There is a vast difference in lesions of the GIT in different segments. Broadly the whole GIT can be divided into upper and lower segments by taking the insertion of ligament of Treitz as a landmark. The disorders of LGIT are responsible for a great number of morbidity. The immune system deals with large number of antigens in the intestine which is a principle site for it. The GIT is a common site for numerous pathological processes from non-neoplastic, pre-neoplastic to neoplastic. Gastrointestinal tumours constitute one of the major causes of morbidity and mortality worldwide and include both benign and malignant tumours. They continue to be the second leading cause of cancer related deaths in the developed world. The early detection and treatment of gastrointestinal neoplasms has been shown to improve patient’s survival significantly [1]. More common lesions from biopsies of LGIT are infection, inflammation, toxic and physical trauma, vacular disorders etc. Various polyps in GIT are hyperplastic, inflammatory, adenomatous and carcinomatous polyps. Biopsies can give the diagnosis without major surgical resection as it helps to reach at inaccessible sites of lesions. Biopsies are also used to monitor the course of the disease, extent of the disease, to detect complications and to assess the response to therapy. Hence, they are considered gold standard investigation for GI lesions [2]. Intestinal lesions are common complaints of all ages, benign lesions being commoner in early ages while malignant lesions being commoner in advancing age. Over 75% of intestinal lesions are benign in nature [3].
The aim of this study was to find out the common lesions of LGIT and trace the cause of the same retrogradely so as to reduce the prevalence of that common diseases. Further the objectives of this study were as follows:
Materials and Methods
An observational retrospective study of various LGIT biopsies sent for HPE at Smt. B.K.Shah Medical Institute and Research Centre, Pathology Department of tertiary care centre, Vadodara, Gujarat, India was carried out. Study was based on the histopathological evaluation of lower gastrointestinal lesions received in the duration from 1st June 2019 to 30th September 2020 (1 year and 3 months), and analysis was done between 1st October 2020 to 15th October 2020. In this study, the records of lower GI specimens were included. Patient’s brief clinical history, age, In Patient Department (IPD) number and patients presenting sign and symptoms were included.
A total of 600 specimens were analysed.
Sample size was calculated with the formula [4]:

where n=Sample size,
Z=Z statistic for a level of confidence,
P=Expected prevalence or proportion
(If the expeted prevalence is 20%, then P=0.2), and d=precision (If the precision is 5%, then d=0.05
The gross examinations of the tissues were carried out and appropriate sections were taken from various sites.
Tissue was processed in fully automated tissue processor by passing through various grades of alcohol, xylene and paraffin wax. After tissue processing paraffin embedded tissue blocks were prepared. From this block 3-5 μm thick sections were cut and stained with Haematoxylin and Eosin (H&E) stain. The sections were evaluated under light microscope.
Method:
Dewax sections in xylene (giving two changes of xylene) for 5 minutes each.
Hydrate sections in descending grade of alcohol for 5 minutes each and wash them briefly in distilled water.
Stain with haematoxylin for 3 minutes.
Wash well in tap water for five minutes till sections are blue.
Differentiate in 1% acid alcohol (1% HCI in 70% alcohol) for 5-10 seconds. (One dip only)
Wash in tap water till sections are blue.
Stain in 1% eosin Y for 2 minutes.
Wash in tap water for 1-2 minutes.
Dehydrate trough ascending grade of alcohol
Clear in Xylene and mount with DPX.
Statistical Analysis
Results were interpreted as percentages and presented in tables.
Results
Among all the 600 case, non-neoplastic lesions 570 (95.0%) were more common than neoplastic lesions cases 30 (5.0%).
Age and sex wise distributions of lower GIT lesions. Incidence of lower GIT lesions are more in 2nd and 3rd decades followed by 4th decades and less in 7th decades and least in 8th decades. All the lesions are more common in male than female [Table/Fig-1].
