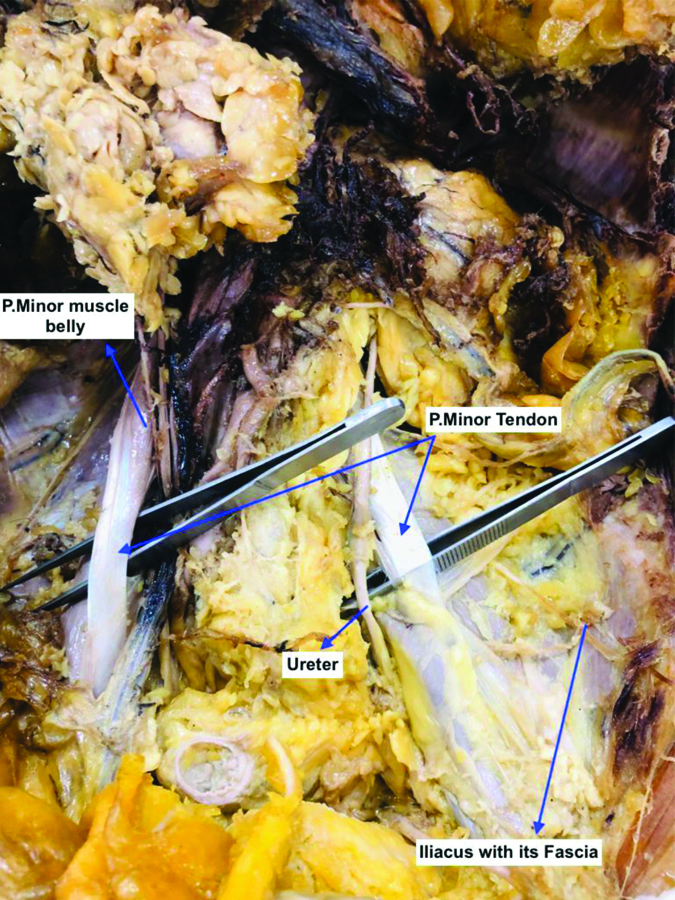
Relatively higher dispersion around the mean was noticed in width of Lt tendon, with higher coefficient of variation than others [Table/Fig-3]. The male to female ratio was 3:2. The muscle was unilateral in both the female cadavers [Table/Fig-1,4] and bilateral in two out of the three male cadavers [Table/Fig-5,6].
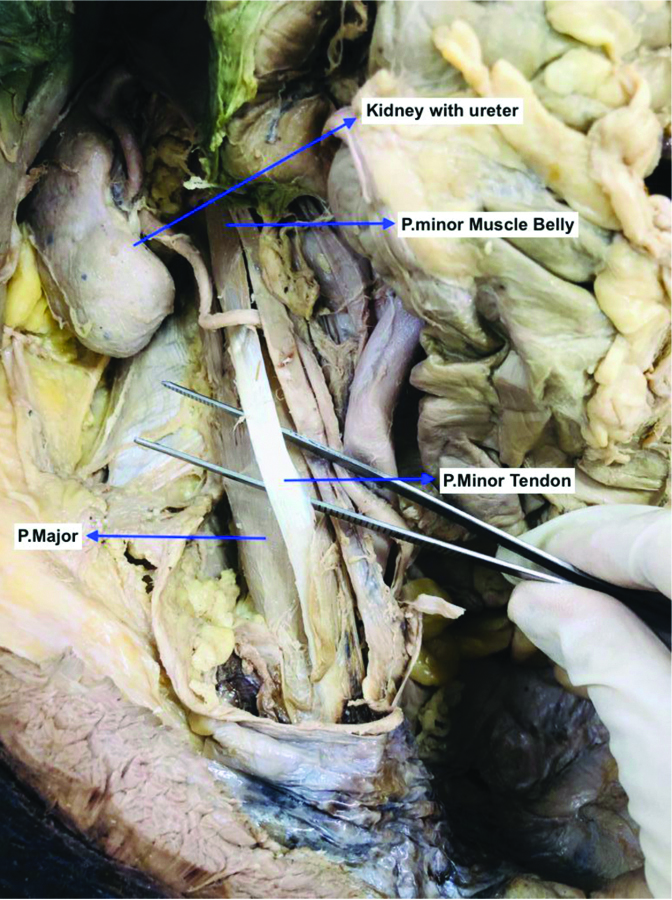
Shows right (Rt) sided unilateral Psoas Minor muscle with a slender muscle belly and tendon.
