Owing to the increased life-span of the modern era, spinal column diseases like trauma, osteoporosis, metastasis and vertebral fractures have been increased tremendously within the last decade [1,2]. PVP is a traditional minimal invasive procedure consisted of injection of Polymethylmethacrylate (PMMA) into the Vertebral Collapse (VC) to obtain a rapid pain relief and mechanical strengthening of the vertebral body. Due to the high temperature of cement reaction, local sensory small nerve endings denervation is another pain control mechanism of PVP [2]. PVP procedure, which is frequently used by orthopaedists and neurosurgeons had been introduced firstly by Galibert P, Deramond H et al., to deal with aggressive vertebral haemangiomas [1].
The main indications of PVP are painful Thoracolumbar Vertebral Fractures (TLVF) due to primary or secondary osteoporosis, neoplastic lesions, trauma and haemangiomas [2-4]. Although PVP is an effective treatment modality to reduce vertebral pain due to variant conditions, many complications related to the procedure have been described like post-surgical pain, radiculopathy, spinal cord compression, pulmonary embolism, cardiac perforation, infection and rib fractures. Some studies have categorised complications as TLVF related, procedure related and material introduction related complications [2-6].
The aim of this retrospective study was to address the complications frequently encountered during the PVP procedure.
Materials and Methods
This retrospective study was conducted in Department of Neurosurgery, Faculty of Medicine, Dokuz Eylul University, after obtaining the Ethical Comittee approval for the study, (Letter no.2020/15-53).
All cases of PVP procedures performed between January 2005 and June 2012 were retrospectively reviewed.
Inclusion criteria: Active mobile patients without associated severe co-morbidities were included in the study.
Exclusion criteria: Patients with severe vertebral fracture collapse (vertebra plana), multiple vertebral metastasis, quadriplegic and bed-ridden patients were excluded from the study. Out of 1375 patients operated with PVP, 601 patients with a 652 vertebral levels have been included in this study.
Preoperatively and during the follow-up periods which ranged from 4 to 16 months average 7.3±5.2 months. As a standard protocal in the Neurosurgery Department, all patients were asked to quantify the pain according to the Visual Analogue Scale (VAS), which is considered as a valid measure of acute pain with a good construct validity [7]. Patterns of cement leakage were evaluated after getting a postoperative x-ray and Computerised Tomography (CT) for all patients who underwent PVP procedure.
Statistical Analysis
The software used was SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL, USA). The p-values were accepted as significant at <0.05.
Results
Out of the 601 patients {244 (40.5%) males, 357 (59.5%) females}, mean age was 63.04±7.4 (range 34 to 90) years. A total of 551 patients underwent surgery at one level, 49 patients at two levels, whereas one patient underwent surgery at three levels. Surgery was performed for 389 patients (64%) with osteoporotic fracture, 146 patients (24%) with metastatic fracture, 41 patients (6.8%) with traumatic fractures, 5 patients (0.8%) with haemangiomas and 3 patients (0.5%) with solitary plasmacytoma. The most frequently reported symptom at the time of admission was back pain in all patients (100%), followed by radicular pain in 102 patients (17%). The most frequent neurological finding was sensorial loss in 78 patients (12%), motor deficit in 47 patients (8%) and sphincter disturbances in 19 patients (3%).
Demographical data of patients have been demonstrated in [Table/Fig-1,2].
Preoperative deomgraphic and clinical history data of the patients.
| Demographic data | Female | Male | Osteoporotic fracture | Metastatic fracture | Traumatic fractures | Haemangioma | Solitary plasmacytoma |
|---|
| Number of patients | 357 (59.5%) | 244 (40.5%) | 389 (64%) | 146 (24%) | 41 (6.8%) | 5 (0.8%) | 3 (0.5%) |
| Present complaints | Back pain | Radicular pain | Sensory loss | Motor deficit | Sphincter disturbance | |
| Number of patients | 601 (100%) | 102 (17%) | 78 (12%) | 47 (8%) | 19 (3%) | |
The distribution of the vertebral levels involved in this study.
