Bacterial Profile and Antimicrobial Susceptibility Pattern of Chronic Suppurative Otitis Media from a Tertiary Care Hospital in Kannauj, Uttar Pradesh, India
Kiran Yadav1, Sandeep Kaushik2, Kumkum Rani3, Anuj Kumar Tyagi4
1 Assistant Professor, Department of Microbiology, Government Medical College, Kannauj, Uttar Pradesh, India.
2 Professor, Department of ENT, Government Medical College, Kannauj, Uttar Pradesh, India.
3 Demonstrator, Department of Microbiology, Government Medical College, Kannauj, Uttar Pradesh, India.
4 Assistant Professor, Department of Microbiology, Government Medical College, Kannauj, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anuj Kumar Tyagi, Assistant Professor, Department of Microbiology, Government Medical College, Kannauj, Uttar Pradesh, India.
E-mail: tyagi.aiims@gmail.com
Introduction
Chronic Suppurative Otitis Media (CSOM) is a chronic and persistent inflammation of the mucosal lining of middle ear cleft which presents with recurrent ear discharge through a tympanic membrane perforation. CSOM is a worldwide disease and has higher prevalence in developing countries causing serious local damage and threatening complications.
Aim
To determine the profile of CSOM, its causative agents and their antibiotic susceptibility pattern.
Materials and Methods
The present study was a retrospective study in which data for culture and antimicrobial susceptibility profile of CSOM cases was retrieved from Microbiology Department of Government Medical College, Kannauj, Uttar Pradesh, India, from January 2019 to October 2019 and the analysis of data was done in February 2020. Two hundred pus swabs from discharging ears were processed during the study period for aerobic bacterial culture and antimicrobial susceptibility pattern in Microbiology Department using standard microbiological techniques. The result analysis of the study was expressed as percentage and proportion for distribution of CSOM cases.
Results
Out of 200 patients, 114 (57%) were males and 86 (43%) females. Among the 200 cases, 147 (73.5%) cases showed growth and 53 (26.5%) showed no growth. The most common organism isolated in this study was Pseudomonas aeruginosa 67 (42.40%) followed by Staphylococcus aureus 48 (30.37%) and Klebsiella spp. 23 (14.55%). Gentamicin (85%) and amikacin (83%) had high level of antibacterial activity on all the isolates. Meropenem was found to be most effective drug for gram negative isolates. All Staphylococcus spp isolates were sensitive to vancomycin (100%).
Conclusion
Pseudomonas aeruginosa was the most predominant organism isolated in otitis media patients. Most of the isolates were sensitive to meropenem.
Antibiotics, Ear discharge, Pseudomonas aeruginosa, Staphylococcus aureus
Introduction
The Chronic Suppurative Otitis Media (CSOM) is a chronic and persistent inflammation of the mucosal lining of middle ear cleft which may present as discharging ear. It is a worldwide disease with higher frequency in developing countries. World Health Organisation (WHO) has estimated the prevalence of CSOM in India, Tanzania, Solomon Islands, Guam, Australian Aborigines and Greenland as highest (>4%) and urgent need of attention is required to deal with the problem as it had resulted in more than 28,000 deaths globally in year 1990 due to various complications [1,2]. It is more common among patients from low socio-economic status due to overcrowding, poor nutrition, lack of health education and inadequate sanitation [3-5].
The aetiology and pathogenesis of CSOM is multifactorial and includes different causes like genetic, allergy, eustachian tube dysfunction and infection [6]. CSOM is one of the important cause in children for physician visit and can cause enormous economic burden to society [7]. The organism isolated in microbiological culture of CSOM cases can be aerobic, anaerobic or mixed with most commonly isolated organisms being Pseudomonas aeruginosa, Staphylococcus aureus, Proteus species, Klebsiella species, or anaerobic bacteria like Bacteroides, Peptostreptococcus or mixed organisms [5,8].