Age and sex wise distribution of lower GIT lesions.
| Age (years) | Male | Female | Total | Percentage |
|---|
| 1-10 | 20 | 8 | 28 | 4.66% |
| 11-20 | 56 | 29 | 85 | 14.16% |
| 21-30 | 97 | 49 | 146 | 24.33% |
| 31-40 | 99 | 47 | 146 | 24.33% |
| 41-50 | 51 | 46 | 97 | 16.16% |
| 51-60 | 36 | 22 | 58 | 9.66% |
| 61-70 | 19 | 9 | 28 | 4.66% |
| 71-80 | 5 | 5 | 10 | 1.66% |
| 81-90 | 1 | 1 | 2 | 0.33% |
| Total | 384 | 216 | 600 | 100% |
Among 600 cases, 249 (41.50%) cases were of lesion of appendix, followed by lesions of small intestinal and caecum, colon and rectum in decreasing order of cases. Out of 249 cases of appendix, 247 cases are non-neoplastic, only 2 cases are neoplastic. Out of 158 cases of small intestine and caecum, 148 cases are non-neoplastic and only 10 cases are neoplastic [Table/Fig-2].
Distribution of lower GIT lesions according to type and site of lesions.
| Site | Non-neoplastic | Neoplastic | Total | Percentage |
|---|
| Small intestine and caecum | 148 | 10 | 158 | 26.33 |
| Rectum | 35 | 4 | 39 | 6.50 |
| Anal Canal | 59 | 2 | 61 | 10.16 |
| Appendix | 247 | 2 | 249 | 41.50 |
| Colon | 81 | 12 | 93 | 15.50 |
| Total | 570 | 30 | 600 | 100 |
Out of 570 non-neoplastic lesions, majority of non-neoplastic lesions were of appendiceal lesion 247 (43.33%) followed by non-specific inflammation 138 (24.21%) [Table/Fig-3].
Distribution of lower gastro-intestinal tract non-neoplastic lesions according to histopathological examination.
| Type | Number of cases | Percentage |
|---|
| Non-specific inflammation | 138 | 24.21 |
| Gangrene | 25 | 4.39 |
| Inflammation with perforation | 17 | 2.98 |
| Inflammation with ulceration | 48 | 8.42 |
| Tuberculous inflammation | 19 | 3.33 |
| Amoebiasis | 4 | 0.70 |
| Gastrointestinal stromal tumour | 4 | 0.70 |
| Hircshsprung’s diseases | 4 | 0.70 |
| Meckel’s diverticulum | 10 | 1.75 |
| Polypoidal lesions | 7 | 1.23 |
| Coeliac diseases | 2 | 0.35 |
| Ulcerative colitis | 3 | 0.53 |
| Fistula | 9 | 1.58 |
| Crohn’s diseases | 2 | 0.35 |
| Tubular adenoma | 1 | 0.18 |
| Atresia | 1 | 0.18 |
| Haemorrhoids | 29 | 5.09 |
| Non-neoplastic appendiceal lesions | 247 | 43.33 |
| Total | 570 | 100 |
Out of 30 neoplastic lesions, most common were of adenocarcinoma 15 cases (50%) followed by mucinous adenocarcinoma 5 cases (16.67%). Cases of non-hodgkin’s lymphoma are least only 3.33% [Table/Fig-4].
Histopathological type wise distribution of lower GIT neoplastic lesions.
| Type | Number of cases | Percentage |
|---|
| Adenocarcinoma | 15 | 50 |
| Signet ring carcinoma | 3 | 10 |
| Mucinous adenocarcinoma | 5 | 16.67 |
| Gist | 4 | 13.33 |
| Non-hodgkin’s lymphoma | 1 | 3.33 |
| Squamous cell carcinoma | 2 | 6.67 |
| Total | 30 | 100 |
Discussion
The LGI biopsies in the diagnosis and treatment of intestinal pathology remain as the gold standard and widely used. Screening of LGIT pathology by endoscopy and diagnosis by endoscopic biopsies are becoming more frequently used for early diagnosis of gastrointestinal pathology in recent years due to increase in people’s awareness level about cancer and cancer prevention. In the present study, age and sex distribution, type and site of the lesions were analysed.