| Level | No. of patients | % |
|---|
| T3 | 1 | 0.15% |
| T4 | 1 | 0.15% |
| T7 | 9 | 1.40% |
| T8 | 6 | 0.93% |
| T9 | 14 | 2.14% |
| T10 | 24 | 3.68% |
| T11 | 25 | 3.84% |
| T12 | 240 | 36.8% |
| L1 | 241 | 36.96% |
| L2 | 58 | 8.89% |
| L3 | 19 | 2.91% |
| L4 | 9 | 1.38% |
| L5 | 5 | 0.77% |
| Total | 652 | 100% |
Same day mobilisation with a supporting brace was allowed for all patients, except for four cases that underwent revision decompression surgery. PVP surgery for adjacent level fractures was performed in four out of five patients that had disc space cement leakage during the initial surgery, whereas PVP had been performed for another non-adjacent levels in three patients. The same type of bone cement was used for all patients (Biomet Bone Cement R 1×40). The mean preoperative VAS was 8.51±1.5, whereas after one and six months the mean postoperative VAS were 1.94±1.0 and 2.53±2.2, respectively. Central spinal canal leakage was observed in four cases; three of them had developed transient monoparesis and varient radiculopathy symptoms for at least one month duration. The fourth patient developed paraplegia [Table/Fig-3].
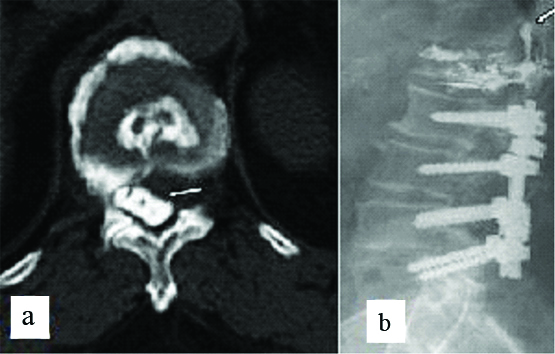
a) Cement leakage into the spinal canal seen on (axial) computerised tomography scan; b) Cement leakage into the spinal canal seen on (lateral view) fluoroscopy.