Shows bilateral Psoas Minor anteromedial to Psoas Major (P. Major). Iliacus with its fascia can been seen.
Shows bilateral Psoas Minor Iliacus with its fascia can been seen.
Discussion
Psoas minor is one of the five most common muscles that have become vestigial during the course of evolution, the others being plantaris, palmaris longus, peroneus tertius and pyramidalis [9]. The muscle is well developed in qaudripeds and brachiates that leap, run and jump. In cats the muscle is active during arching its back [11]. It has receded in humans; however, its presence is vital in certain professions such as sports and can get injured during football and other such sports [12]. The muscle shows a number of variations based on race, gender, morphology, attachment to name a few. The muscle was found in five out of nine cases in this study (55.55%). The accepted prevalence of the muscle is in the range of 33.4% and 52% [13]. Similar studies carried out in 2010 in 30 cadavers showed the presence of this muscle in 70% of the cases [14]. In 1934, Seib GA, conducted a study to investigate the occurrence of the psoas minor muscle in various races. According to his study, the muscle was present in 50% Orientals, 43% Caucasians and 33% Afro Caribbean population [15]. However, according to the findings of Hanson P et al., in 1999, the psoas minor was present in 9% Afro-Caribbean’s and 87% Caucasians [16]. The frequency of its presence was 60% in the Bulgarians, similar to the frequency in Brazilians (59%) and higher than the prevalence in Indian population (36.67%) [17]. In the USA the frequency is 65% which is much higher as compared to 35-55% in the Japanese population [18]. According to Kraychete, the muscle was found in only 30% of the cases [19]. In an observational study comprising of 2,627 cadavers, bilateral agenesis was noted in 54.5% cases [7]. According to the work done by Guerra DR et al., on foetuses, out of the 22, in 59.09% cases the muscle was present [20]. These findings were similar to the observations made by Snell RS, where the prevalence was found to be 60% [21].
Another common variation of the muscle is agenesis. Agenesis can be unilateral or bilateral. Few studies suggest the muscle to be more prone to agenesis in females [15]. Another study states the contrary and noted the muscle agenesis more frequently occurred in males [7]. The present medical consensus states no difference in the prevalence of the psoas minor muscle in the two sexes [22,23]. In the current study, the muscle was bilateral in two male cadavers [Table/Fig-1,5,6], and unilateral in the three cadavers out of which two were females [Table/Fig-1,4]. In a study on 22 foetuses, 13/22 foetuses reported the presence of the muscle. It was bilateral in 10/13 foetuses, unilateral in 3/13 foetuses [20]. According to Hanson P et al., the muscle was bilaterally in 87% white subjects and unilateral in 9% blacks [15].
The morphology of the muscle has been reported to show variations. In the present study, in all the five cases, the muscle took origin from the T12-L1 vertebra and the intervening intervertebral disc. According to literature, the muscle fibres also took origin from the L1-L2 and intervertebral disc [7,22], subdiaphragmatic fascia and medial arcuate ligament [17,24]. The muscle is generally inserted on the pectenial line (pecten pubis) and iliopubic eminence and fascia iliaca [8]. In present study, one of the cadavers had a very small muscle belly with along tendon fanning out as an aponeurosis and attaching to the pectineal line, fascia iliaca, obturator fascia extending up to medial part of the inguinal ligament [Table/Fig-2]. The remaining four cadavers had a more appreciable muscle belly and thicker tendons. The ratio of the muscle belly to its tendon varied considerably [Table/Fig-1]. The muscle was found to be more slender and tendinous in case of the two female cases [Table/Fig-2,4]. Based on previous studies, the muscle can shows wide range of variations in its insertion. Studies report the bifurcation of the tendon and the aberrant band inserts onto the synchondrosis between L5, iliopectineal line and sacrum [13,22]. A double headed psoas minor was reported by Protas M et al., [5]. The lateral head originated from L1 vertebral body whereas the medial head arose from L4/L5 vertebral body and got inserted through a common tendon onto the iliopectineal eminence. The tendon was noted to be continuous with the pelvic fascia or the iliac fascia. Guerra DR et al., in his study described variation such as insertion on the pectinial line of femur, neck of femur, lesser trochanter, the fascia iliac, inguinal ligament or pectineal ligament [20]. Ojha P et al., reported three cases of thin bellied and long fan shaped tendon psoas minor which inserted near the iliopectineal eminence, merging with the obturator fascia medially and iliac fascia laterally [25]. A similar finding was observed in the current study where one of the cases with a small muscular belly and long fanned out tendon, got inserted on the above mentioned sites as well as merged with the inguinal ligament.