CSOM can lead to more serious and life threatening complications like; mastoid abscess, hearing loss, meningitis, intracranial abscess [9]. Early microbiological diagnosis and effective management could prevent serious complications later on. The changing trends of bacterial profile and antimicrobial susceptibility pattern of CSOM cases due to geographical and environmental variations in study population can address the menace of increased antibiotics abuse and thus makes it imperative to carry out the current study. Therefore, the present study was done to identify the causative organisms of CSOM infections and their antimicrobial susceptibility pattern to provide a guideline for empirical antibiotic therapy.
Materials and Methods
The present study was a retrospective cross-sectional study which was conducted on the basis of the records of 200 pus swab samples from discharging ear submitted for culture and antibiotic susceptibility testing to the Department of Microbiology in the Government Medical College, Kannauj, Uttar Pradesh, India from January 2019 to October 2019 and the analysis of data was done in February 2020. Since the study was a retrospective study ethical clearance and consent was not required.
Sample size calculation: With 95% confidence level or power and taking margin of error as 5%, the sample size calculated was 121 samples, but to be on better side, 200 samples were included for which the power of the study was 100%.
The study participants were all clinically suspected cases of otitis media that provided pus swab from discharging ears at the Microbiology Department during the study period. Age, sex profiles, results of bacterial isolates and antimicrobial susceptibility testing of patients who had ear infection were retrieved from the Microbiology laboratory using a standard data recording format.
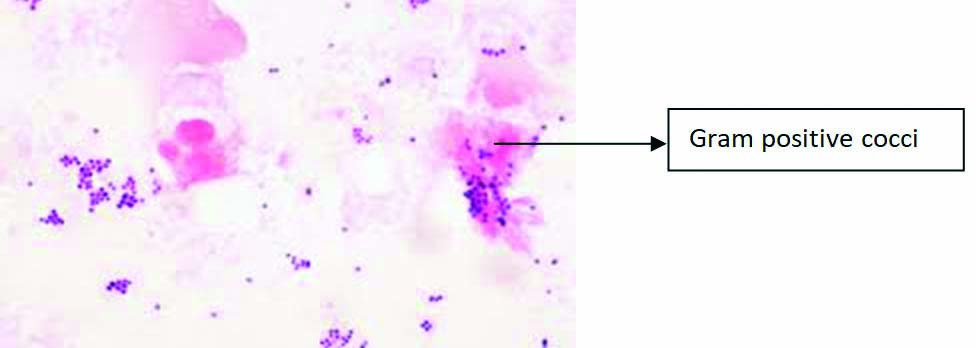
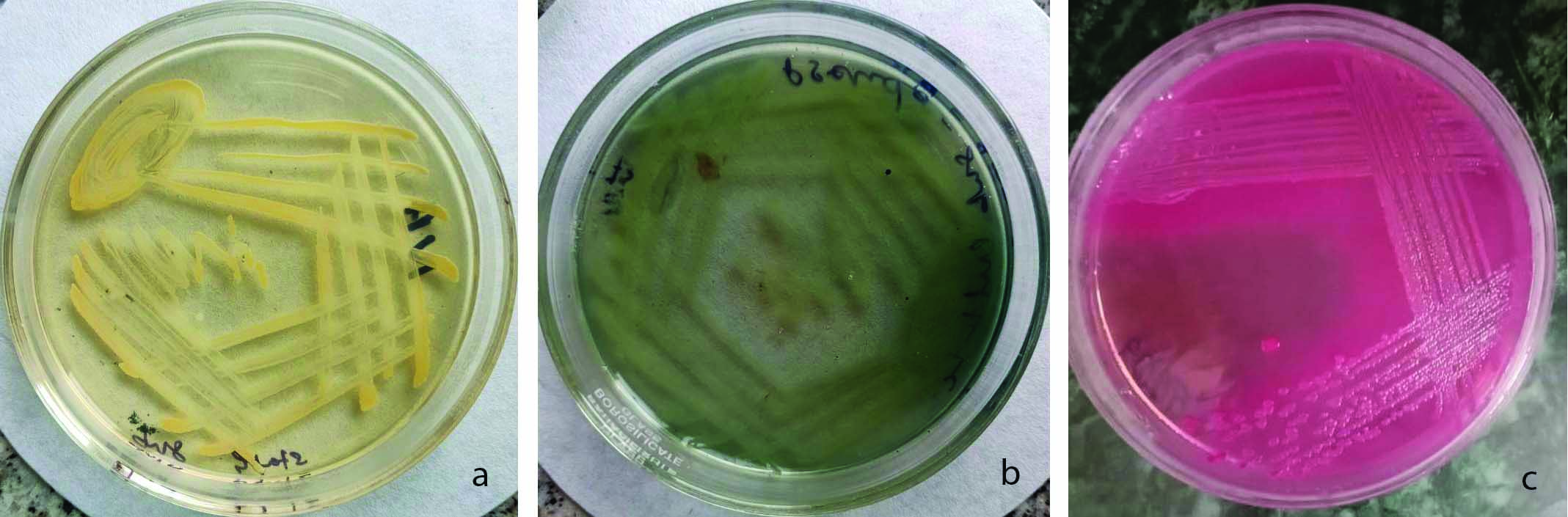