The cement leakage had been tolerated well by one patient with a remarkable symptomatic resolution occurred within one month. Whereas, decompressive foraminotomy had been performed for two patients on the 24th and 38th days postoperatively; due to intractable radicular pain. Both patients had recovered completely at three and five months after surgery, respectively [Table/Fig-4]. Immediate total laminectomy and decompression surgery had been performed for removal of the cement leakage to the spinal canal for the patient who developed total paraplegia, however just minimal sensorial improvement had been recognised one year after the surgery.
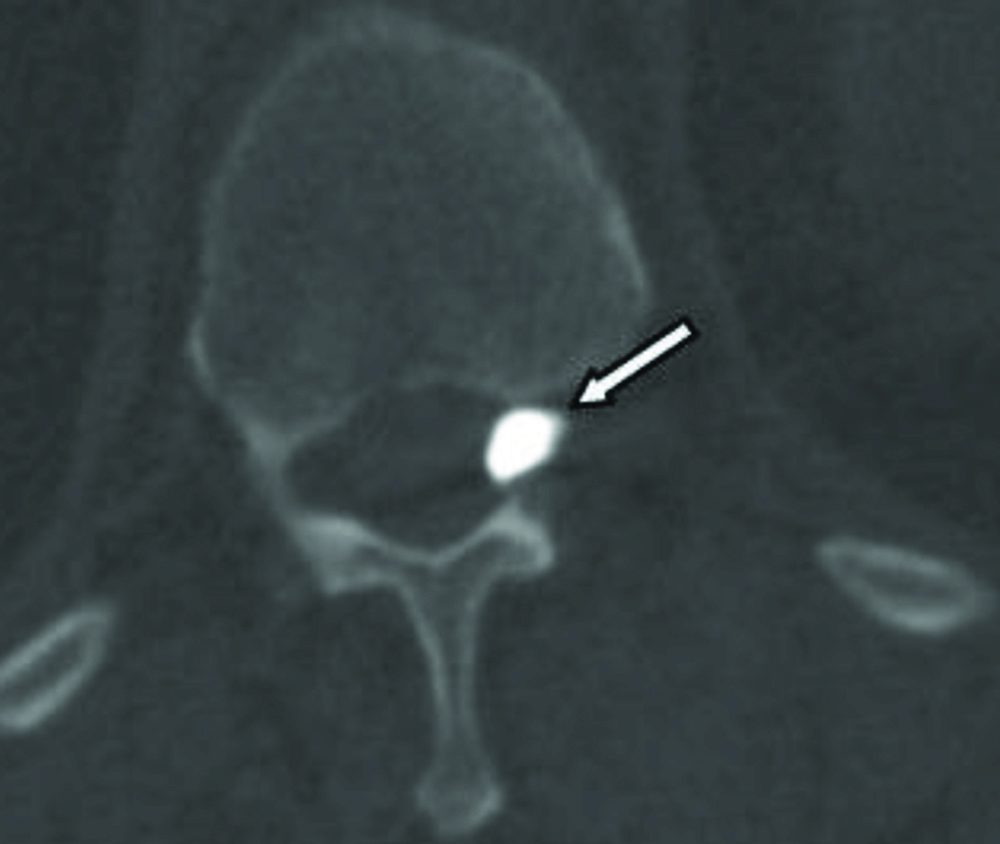
Cement leakage into the intervertebral foramen discovered in (axial) computerised tomography of the affected vertebrae.
Asymptomatic leakage had been recognised beneath the posterior longitudinal ligament in 42 patients (6.9%), beneath the anterior longitudinal ligament in 18 patients (2.9%) and into disc space in 31 patients (5.1%) [Table/Fig-5]. Venous leakage occurred in four patients (0.6%) patients, and was asymptomatic in all of them [Table/Fig-6].
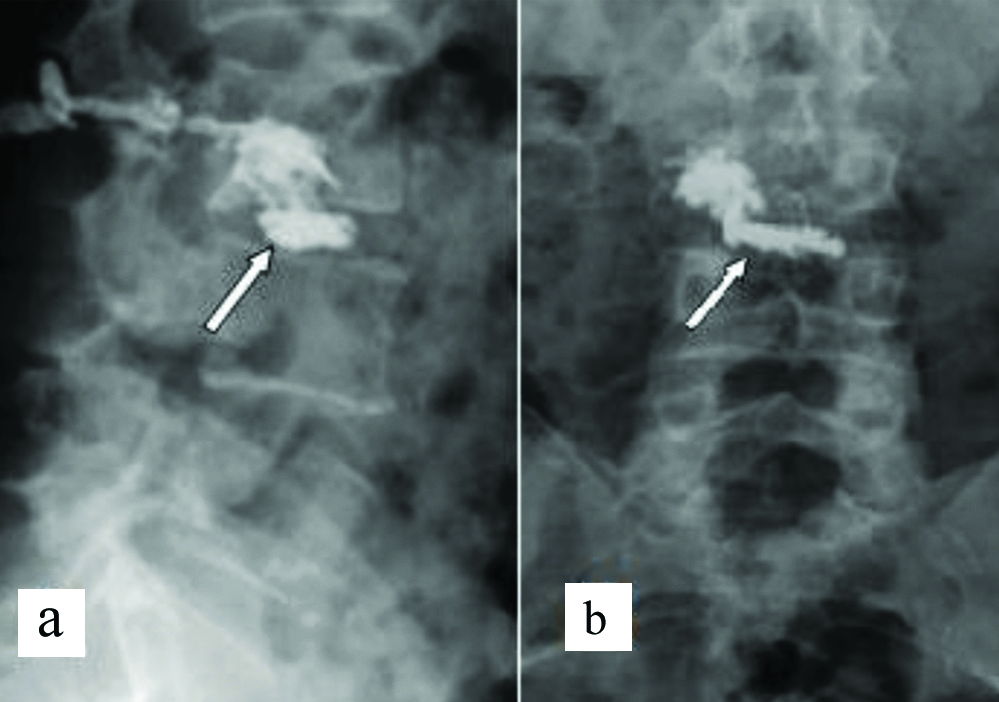
a) Anteroposterior and b) Lateral views of cement leakage into the intervertebral disc and pedicle.
