Spontaneous Rupture of Spleen in Acute Pancreatitis: A Rare Case
Sharvari Shashikant Gulve1, Pratap Singh H Parihar2, Rutuja Pratap Singh Parihar3
1 Junior Resident, Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Datte Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
2 Professor, Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Datte Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
3 Intern, Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Datte Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sharvari Shashikant Gulve, Junior Resident, Department of Radiodiagnosis, Acharya Vinobha Bhave Rural Hospital, Wardha-442001, Maharashtra, India.
E-mail: sharvari23@yahoo.com
Spontaneous rupture of the spleen is a rare disorder and has been reported to occur due to Haematological, neoplastic and infectious diseases involving the spleen. We present a case of 25 years young male who presented with epigastric pain and fever since four days. The contrast-enhanced computed tomography scan showed complete distortion of splenic architecture with perisplenic mixed density collection that suggested splenic rupture. Pancreas was bulky in the tail region with adjacent fluid density collection. The peripancreatic fluid in the tail region eroded the splenic capsule and penetrated into splenic parenchyma causing spontaneous rupture of the spleen. It also eroded the vessel and caused haematoma. Splenic artery embolisation was done and later managed conservatively.
Complications, Computed tomography, Pancreas, Splenic rupture
Case Report
A 25-year-old male presented with history of abdominal pain in epigastric region and fever since four days. The pain was initially mild then gradually increased and aggravated on having food. There was no history of vomiting. The patient denied history of trauma. The patient was alcoholic and last consumption was two days before the epigastric pain started. Patient had no history of diabetes or hypertension. On physical examination, pulse was 120 bpm, blood pressure was 110/70 mm of hg, respiratory rate was 18/min. On routine lab test haemoglobin was 5.4%, WBC was 17400/L and haematocrit was 16.4. The ultrasonography of the patient was done which revealed heterogenous and bulky pancreas in tail region with hypoechoic area in spleen. On further investigations, liver enzymes were deranged. Serum Glutamic Pyruvic Transaminase (SGPT)-584, Serum Glutamic Oxaloacetic Transaminase (SGOT)-750 and bilirubin-2.8 IU/L. serum amylase was 444 IU/L and lipase was 941 IU/L.
