The Anterior Cruciate Ligament (ACL) is the most commonly injured ligament in the knee that requires surgical intervention. The weakness of quadriceps muscle is a sequele of ACL tear that can persist even after reconstruction [1,2]. This weakness, if persists, can be hazardous to the patient as it could alter the movement strategies, decrease in functional activity and thus increases the chances of reinjury [3]. It may also delay the return of patient to daily activities and thus alter the quality of life. To optimally prepare the patient to recover, complete function of quadriceps muscle must be restored but this often not achieved despite targeted rehabilitation. Konishi Y et al., reported a 7% deficit in quadriceps volume in the reconstructed limb as compared to the contra-lateral limb 6-12 months following the ACL Reconstruction (ACLR) [4]. The weakness is proposed due to changes in morphology and the neurological mechanisms [3,5,6]. One of the hypothesis also proposed that decrease in quadriceps size might contribute to the weakness of quadriceps [7].
Understanding the effects of ACLR on size and volume of quadriceps muscle may aid in further clarification of quadriceps atrophy and strength deficits [8]. Also, structured rehabilitation programs can be planned depending on the quadriceps size. So, muscle wasting if identified in early postoperative period can help us formulate structured protocols for rehabilitation that can help patient to recover. The most common method used for this is MRI which is not feasible to use. Thus, there is a need of a method for early determination of the quadriceps thickness after ACLR surgery. It will help us formulate a plan for its reactivation and recovery well before the complications occur. The traditional method for evaluation of quadriceps thickness is by measuring cross-sectional area of thigh. But, its accuracy is varied in previous studies [7,9]. Best available method for scan of quadriceps thickness and muscle volume measurement includes MRI and CT scan [10-12], but it is neither accessible nor affordable to masses of population due to limited resources. Also, these methods are expensive and require specific equipments along with special safety procedures.
Materials and Methods
This prospective longitudinal study was conducted in Department of Orthopaedics of Tertiary Health Care Centre for a period of 12 months from 1st November 2018 to 31st October 2019 after getting approval from Institutional Ethics Committee (IEC) (IEC/SNMC/2018/152).
Inclusion criteria: All the patients between the age range of 18-45 years, with ACL tear operated only arthroscopically, with semi-tendinosus and gracilis graft used for reconstruction and those giving consent to participate in the surgery were included.
Exclusion criteria: The patients having any co-morbidity which can affect the muscle rehabilitation and strength such as polio, paralysis and any condition requiring prolonged immobilisation. Patients having any infections postoperatively, patients with multi-ligaments injuries, patients having any injury in contra-lateral knee, patients refusing to participate in study or those who did not return for proper follow-ups were excluded from the study.
All the patients were evaluated with MRI preoperatively to confirm ACL tear and were operated arthroscopically with ACLR. Total number of patients operated for arthroscopic ACL tear was 52. Out of 52 patients, four patients did not return for follow-up so those were excluded. So, the data was collected from 48 study participants and were evaluated by an independent examiner. An informed written consent was taken from all the patients prior to the study and procedure was explained.
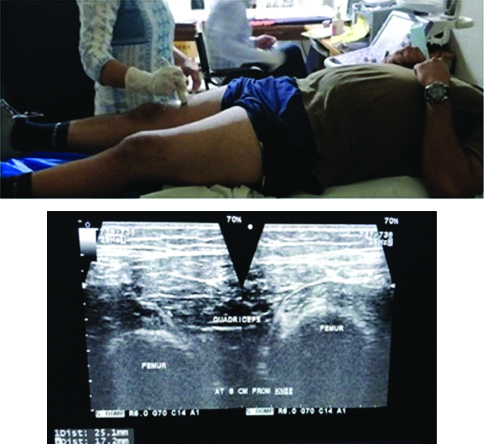
After six months of the surgery, at the follow-up the patients were evaluated for quadriceps thickness. The femur length was taken from knee joint line to Greater Trochanter (GT) and divided into three equal parts by two points, at 1/3rd of femur length and 2/3rd of femur length (from knee joint/mid of patella). USG (7mhz, Aloka portable USG machine) was then performed to measure quadriceps thickness for both the limbs [Table/Fig-1], i.e., the involved and the contra-lateral limb at these two fixed points (1/3rd and 2/3rd of femur length from knee joint) [13]. This procedure was repeated for the contra-lateral limb and measurements were compared. To maintain the uniformity, the evaluation was done by a single Radiologist in the Department of Radio-diagnosis for all the patients.
USG to measure quadriceps thickness.
On the same visit, measurement of thigh circumference was accomplished with the patient in supine position and the knee in 10 degree flexion [Table/Fig-2]. The circumference was measured with a tape at the points 1/3rd and 2/3rd of the femur length (at the same points as that of USG). This procedure was repeated for the contra-lateral limb and measurements were compared. To maintain uniformity, the evaluation was done by a single examiner for all the cases.