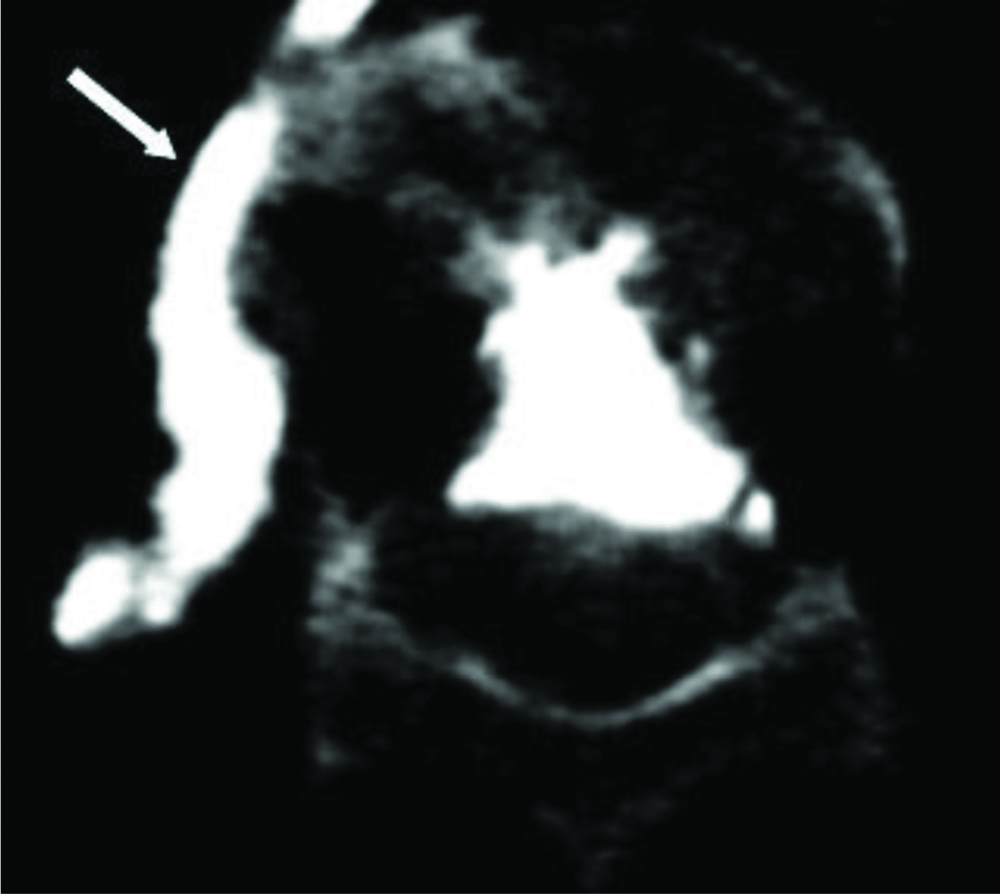
Cement leakage around vena cava seen on (axial view) computerised tomography.
Discussion
The PVP procedure has increased tremendously within the last decade and is becoming mostly the more common minimal invasive surgical method to deal with the annoying localised pain related to osteoporotic compression fractures of the spine without noticeable epidural compression [8-10]. Transient symptomatic worsening has been documented as a frequent complication after PVP [9]. The aim of this study was to address the frequantly encountered complications of 601 cases underwent PVP procedure.
As for the whole study group, the mean visual analog pain scale decreased from a preoperative average value of 8.51±1.5 to 1.94±1.0 at one month following operation.
Several studies have demonstrated that, the complications rate after PVP is considered very low, however can be devastating. Different complications like intraoperative hypotension, transient fever, infection, temporary worsening of the fracture pain, rib or adjacent segment fracture, cement leakage, neurological deficit and vascular injuries [9,10]. leakage of cement frequently occuring during the procedure is the main source of clinical complications after PVP [11]. Cement leakage has been reported to occur in 38% to 72.5% of patients with malignant collapse [11,12]. Fortunately, it is well tolerated in the large majority of patients.