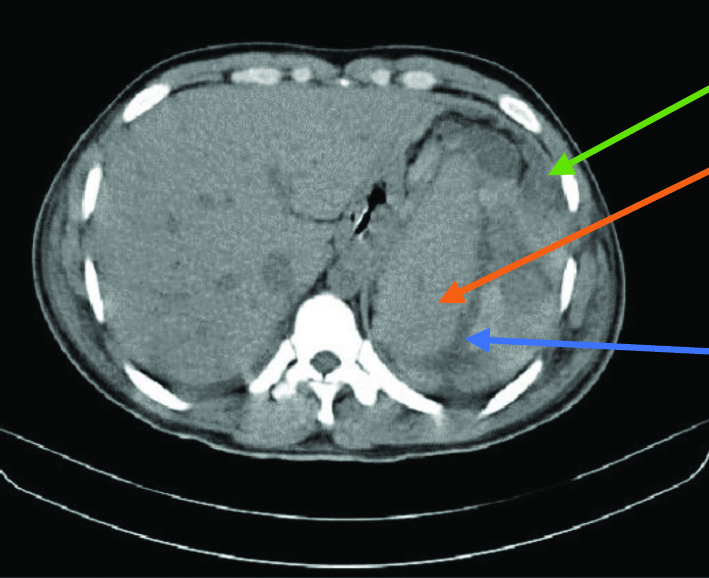
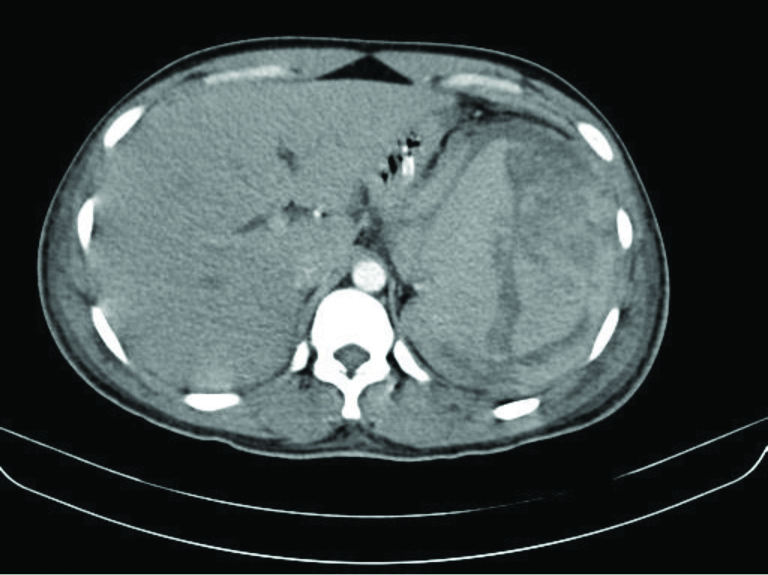
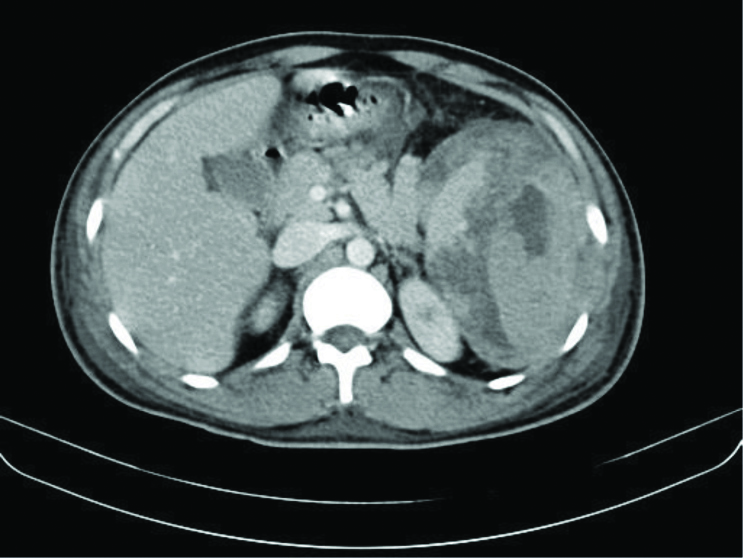
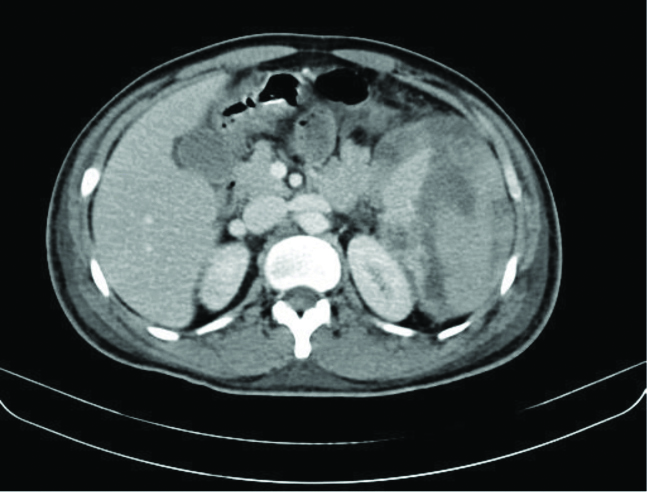
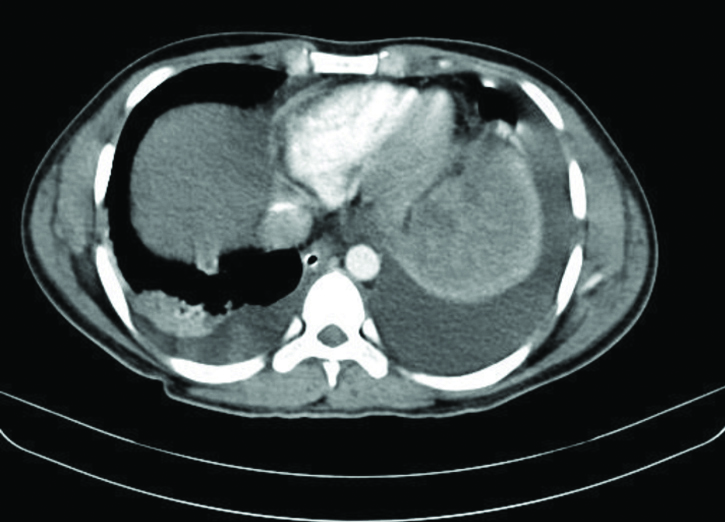
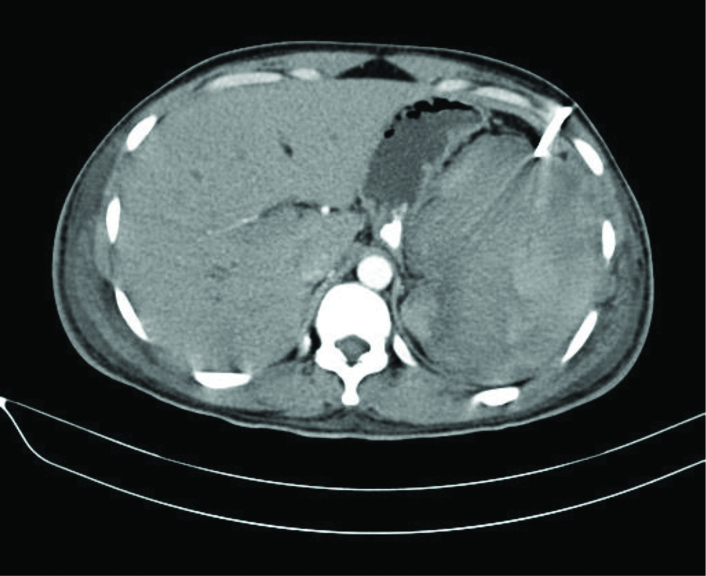
Noncontrast computed tomography showed enlarged spleen with perisplenic collection and linear hypodensity in splenic parenchyma [Table/Fig-1]. The contrast-enhanced computed tomography was done which revealed complete distortion of splenic architecture with heterogeneously enhancing areas within and capsulated fluid density collection with parts of normal spleen embedded within. It was approximately measuring 16×13×11 cm [Table/Fig-2,3]. Pancreas were bulky with peripancreatic fluid collection in the region of tail [Table/Fig-4]. Liver was enlarged. There was evidence of ascites and bilateral pleural effusion [Table/Fig-5]. Based on this the diagnosis of acute pancreatitis with modified CTSI of 6 (moderate acute pancreatitis) with spontaneous splenic rupture was done. The patient was treated with splenic artery embolisation and pigtail catheter and later managed conservatively by antibiotics and antiemetics. The postoperative CT scan was done which showed pigtail catheter near abdominal wall on left side [Table/Fig-6]. The patient was kept under observation for 14 days. The ascites regressed eventually however, haematoma took time to regress. The patient was haemodynamically stable after 14 days, after which the patient was discharged. Patient did not come for follow-up later.
Noncontrast computed tomography showing enlarged spleen (red arrow) with perisplenic collection (green arrow) and linear hypodensity in splenic parenchyma (blue arrow).
Contrast-enhanced computed tomography revealed complete distortion of splenic architecture with heterogeneously enhancing areas within with nonenhancing hypodensities and capsulated fluid density collection.
The contrast-enhanced computed tomography revealed perisplenic fluid density collection, with distortion of the splenic parenchyma causing displacement of pancreatic tail.