The samples were labeled with date, time, patient’s name, age and sex. Two pus samples were collected; the first swab was used for direct smear stain examination [Table/Fig-1] and the second swab for culture on 5% Sheep Blood Agar (SBA), Mac-conkey Agar (MA) and Chocolate Agar (CA). Different types of colonies in Nutrient Agar (NA) and MA is shown in [Table/Fig-2]. The SBA, MA were incubated at 37°C for 24 hours, whereas CA was incubated in candle jar generating 5% Carbon Dioxide (CO2) at 37°C for 48 hours [10]. The isolates identification was done on the basis of standard microbiological techniques like microscopic stain examination, colony morphology and biochemical testing [10]. The antibiotic susceptibility testing was done in-vitro on Muller Hinton agar using Kirby Bauer disc diffusion method using 0.5 McFarland culture suspension of isolate as per Clinical and Laboratory standard Institute (CLSI) recommendation [11]. The antibiotics used for testing were ampicillin (10 mcg), amikacin (30 mcg), amoxycillin/clavulanic acid (20/10 mcg), ceftriaxone (30 mcg), gentamicin (10 mcg), levofloxacin (5 mcg), meropenem (10 mcg) and vancomycin (30 mcg).
A standard procedure was followed to maintain the quality control in the laboratory test results. American Type Culture Collection (ATCC) control strains of Staphylococcus aureus (ATCC 25923), Escherichia coli (ATCC 25922) and Pseudomonas aeruginosa (ATCC 27853) were used for the quality control purpose [11,12].
Statistical Analysis
The result were expressed as percentage and proportion for distribution of CSOM cases according to age and gender using Microsoft Excel version 2007.
Results
A total of 200 samples were studied, of which 147 (73.5%) samples showed growth and 53 (26.5%) samples were sterile. Out of 147, 136 were pure aerobic growth and 11 samples showed mixed growth [Table/Fig-3,4]. Out of the 200 cases studied, 114 (57%) were males and 86 (43%) were females. Among the 147 cases showing microbial growth, 82 (55.8%) were males and 65 (44.2%) were females. The maximum numbers of patients were in age group 0-10 years followed by age group 11-20 years [Table/Fig-5].
Direct gram stain of ear swabs of patients with CSOM showing gram positive cocci (X1000).
a) Nutrient agar culture plate showing colonies of Staphylococcus growth; b) Nutrient agar culture plate showing colonies of Pseudomonas growth; c) Mac-conkey agar culture plate showing colonies of Klebsiella species.