Calculation of thigh circumference.

Statistical Analysis
The collected data was computed in Microsoft Excel sheet. Analysis was carried out by mean and Standard Deviation (SD) for quantitative variables, frequency and proportion for categorical variables. The correlation between mean thigh circumference and muscle thickness by USG was assessed by the Pearson’s correlation coefficient. The student’s t-test was used to test statistical significance. The p-value <0.05 was considered to be significant.
Results
Out of total 48 patients, 42 (87.50%) were male and 6 (12.50%) were female. The mean age of the patients were 31.92±8.5 years. About 29 patients were operated in the right side and 19 patients were operated in left side. A total of 32 (66.7%) patients had road traffic accident as the cause of injury while sports injury was involved in 10 (20.8%) patients and household injury in 6 (12.5%) patients.
USG
All the 48 patients were reported to have decreased muscle thickness at 1/3rd of femur length point (from knee joint) and 47 patients were reported with decrease thickness at 2/3rd of femur length point (from knee joint) by USG evaluation. There was only one case observed where quadriceps thickness was not decreased in operated limb.
Thigh Circumference
Among 48 patients, 40 were reported with decrease in thigh circumference at 1/3rd of femur length point (from knee joint) and 33 were seen to have decreased thigh circumference at 2/3rd of femur length point (from knee joint) by measuring thigh circumference with measuring tape.
Evaluation at 1/3rd of Femur Length Point (from knee joint)
By thigh circumference and USG evaluation method quadriceps muscle thickness were recorded in operated limb and compared with the contra-lateral limb at 1/3rd of femur length point from knee joint [Table/Fig-3]. This comparison was statistically significant (p<0.05).
Paired t-test used for evaluation (1/3rd of femur length).
| Variables | In operated limb | In contra-lateral limb |
|---|
| Mean circumference by measuring tape (cm) | 45.75 | 48.18 |
| Mean thickness by USG evaluation (mm) | 21.15 | 24.47 |
| SE (mean) by thigh circumference method | 0.46 | 0.46 |
| SE (mean) by USG evaluation | 0.31 | 0.47 |
| Deficit (mean) by thigh circumference method | 5.04%p-value: 0.0003 |
| Deficit (mean) by USG evaluation | 23.05%p-value: 1.02E-07 |
The correlation between mean thigh circumference and muscle thickness by USG at this point was assessed and found to be negative (r=-0.16); p-value <0.05 considered significant; USG: Ultrasonography
Evaluation at 2/3rd of Femur Length (from knee joint)
By thigh circumference and USG evaluation method quadriceps muscle thickness were recorded in operated limb and compared with the contra-lateral limb at 2/3rd of femur length from knee joint [Table/Fig-4]. This comparison was statistically significant (p<0.05).
Paired t-test used for evaluation (at 2/3rd of femur length).
| Variables | In operated limb | In contra-lateral limb |
|---|
| Mean circumference by measuring tape (cm) | 54.29 | 56.87 |
| Mean thickness by USG evaluation (mm) | 32.87 | 37.475 |
| SE (mean) by thigh circumference method | 0.69 | 0.77 |
| SE (mean) by USG evaluation | 0.50 | 0.66 |
| Deficit (mean) by thigh circumference method | 4.43% p-value: 0.015 |
| Deficit (mean) by USG evaluation | 11.72% p-value: 1.50E-07 |
The correlation between mean thigh circumference and muscle thickness by USG at 2/3rd from knee joint was assessed and found to be only mildly positive (mild; r=0.20). Here, p-value was 0.08, which was not significant. Thus, there was no strong correlation established between measurements by USG and thigh circumference
Discussion
The purpose of this study was to determine the effect of ACLR on quadriceps muscle thickness. Literature states that ACLR can lead to weakness of quadriceps muscle that can last from months to years [2,7]. In this study, quadriceps muscle thickness were measured using USG to identify the atrophy pattern in the early phase after ACLR and correlated it with their matched uninvolved extremities. This study quantifies quadriceps thickness at two distinct levels of the thigh and found a significant deficit of 13.05% in the involved extremity at 1/3rd of femur length from knee joint and a deficit of 11.72% in involved extremity at 2/3rd of femur length from knee joint. It is established that the quadriceps of the involved extremity definitely goes under atrophy despite early rehabilitation and mobilisation.