In present study, of 600 cases of LGIT lesions, 570 (95%) cases were non-neoplastic and 30 (5%) were neoplastic. Among 570 non-neoplastic lesions, majority were of appendiceal lesions. Among neoplastic lesions, large proportion was of adenocarcinoma.
In the comparative study done by Nanavati MG et al., there were 157 cases of non-neoplastic lesion comprising 78.5% of total 200 cases which were less as compared to present study [5]. In both studies, non-neoplastic lesions were more common than neoplastic lesions [Table/Fig-5].
Comparison between non-neoplastic and neoplastic lower GIT lesion [5].
| Lesions | Nanavati M et al., [5] (2014) | Present study (2021) |
|---|
| Number of cases | Percentage (%) | Number of cases | Percentage (%) |
|---|
| Non-neoplastic | 157 | 78.5 | 570 | 95.0 |
| Neoplastic | 43 | 21.5 | 30 | 5.0 |
| Total | 200 | 100 | 600 | 100 |
In the present study, the peak age of neoplastic lesions was 41-70 years and male to female ratio is 1.7:1. In the comparative study of Sharma P and Deka M it was 61-70 years and male to female ratio was 1.9:1. In both studies, male preponderance was seen [6].
In the present study, adenocarcinomas comprise 50% of neoplastic lesions of LGI, while in the study of AbdulKareem FB et al., 87.1% cases are of adenocarcinomas and in the study of Patel Mandakini M et al., 76.2% of adenocarcinomas [Table/Fig-6] [7,8]. In both the studies overall adenocarcinomas were more common in the neoplastic lesions of LGI [7,8].
Comparative histological type of lower GI lesions [7,8].
| Types of neoplasm | AbdulKareem FB et al., [7] (2008) | Patel Mandakini M et al., [8] (2012) | Present study (2021) |
|---|
| Adenocarcinoma | 366 (87.1%) | 61 (76.2%) | 15 (50%) |
| Mucinous Adenocarcinoma | 06 (24%) | - | 5 (16.67%) |
| Signet ring cell carcinoma | 02 (8%) | 03 (3.7%) | 3 (10%) |
| Nonhodgkin’s lymphoma | 01 (4%) | 02 (2.5%) | 1 (3.33%) |
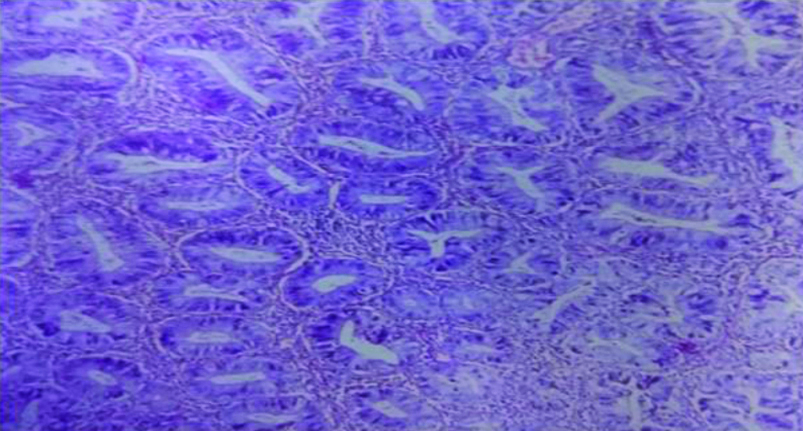
In tubular adenoma, polypoidal colonic mucosa covered with dysplastic epithelium arranged in pseudostratified manner was seen [Table/Fig-7]. Out of 570 cases, only one case of tubular adenoma was noted. In comparison with the study of Siddiqui B et al., from 44 cases of LGIT biopsies, only four cases were of tubular adenoma [9].
Tubular adenoma (H&E Stain, 40X)-Composed of neoplastic tubules lined by tall columnar stratified epithelium.