Type of aerobic bacterial growth obtained from ear discharge.
| Type of aerobic bacterial growth | Total isolates (n) |
|---|
| Pure growth | 136 |
| Mixed growth* | 11 (22) |
| Total isolates | 158 |
*Mixed growth -11 samples showed polymicrobial growth with each having two different microbial growth on culture media. Total isolated microorganism:136+(11x2)=158
Distribution of polymicrobial growth pattern in CSOM cases.
| Mixed isolates | Sample |
|---|
| Staphylococcus aureus + Pseudomonas aeruginosa | 5 |
| Staphylococcus aureus +Klebsiella species | 3 |
| Pseudomonas aeruginosa +Klebsiella species | 3 |
Distribution of patients with Chronic Suppurative Otitis Media (CSOM) according to age and sex (n=200).
| Age group (years) | Males n (%) | Females n (%) | Total n (%) |
|---|
| 0-10 | 38 (19) | 23 (11.5) | 61 (30.5) |
| 11-20 | 20 (10) | 17 (8.5) | 37 (18.5) |
| 21-30 | 19 (9.5) | 13 (6.5) | 32 (16) |
| 31-40 | 14 (7) | 10 (5) | 24 (12) |
| 41-50 | 10 (5) | 11 (5.5) | 21 (10.5) |
| >50 | 13 (6.5) | 12 (6) | 25 (12.5) |
| Gender | 114 (57) | 86 (43) | 200 (100) |
In this study, it was found that unilateral infection (69%) was more common than bilateral infection (31%) and the disease was more prevalent in younger age group and among rural population (71%).
Out of the 158 (136 samples showed pure aerobic monomicrobial growth, 11 samples showed aerobic polymicrobial growth with each having two different microbial growth) bacterial isolates, 110 were gram negative bacteria, of which Pseudomonas aeruginosa 67 (42.40%) was the most predominant followed by Klebsiella spp. 23 (14.55%) and Escherichia coli 15 (9.49%). Among the gram-positive bacteria, Staphylococcus aureus was isolated in 48 (30.37%) cases [Table/Fig-6].
Frequency of isolated bacterial species from ear swabs of patients with CSOM.
| Bacteria isolated | Number | Percentage |
|---|
| Pseudomonas aeruginosa | 67 | 42.40 |
| Staphylococcus aureus | 48 | 30.37 |
| Klebsiella spp. | 23 | 14.55 |
| Escherichia coli | 15 | 9.49 |
| Enterobacter spp. | 3 | 1.89 |
| Proteus Spp. | 2 | 1.26 |
| Total | 158 | 100 |
Pseudomonas aeruginosa was the predominant organism isolated in this study, which was highly sensitive to meropenem and aminoglycoside and least sensitive to fluoroquinolone group of drugs. Staphylococcus aureus isolates were 100% sensitive to vancomycin followed by aminoglycosides and fluoroquinolone. Gram negative isolates showed high degree sensitivity to meropenem and aminoglycosides. They showed least sensitivity to penicillin, amoxicillin-clavulanic acid and cephalosporins [Table/Fig-7].
Antibiotic susceptibility pattern of isolated bacterial species from ear swabs of patients with CSOM.
| Bacteria isolated | No. | AMP % (n) | AK % (n) | AMC % (n) | CTR % (n) | GEN % (n) | LEV % (n) | MRP % (n) | VAN % (n) |
|---|
| Pseudomonas aeruginosa | 67 | NIL | 77.61 (52) | 53.73 (36) | 71.64 (48) | 80.59 (54) | 52.23 (35) | 91.04 (61) | - |
| Staphylococcus aureus | 48 | 6.25 (3) | 91.66 (44) | 70.83 (34) | 70.83 (34) | 93.75 (45) | 87.5 (42) | - | 100 (48) |
| Klebsiella species | 23 | NIL | 78.26 (18) | 60.86 (14) | 65.21 (15) | 78.26 (18) | 78.26 (18) | 91.30 (21) | - |
| Escherichia coli | 15 | 20 (3) | 80 (12) | 60 (9) | 60 (9) | 93.33 (14) | 80 (12) | 93.33 (14) | - |
| Enterobacter species | 3 | NIL | 100 (3) | 33.33 (1) | 66.66 (2) | 66.66 (2) | 33.33 (1) | 100 (3) | - |
| Proteus species | 2 | NIL | 100 (2) | 50 (1) | 100 (2) | 50 (1) | 50 (1) | 100 (2) | - |
AMP: Ampicillin (10 mcg); AK: Amikacin (30 mcg); AMC: Amoxycillin/clavulanic acid (20/10 mcg); CTR: Ceftriaxone (30 mcg); GEN: Gentamicin (10 mcg); LEV: Levofloxacin (5 mcg); MRP: Meropenem (10 mcg); VAN: Vancomycin (30 mcg)
Discussion
Otitis media is a worldwide disease with higher prevalence in developing countries, particularly among lower socio-economic section of the society [4]. In this study, males were more affected as compared to females (M:F=1.26:1), which is similar to the study done by Falagas ME et al., [13]. In present study, patients in the age group 0-10 years had high prevalence of CSOM. Other studies that have also shown the similar results [14,15]. This may be explained by short eustachian tube in small children as the infected material from nose and sinuses may trickle along the eustachian tube to the tympanic cavity [16]. In this study, 110 gram negative and 48 gram positive organisms were isolated. The frequency of bacterial isolates were Pseudomonas aeruginosa 67 (42.40%), Staphylococcus aureus 48 (30.37%), Klebsiella species 23 (14.55%). [Table/Fig-8] shows comparative chart of various studies done in the past [17-22]. The difference in the isolated organism may be due to geographical variation.