Racial disparity has been reported in a number of previous studies. Morphologically, psoas minor is thicker in whites as compared to blacks. The mean length was maximum in the Indian population in comparison to Bulgarian population [16]. Joshi SD et al., in a particular study found 30% prevalence the mean length was 23.75 cm and mean width was 1.32 cm [14]. A similar study by Ojha P et al., noted the mean length to be 22.12 cm and the prevalence was 26.6% [25]. In a study, in Brazil the mean length was noted to be 23.93 cm and mean width was 1.75 cm [26]. In US, the mean length noted was 23.85 cm [27]. The mean width did not show any significant difference.
Embyrological and evolutionary basis: As per Lamarck’s “First Law,” an alteration in the environment also alters the needs and behaviour of the organisms living in that environment. This subsequently leads to an increased or decreased use of a given structure or organ. Greater use would cause the structure to enhance in size within an individual and gradually across generations, while disuse would trigger its atrophy or even disappearance [28]. The fact that anatomical structures change over time in response to environmental changes was also explained and refined by Darwin CR [29]. In humans, there are several examples of vestigial muscles like ear muscles, and various small tendinous muscles. These muscles are considered vestigial due to their lack of adaptive function, as well as their inconsistency among humans [30]. Psoas minor is well developed in quadrupeds that brachiate and hop or run at high speed. These functions are not required for bipedal gait in plantigrade man, hence the muscle has receded during evolution [31,32]. Psoas minor plays a minor role in lumbar spine flexion and its absence does not show any reduction of biomechanical or dynamic function [33]. In patients with Trisomy 18, psoas minor is consistently absent. In cases with aneuploidy, increased frequency of muscle anomalies has been reported. This is because of there is late developmental processes in them and muscles involved are usually those that differentiate relatively late during embryonic growth [4].
Clinical implications: Psoas minor, functions as an accessory to psoas major. Psoas minor syndrome is a subtype of psoas major syndrome. The psoas minor muscle is retroperitoneal and lies in juxtaposition to vital neurovascular structures in the posterior abdominal wall. Any neoplasm, haematoma, infection or abscess confined in the retroperitoneal planes is likely to involve the adjoining psoas muscle with its fascia [34]. Iliopsoas Muscle (IPM) functional disorder paints a very nonspecific clinical picture and is often neglected before being correctly diagnosed [5,35]. In case of insertion down in the femur, the muscle may be prone to overstrain. Strain in the muscle can lead to 50% decrease in flexion of hip joint. The patient may present with chronic backache, pain in the iliac fossa, difficulty in achieving an upright posture [36]. This pain usually exacerbates on palpation. The symptoms arise due to compression of neurovascular structures. The differential diagnosis could include psoas abcess, haematoma, tumour, metastasis, appendicitis, diverticulitis, salpingitis, ectopic pregnancy, ureteric calculus and must be ruled out [29]. Psoas muscle strain is encountered in sports like golf and football. The pain aggravates while playing with feet-off the ground. It leads to pain in inguinal region extending towards the abdominal wall and testis, interfering with their movements and posture.
These syndromes are often ignored since they present a vague and inconsistent clinical picture [29]. The psoas group of muscles are inaccessible for inspection and there is lack of knowledge of the IPM examination techniques. Treatment options include physical rehabilitation, opioid analgesics, muscle relaxants and surgical intervention like tenotomy [36,37].
Limitation(s)
The retroperitoneal disposition of the psoas minor would provide an insight and guide the invasive interventional procedures and differential diagnosis of simulating clinical complaints. A further study with a larger sample size backed by imaging techniques can be of significant value to anatomists, clinicians and physiotherapists.
Conclusion(s)
Psoas minor shows a significant level of variations, in terms of its origin, insertion, morphology, racial disparity as reported in the current as well as earlier studies. A comprehensive knowledge about the incidence and variations of this vestigial but clinically significant muscle is of substantial academic interest to anatomists. The role of psoas minor is often overlooked by the clinicians and academicians owing to insufficiency of its anatomical and surgical comprehension. A detailed knowledge about the muscle and its variations could help the clinicians in accessing the aetiopathogenesis, clinical scenario, differential diagnosis and treatment of the IPM functional disorders.
*Calculations made using excel formula