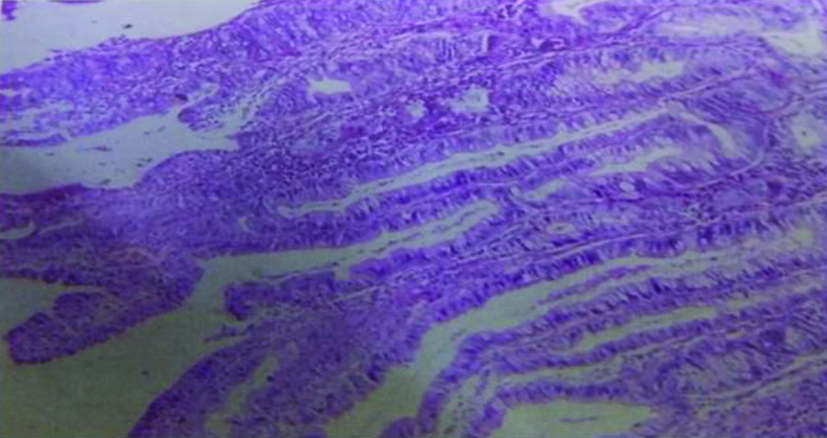
In villous adenoma, pointed processes of lamina propria which is lined by displastic pseudostratified columnar epithelium was seen [Table/Fig-8].
Villous Adenoma (H&E Stain, 40X)-Composed of finger like processes lamina propria covered by tall columnar epithelium.
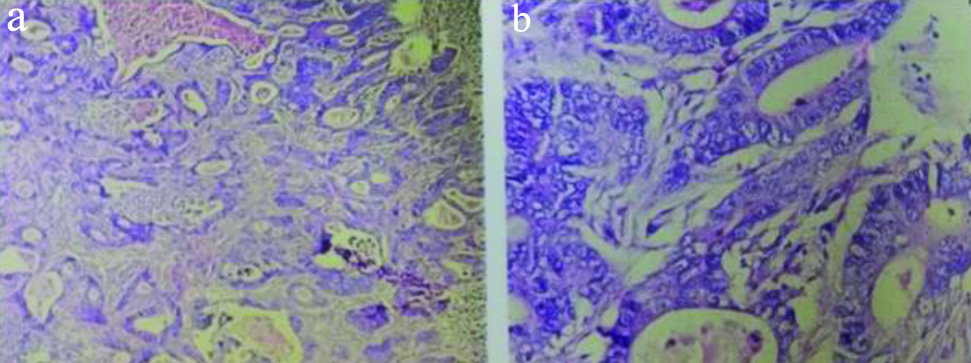
In the LGIT, Adenocarcinomas were the commonest malignant tumour. 15 out of 30 malignant cases (50%) were reported. The most common grade in present study was Grade 2 i.e., moderately differentiated adenocarcinoma. [Table/Fig-9] constituting of all adenocarcinomas which is similar to the study of Venkatesh V and Thaj RR [2]. In this, irregular tubules with nuclear pleomorphism was seen.
Moderately differentiated adenocarcinoma. Irregular tubules with nuclear pleomorphism are seen. a. (H&E Stain 10X) b. (H&E Stain 40 X).