Contrast-enhanced computed tomography showing peripancreatic fluid collection in the region of tail of pancreas.
Contrast-enhanced computed tomography showing bilateral pleural effusion.
Postoperative noncontrast CT scan shows perisplenic hyperdense collection and artifact due to catheter.
Discussion
The anatomical relationship between the tail of the pancreas and the splenic hilum allows the spread of pancreatitis-induced inflammatory processes into the spleen. The pancreatic tail extends along the course of the splenic vessels to enter the splenic hilum. It is located within the two layers of peritoneum which constitute the spleno-renal ligament. The peritoneum that is covering the anterior surface of the pancreas and enclosing the splenic vessels is continuous with the splenic capsule. This anatomic association allows the leaked pancreatic enzymes to dissect postero-laterally along the splenic vessels to get access to the splenic hilum and capsule [1,2]. Various types of pancreatic fluid involvement are seen which include perisplenic, intrasplenic, and mixed. In perisplenic involvement, the fluid dissects the splenic peritoneal layer from the splenic capsule not including it. Direct intrasplenic involvement occurs due to pancreatic enzymes which erodes the splenic capsule. The fluid collection adjacent to splenic parenchyma penetrates into the splenic parenchyma via the disrupted capsule. Rarely, it is caused by pancreatitis occurring in ectopic or intrasplenic pancreatic tissue or due to liquefaction of splenic infarct. Spontaneous splenic rupture and haematoma are unusual complications of pancreatitis which causes detrimental consequences and even a fatal outcome [3]. CT is valuable for identifying splenic complications, as well as for patient follow-up [4,5]. It helps to determine the volume of collection and compare it with the previous scan. Depending upon the haemodynamic status of the patient, the management of splenic complications varies. For the patients who are haemodynamically stable, treatment options include a conservative approach, percutaneous drainage, angiography study, embolisation and surgery. However, use of a conservative approach requires strict follow-up with serial ultrasound or CT scan [4,6,7].