Review of literature-Isolated organisms in CSOM cases [17-22].
| Study | Pulication Year | Place | Sample size (n) | Most common isolated organism (%) |
|---|
| Deb T and Ray D [17] | 2012 | Agartala | 97 | Pseudomonas aeruginosa (37.73%), Escherichia coli (20.75%) |
| Prakash R et al., [18] | 2013 | Uttarakhand | 204 | Staphylococcus aureus (48.69%), Pseudomonas aeruginosa (19.89%) |
| Orji FT and Dike BO [19] | 2015 | Nigeria | 279 | Pseudomonas aeruginosa (44%), Staphylococcus aureus (17%) |
| Shetty AK and Shetty A [20] | 2014 | Mangalore | 80 | Pseudomonas aeruginosa (37.8%) Staphylococcus aureus (30.49%) |
| Kazeem MJ and Aiyeleso R [21] | 2016 | Nigeria | 380 | Pseudomonas aeruginosa (31.5%) Staphylococcus aureus (23.2%) |
| Ranagaiah ST et al., [22] | 2017 | Karnataka | 135 | Staphylococcus aureus (31.8%), Pseudomonas aeruginosa (31.1%) |
| Present study | 2021 | Uttar Pradesh | 200 | Pseudomonas aeruginosa (42.40%) Staphylococcus aureus (30.37%) |
In the present study, gentamicin (85%) and amikacin (83%) had high level of antibacterial activity on all the isolates. In Worku M and Bekele M study, amikacin (90%) and gentamicin (89%) had shown good results to both gram positive and gram negative isolates [23]. The most effective drug against Pseudomonas aeruginosa was meropenem (91%), followed by gentamicin (81%) and amikacin (78%). In a study done by Harshika YK et al., they found Pseudomonas aeruginosa isolates susceptible to imipenem and amikacin (93.6%) followed by gentamicin (89.3%) [24]. Staphylococcus aureus isolates were found to be maximum sensitive to vancomycin (100%) followed by good sensitivity to aminoglycosides (93%) and levofloxacin (88%). Pseudomonas species invade middle ear through defect in the tympanic membrane from an acute episode of otitis media. The high isolation of Staphylococcus aureus in CSOM cases can be due to its ubiquitous nature and high colonisation rate in external auditory canal and upper respiratory tract.
Otitis media is an important cause of hearing impairment and is a serious issue in pediatric age group. If it is not managed well in time it could led to serious effects later in the life in language development, communication skill and educational process. In current scenario, microbial profile and their antimicrobial susceptibility pattern in CSOM cases changes with time to time due to geographical and environmental variations in study population [18]. Along with that many people self medicate themselves with antibiotics which change their microbial flora and susceptibility to antibiotics. This has led to emergence of resistance in common microbes to the basic antibiotics and shifting treatment towards higher antibiotics, making the treatment more expensive and unaffordable. So, it is the urgency in today’s time to monitor the changing trends in microbial profile and their susceptible pattern to control the indiscriminate use of antibiotics, ultimately controlling the emergence of antimicrobial resistance. Poor hygiene, pond/river bath, homemade therapy for treatment i.e use of oil, honey and unconventional ear drops should also be avoided.