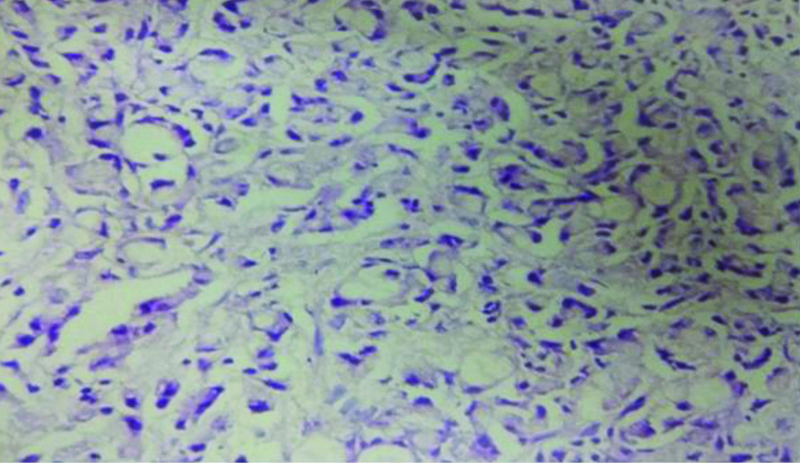
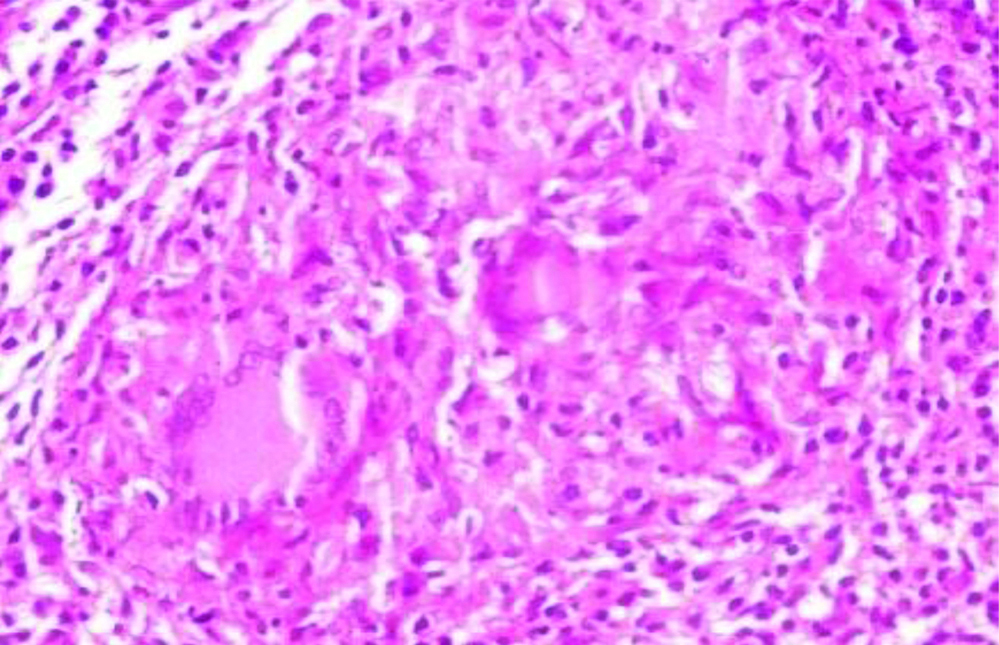
Three cases out of 30 malignant cases (l0%) were of Signet ring adenocarcinoma [Table/Fig-10] in comparision with the study of Suvernakar SV et al., in which out of 67 cases only three cases (4.5%) were of signet ring cell adenocarcinoma [10]. In this, cells having intracellular mucin which displaced the nuclei to side. Pools of extracellular mucin were also present.
Signet ring cell adenocarcinoma. Cells having intracellular mucin and displaced nuclei (H&E Stain, 40X).
Out of 570 cases, 19 cases have tuberculous inflammation. In this, granulomas were seen with central necrosis and peripheral epitheloid cells, lymphocytosis and giant cells [Table/Fig-11].
Giant cells in granuloma in case of tuberculosis of appendix-Granulomas with central necrosis, peripheral lymphocytosis and giant cells. (H&E Stain, 40X)
Limitation(s)
In the present study, the sample size was low and the study analysed the data of only one geographical region.
Conclusion(s)
A wide variety of neoplastic and non-neoplastic lesions were diagnosed in the present study. In small intestine, non-neoplastic lesions were common while most of the malignant lesions were common in large intestine. The most common non-neoplastic lesion was appendicitis followed by non-specific inflammation and the most common neoplastic lesion was adenocarcinoma. Peak incidence of adenocarcinomas between 5th to 7th decades. Malignant lesions of small intestine are rare. Tumours of LGIT shows male preponderance M:F ratio of 1.7:1. Early biopsy can help the surgeon to detect many non-neoplastic and neoplastic diseases at early stage. So, proper management can be given to the patients at the earliest.