Recurrent Myxoid Chondrosarcoma of Mandible: A Case Report
Prabha Verma1, Rohini Khurana2, Sambit Swarup Nanda3, Satyajeet Rath4
1 Senior Resident, Department of Radiation Oncology, Dr Ram Manohar Lohia Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
2 Professor, Department of Radiation Oncology, Dr Ram Manohar Lohia Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
3 Assistant Professor, Department of Radiation Oncology, Homi Bhabha Cancer Hospital, Varansi, Uttar Pradesh, India.
4 Senior Resident, Department of Radiation Oncology, Dr Ram Manohar Lohia Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rohini Khurana, Professor, Department of Radiation Oncology, Dr Ram Manohar Lohia Institute of Medical Sciences, Lucknow, Uttar Pradesh-226010, India.
E-mail: drrohinisethi@gmail.com
Myxoid chondrosarcoma is a rare malignant neoplasm of bone or soft tissue origin, characterised by the presence of chondroid and myxoid matrix. These are traditionally radio resistant tumours, so wide surgical resection remains the mainstay of treatment. However, radiotherapy is generally advised for high-grade lesions with poor prognostic factors with adjuvant chemotherapy. The treatment decisions are primarily guided by the histological grade, extent of surgical resection, and site of the neoplasm. A case of a 28-year-old male who presented with recurrent painful swelling in the mandibular region is discussed here. To date, very few cases of Extraskeletal Myxoid Chondrosarcoma (EMC) occurring in the mandible region have been reported. So, due to the paucity of available literature, controversies still exist regarding effective treatment approaches in newly diagnosed and recurrent cases. This case reports the clinical presentation, histopathology, radiological characteristics, immune profile, and treatment modalities used in EMC with a comprehensive and relevant review of the literature.
Bone neoplasm, Ground-glass, Metastasis, Radiation, Sun-burst
Case Report
A 28-year-old male, operated case of myxoid chondrosarcoma of left mandible region, presented to us with chief complaints of pain and rapidly growing swelling at the postoperative site for one month. The patient had a history of surgery performed at a different centre for a similar mass lesion at the same site four months back. Preoperative clinical details suggested a growth extending from upper to lower premolar, gingivo-buccal sulcus reaching