Limitation(s)
In the present study, 53 samples were culture sterile, which may be due to either fungal infection or some anaerobic aetiology. Further studies should be done to overcome these limitations.
Conclusion(s)
In Chronic Suppurative Otitis Media (CSOM), gram negative isolates were higher compared to gram positive isolates. Pseudomonas aeruginosa was the most predominant organism followed by Staphylococcus aureus. Thus, this study concludes that CSOM remains an ongoing problem. Time to time evaluation of microbial pattern and antibiotic susceptibility of isolates is necessary for rational antibiotic usage and successful treatment. Proper selection of topical antibiotics on the basis of culture and sensitivity with keeping the ear dry is the main modality of treatment for CSOM. The patient should be advised to take complete course of antibiotics which will prevent complications as well as emergence of drug resistance.
*Mixed growth -11 samples showed polymicrobial growth with each having two different microbial growth on culture media. Total isolated microorganism:136+(11x2)=158
AMP: Ampicillin (10 mcg); AK: Amikacin (30 mcg); AMC: Amoxycillin/clavulanic acid (20/10 mcg); CTR: Ceftriaxone (30 mcg); GEN: Gentamicin (10 mcg); LEV: Levofloxacin (5 mcg); MRP: Meropenem (10 mcg); VAN: Vancomycin (30 mcg)
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? No
Was informed consent obtained from the subjects involved in the study? No
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 31, 2020
Manual Googling: Feb 16, 2021
iThenticate Software: Mar 30, 2021 (24%)
[1]. Chronic suppurative otitis media burden of illness and management options. World Health Organisation Geneva Switzerland; 2004 [Google Scholar]
[2]. Ahmad S, Antibiotics in chronic suppurative otitis media: A bacteriologic studyEgypt J Ear Nose Throat Allied Sci 2013 14:191-94.10.1016/j.ejenta.2013.06.001 [Google Scholar] [CrossRef]
[3]. Gulya AJ, Minor LB, Glasscock ME, Poe D, Glasscock shambaugh surgery of the earPMPH-USA 2010 [Google Scholar]
[4]. Zakzouk SM, Hajjaj MF, Epidemiology of chronic suppurative otitis media among Saudi children: A comparative study of two decadesInt J Pediatr Otorhinolaryngol 2002 62(3):215-18.10.1016/S0165-5876(01)00616-4 [Google Scholar] [CrossRef]
[5]. Lasisi AO, Olaniyan FA, Muibi SA, Azeez IA, Abdulwasiu KG, Lasisi TJ, Clinical and demographic risk factors associated with chronic suppurative otitis mediaInt J Pediatr Otorhinolaryngol 2007 71(10):1549-54.10.1016/j.ijporl.2007.06.00517643499 [Google Scholar] [CrossRef] [PubMed]
[6]. Maharjan M, Bhandari S, Singh I, Mishra SC, Prevalance of otitis media in school going children in eastern NepalKathmandu Univ Med J 2006 4(4):479-82. [Google Scholar]
[7]. Niemela M, Uhari M, Mottonen M, Pokka T, Cost arising from otitis mediaActa Paediatr 1999 88(5):553-56.10.1111/j.1651-2227.1999.tb00174.x [Google Scholar] [CrossRef]
[8]. Mansoor T, Musani MA, Khalid G, Kamal M, Pseudomonas aeruginosa in chronic suppurative otitis media: Sensitivity spectrum against various antibiotics in KarachiJ Ayub Med Coll Abbottabad 2009 21(2):120-23. [Google Scholar]
[9]. Wiwanitkit S, Wiwanitkit V, Pyogenic brain abscess in ThailandNorth Am J Med Sci 2012 4(6):245-48.10.4103/1947-2714.9720022754873 [Google Scholar] [CrossRef] [PubMed]