Hernani BL et al., presented a case in which there was splenic rupture and haematoma due to acute severe pancreatitis, haemoperitoneum and extravasation of contrast in splenic vein [4]. In this case, there was splenic haematoma and haemoperitonium.
In a case report by Jain D et al., atraumatic splenic rupture with pancreatitis was observed with fluid density collection along the tail of pancreas with perisplenic haematoma [3]. The haematoma was well localised [3]. In present case, there was total disruption of splenic parenchyma while in case by Jain D et al., the rupture was near the posterior surface of spleen.
According to the case report by Torricelli P et al., in a spontaneous rupture of spleen pancreatic pseudocyst can erode the splenic capsule and cause haemorrhage [8]. Thus, splenic rupture is rare complication of the pancreatitis with varied presentations.
Conclusion(s)
Spontaneous splenic rupture is rare complication of pancreatitis. The presence of peripancreatic fluid collection, splenic vein thrombosis, pancreatitis involving tail of pancreas is the potential risk factor. High degree of clinical suspicion is required for prompt diagnosis and treatment. Contrast-enhanced computed tomography is most comprehensive and sensitive diagnostic modality for spontaneous splenic rupture.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 04, 2020
Manual Googling: Dec 07, 2020
iThenticate Software: Jan 15, 2021 (20%)
[1]. Patil PV, Khalil A, Thaha MA, Splenic parenchymal complications in pancreatitisJournal of the Pancreas: JOP 2011 12(3):287-91.21546711 [Google Scholar] [PubMed]
[2]. Fishman EK, Soyer P, Bliss DF, Bluemke DA, Devine N, Splenic involvement in pancreatitis: Spectrum of CT findingsAmerican Journal of Roentgenology: AJR 1995 164(3):631-35.10.2214/ajr.164.3.78638847863884 [Google Scholar] [CrossRef] [PubMed]
[3]. Jain D, Lee B, Rajala M, A traumatic splenic hemorrhage as a rare complication of pancreatitis: Case report and literature reviewClinical Endoscopy 2020 53(3):31110.5946/ce.2019.08731337192 [Google Scholar] [CrossRef] [PubMed]
[4]. Hernani BL, Silva PC, Nishio RT, Mateus HC, Assef JC, De Campos T, Acute pancreatitis complicated with splenic rupture: A case reportWorld Journal of Gastrointestinal Surgery 2015 7(9):21910.4240/wjgs.v7.i9.21926425272 [Google Scholar] [CrossRef] [PubMed]
[5]. Sharada S, Olakkengil S, Rozario AP, Occult splenic rupture in a case of chronic calcific pancreatitis with a brief review of literatureInternational Journal of Surgery Case Reports 2015 14:95-97.10.1016/j.ijscr.2015.06.01526255003 [Google Scholar] [CrossRef] [PubMed]
[6]. Lankisch PG, The spleen in inflammatory pancreatic diseaseGastroenterology 1990 98(2):509-16.10.1016/0016-5085(90)90848-U2403954 [Google Scholar] [CrossRef] [PubMed]
[7]. Mujtaba G, Josmi J, Arya M, Anand S, Spontaneous splenic rupture: A rare complication of acute pancreatitis in a patient with Crohn’s diseaseCase Reports in Gastroenterology 2011 5(1):179-82.10.1159/00032721521552441 [Google Scholar] [CrossRef] [PubMed]
[8]. Torricelli P, Coriani C, Marchetti M, Rossi A, Manenti A, Spontaneous rupture of the spleen: Report of two casesAbdominal Imaging 2001 26(3):290-93.10.1007/s00261000015811429955 [Google Scholar] [CrossRef] [PubMed]