Various studies conducted previously have used MRI for evaluation of quadriceps thickness post ACLR. Arangio GA et al., in his study used MRI for quantification of quadriceps in cross-sectional area and found 8.6% deficit in the involved limb as compared to uninvolved limb [9]. In this study, USG has been used as it is an easily available and affordable alternative of MRI. Studies like Pardo E et al., have reported that USG can be used to quantify quadriceps muscle thickness [14] which was further supported by Giles LS et al., stating that MRI and USG provide equivocal results for the evaluation of quadriceps thickness [15]. Both the studies have significantly compared the advanced modalities like USG and MRI with the conventional thigh circumference method and supported the findings of this study. Yang JH et al., studied effects of ACLR on individual quadriceps muscle thickness using USG and found a significant reduction in thickness postoperatively [16]. In a recent study by Garcia SA et al., rectus femoris Cross-Sectional Area (CSA) were evaluated after ACLR via ultrasound imaging and bilateral reductions in rectus femoris CSA were noted where only the uninvolved limb returned to preoperative CSA and the involved limb failed to return to preoperative levels [17].
Thigh circumference was also measured using conventional tape methods and observed a deficit of 5.04% at 1/3 of femur length from knee joint and 4.43% at 2/3rd of femur length from knee joint in the operated limb as compared to uninvolved limb. Many studies have previously reported comparable deficits using thigh circumference. Arangio GA et al., observed 1.8% decrease in thigh circumference in the involved extremity [9]. Yoshii R et al., evaluated thigh circumference and showed increase in subcutaneous fat CSA and decrease in quadriceps muscle CSA lead to effective decrease in thigh circumference on the operated side [18]. In this study, there was no positive correlation between thigh circumference measurements and muscle thickness using USG (negative pearson co-efficent at 1/3rd of femur length and very mild positive at 2/3rd of femur length). The conventional method of measuring thigh circumference using tape falsely underestimates the wasting. Gerber C et al., reported that the difference in thigh circumference between an injured and uninjured leg explained only 32% of the difference in muscle cross-sectional area [19]. Yoshii R et al., also reported that thigh circumference measurements might not imitate real muscle CSA in ACL patients [18]. There are two possible explanations for this:
Firstly, the subcutaneous fat or other tissues can vary between a person’s injured and uninjured lower extremity.
Secondly, the disuse of an injured limb will result in a reduction of muscle tone, which causes the thigh cross-section to lose its round shape.
Muscle size is a primary determinant of muscle strength among healthy individuals without a history of joint injury. It has been hypothesised that central nervous system alterations and thigh muscle atrophy work in concert to cause persistent quadriceps weakness in the involved limb following ACLR [8]. However, it is largely unclear to what degree muscle size is a determinant of this persistent weakness. So, it is important to identify wasting at an early stage of ACLR to prevent persistent weakness and periodically assess the quadriceps muscle thickness in individuals after ACLR. Saxena S et al., in his very recent study used USG to measure muscle girth after 12-14 weeks post-ACLR and showed a different progressive recovery of the muscle girth as 31% and 10% for supervised and unsupervised groups respectively [13]. Thus, muscle wasting if detected early postoperatively can help for supervised rehabilitation protocols for the patient.
This study brings to notice that despite aggressive rehabilitation protocols, quadriceps still gets wasted after ACLR since its wasting is not even checked periodically after surgery. Longer duration studies like this with larger sample size must be done in future to obtain a better understanding of pattern of quadriceps wasting after ACLR using standard protocols. This must be a routine to evaluate quadriceps during rehabilitation as this can help us modify or restructure existing protocols for early return of patient to routine activity. Also, acute wasting can be prevented to convert into chronic atrophy that becomes very difficult to recover. Early detection of muscle size can also help in starting early rehabilitation protocols by using various newer modalities like Blood Flow Restriction (BFR) therapy and drug therapy. BFR to the affected extremity during low intensity resistance training is hypothesised to significantly increase muscle size and thus help in recovery. The mechanism proposed for this is anaerobic respiration by the muscles can lead to their hypertrophy [20]. Drugs can also be used for muscle atrophy prevention if administered early and include ghrelin agonists, selective androgen receptor molecules, espindolol, and skeletal muscle troponin inhibitors [21].
Limitation(s)
There were certain limitations in present study. Possible explanations of persistent quadriceps atrophy in present study patients include significant preoperative atrophy. Authors did not measure preoperative muscle thickness in this study. Also, authors did not include comparisons of healthy controls to better understand the differences between healthy quadriceps muscle morphology and that of patients with ACLR. This study suggests that inclusion of muscle size assessment in evaluating the clinical outcomes post ACLR would aid in developing a clearer understanding of the timing of quadriceps atrophy, influencing short and long term outcomes after ACLR.
Conclusion(s)
Quadriceps atrophy is found in widespread cases after ACLR even after standard rehabilitation protocols. Quadriceps wasting should be determined in postrehabilitation phase by USG, which is an easy available and accessible option as compared to MRI and CT scans. Selective rehabilitation protocols can further be established if wasting is identified early. This can prevent the conversion of acute wasting into chronic atrophy and should be a standard protocol after ACLR. Measurement of thigh circumference cannot be considered as a standard protocol for the same as it underestimates the atrophy and can be misleading.