Zhan Y et al., in their systematic review, comparing vertebroplasty with kyphoplasty in the treatment of cancer-related vertebral compression fractures, reported that cement leakage occurred in 37.9% PVP patients [13]. Chen W et al., in their meta-analysis of randomised controlled study reported that, unilateral PVP approach decreases the incidence of cement leakage [11]. Cement may leak into a large variety of adjacent compartments including, instrumentation tract, the paravertebral soft tissue in 6% to 52.5% of patients and the spinal canal in up to 37.5% of patients [11,12]. Other studies showed that cement may leak through intervertebral disc in 5% to 25%, around the paravertebral veins in 5% to 16.6%, and the epidural veins in 16.5% of patients. Cement leakage into the metameric artery, inferior vena cava, aorta and lungs has also been reported [14,15].
Cement leakage through disc spaces has been proven by some studies to increase the probability of adjacent vertebra fracture [11,16,17]. It is well known that, cement leakage into the spinal canal is due to destruction of the posterior cortex of the injuried vertebra. In patients who have soft tissue mass in the anterior part of the spinal canal such as in aggressive haemangiomas and malignant diseases, cement extravasation mostly occurs through the soft tissue mass. When there is enough residual space for the thecal sac, cement leakage through the spinal canal is well tolerated [14-18]. In this study, cement leakage into the spinal canal occurred in four cases. Although it has been tolerated well by one patient, transient monoparesis which had been resolved postoperatively occurred in two patients and paraplegia occurred in one patient.
Cement leakage is very common when using the standard postero-lateral approach which crosses the foramen [19]. However, in this study cement leakage into the foramen was less frequently encountered since the transpedicular approach was used. Spinal canal and foraminal cement leakage can be the result of fractures through the inferior and medial cortices of the pedicle at the time of the intervention. Peh WCG et al., reported intervertebral disk space leakage in 35% of patients series who have severe Vertebral Canal (VC) and concluded that leakage was not dependent on the shape of the VC (vertebra plana, gibbous deformity, H shape) [18]. Intervertebral disk leakage is mostly asymptomatic, however it may have long-term mechanical consequences on adjacent vertebrae [19,20]. Cement leakage around veins is a frequent complication after PVP surgery. It doesn’t carry serious effect on the vein itself, but may cause pulmonary embolism. Venous leakage may extend into the inferior vena cava without causing a significant clinical symptom. Padovani B et al., documented a case of pulmonary embolism with a good outcome [21]. Scroop R et al. had documented in a 78-year-old woman, a paradoxical cerebral arterial embolisation with a pulmonary embolism of cement after a multilevel vertebroplasty [22]. Multiple cement pulmonary emboli have been found to increase the risk of pulmonary hypertension and right-to-left shunting into the venous circulation through a patent foramen ovale [23]. This occurred mainly due to failure of recognising venous migration of cement emboli during the procedure. Aebli N et al., in an experimental study on animals, found a cement string, wrapped into an ovoid shape approximately 3 cm long in a main pulmonary artery in one sheep [23]. In this series, venous leakage occurred in four patients and was asymptomatic in all of them. In this retrospective study, two patients underwent decompressive foraminotomy on the 24th and 38th postoperative days due to intractable radicular pain, whereas one patient underwent total laminectomy and removal of the leaked cement from the spinal canal at the 9th minute of the intervention due to motor and sensorial deficits of the lower extremities immediately noticed during the PVP procedure. The authors’ PVP experience stress upon the fact that, PVP should be performed in a fully prepared operation theater in case of the necessity to revert immediately to open surgery in case of cement leakage into the spinal canal.
Limitation(s)
The retrospective nature of this study did not permit a thorough assessment of the predisposing factors that may lead to cement leakage, other than vertebral body cortex fracture.
Conclusion(s)
This study reveals the fact that, PVP procedure is associated with serious complications and it would be more wise to perform such a procedure in a fully equipped operation theater to allow urgent surgical intervention to prevent palpable devastating complications associated with cement leakage into the spinal canal.