[10]. Cheesbrough M, District Laboratory practice in tropical countries - Part 2 2000 2nd edCambridge University PressISBN- 13 978-0-521-67631-1 [Google Scholar]
[11]. CLSIPerformance standard for antimicrobial susceptibility testing; Twenty-fourth informational supplement 2014 34(1)Wayne, PAClinical and Laboratory standard Institute:CLSI document M100-S24 [Google Scholar]
[12]. Basu S, Pal A, Desai PK, Quality control of culture media in a microbiology laboratoryIndian J Med Microbiol 2005 23(3):159-63.10.1016/S0255-0857(21)02585-8 [Google Scholar] [CrossRef]
[13]. Falagas ME, Mourtzoukou EG, Vardakas KZ, Sex differences in the incidence and severity of respiratory tract infectionsRespir Med 2007 101(9):1845-63.10.1016/j.rmed.2007.04.01117544265 [Google Scholar] [CrossRef] [PubMed]
[14]. Ahmad BM, Kudi MT, Chronic suppurative otitis media in Gombe, NigeriaNiger J Surg Res 2003 5:03-04.10.4314/njsr.v5i3.12253 [Google Scholar] [CrossRef]
[15]. Shrestha BL, Amatya RCM, Shrestha I, Ghosh I, Microbiological profile of chronic suppurative otitis mediaNepalese J ENT Head Neck Surg 2011 2(2):06-07.10.3126/njenthns.v2i2.6793 [Google Scholar] [CrossRef]
[16]. Nwabuisi C, Ologe FE, Pathogenic agents of chronic suppurative otitis media in Ilorin, NigeriaEast Afr Med J 2002 79(4):202-05.10.4314/eamj.v79i4.887912625677 [Google Scholar] [CrossRef] [PubMed]
[17]. Deb T, Ray D, A study of the bacteriological profile of chronic suppurative otitis media in AgartalaInt J Otorhinolaryngol Head Neck Surg 2012 64(4):326-29.10.1007/s12070-011-0323-624294571 [Google Scholar] [CrossRef] [PubMed]
[18]. Prakash R, Juyal D, Negi V, Pal S, Adekhandi S, Sharma M, Microbiology of chronic suppurative otitis media in a tertiary care setup of Uttarakhand state, IndiaN Am J Med Sci 2013 5(4):282-87.10.4103/1947-2714.11043623724403 [Google Scholar] [CrossRef] [PubMed]
[19]. Orji FT, Dike BO, Observations on the current bacteriological profile of chronic suppurative otitis media in south eastern NigeriaAnn Med Health Sci Res 2015 5(2):124-28.10.4103/2141-9248.15362225861532 [Google Scholar] [CrossRef] [PubMed]
[20]. Shetty AK, Shetty A, Aerobic bacteriological profile and their antibiotic susceptibility in chronic suppurative otitis media in patients from Mangalore, Karnataka stateJ Acad Clin Microbiol 2014 16:03-07.10.4103/0972-1282.134454 [Google Scholar] [CrossRef]
[21]. Kazeem MJ, Aiyeleso R, Current bacteriological profile of chronic suppurative otitis media in a tertiary facility of Northern NigeriaIndian J Otol 2016 22:157-61.10.4103/0971-7749.187979 [Google Scholar] [CrossRef]
[22]. Ranagaiah ST, Dudda R, Prasad MH, Balaji NK, Sumangala B, Gudikote MM, Bacteriological profile of chronic suppurative otitis media in a tertiary care hospitalInt J Otorhinolaryngol Head Neck Surg 2017 3(3):601-05.10.18203/issn.2454-5929.ijohns20173031 [Google Scholar] [CrossRef]
[23]. Worku M, Bekele M, Bacterial isolate and antibacterial resistance pattern of ear infection among patients attending at Hawassa university referral Hospital, Hawassa, EthiopiaIndian J Otol 2014 20(4):15510.4103/0971-7749.146929 [Google Scholar] [CrossRef]
[24]. Harshika YK, Sangeetha S, Prakash R, Microbiological profile of CSOM and their antibiotic sensitivity pattern in a tertiary care hospitalInt J Curr Microbiol App Sci 2015 4(12):735-43. [Google Scholar]