up to maxilla, and radiological details suggested moderate-sized irregular lesion arising from left ascending ramus of mandible extending to the condyle. He underwent left hemi-mandibulectomy with ipsilateral supraomohyoid neck dissection. Postoperatively, a gross tumour mass of 5×4.5 cm2 was sent. The histopathological Examination (HPE) suggested a tumour composed of cartilaginous tissue with nodular growth pattern and myxoid rich matrix which is suggested of myxoid chondrosarcoma histology (grade II). The negative resected margins, none of the 22 lymph nodes were positive. No adjuvant treatment was advised by the treating doctor.
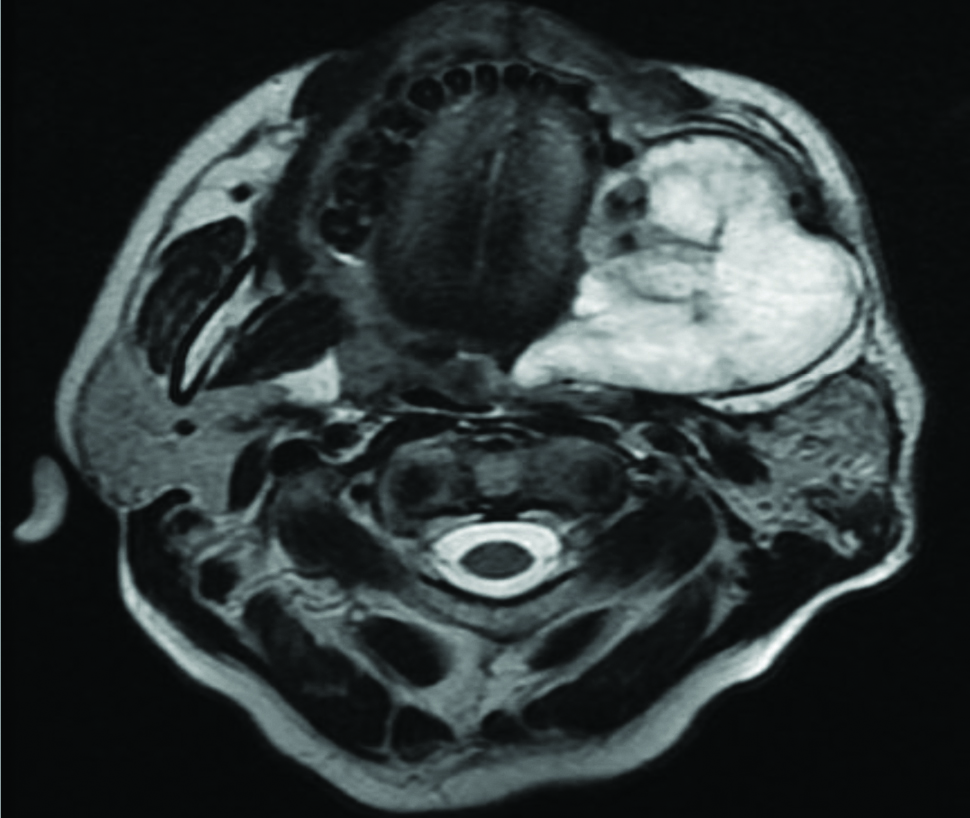
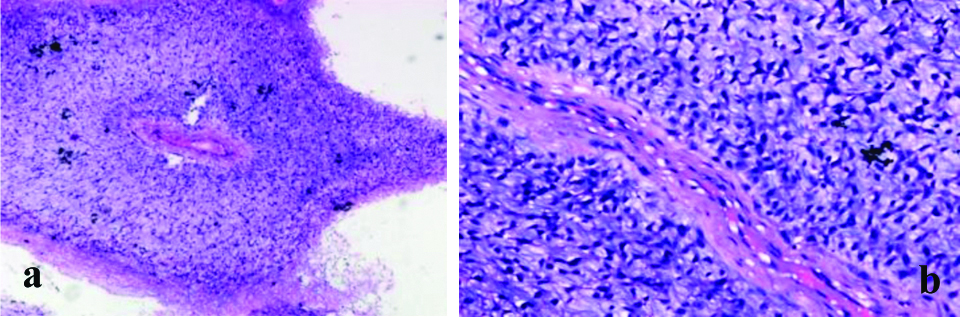
The patient presented in Radiation Oncology Out Patient Department (OPD), four months after first surgery with chief complaints of dull aching localised pain and swelling at the postoperative site. On clinical examination, a 5×5 cm soft to firm, gradually progressive, non-tender, ill-defined swelling along myocutaneous flap extending up to the angle of mandible was detected. The skin overlying the swelling was normal. Intraorally, a same size, non-hyperemic swelling with restricted mobility was detected along the left premolar and molar region. Magnetic Resonance Imaging (MRI) face suggested a 5.7×5.7×6 cm heterogeneous solid cystic lesion in the myocutaneous flap, encircling the cut margin of the mandible [Table/Fig-1]. The provisional diagnosis was a recurrence of myxoid chondrosarcoma and the differential diagnosis was an infection of the mandibular region. For confirmation of diagnosis, an excisional biopsy was done which suggested a myxoid variant of chondrosarcoma suggestive of recurrence. The patient underwent repeat surgery with left buccal mucosa composite resection with removal of myocutaneous flap and reconstruction. Postoperatively on gross examination of the specimen a greyish-white tumour of size 8.5×7.0 cm with irregular surface seen. Histopathologic examination suggested tumour tissue with hyper and hypocellular areas with tumour cells arranged in sheets separated by fibrous bands and disposed of in myxoid stroma suggestive of myxoid chondrosarcoma histology, grade II [Table/Fig-2], with mandibular bone infiltration, 0/2 lymph node metastasis, no Lymphovascular Invasion (LVI) or perineural invasion and free margins. For further confirmation, Immunohistochemistry (IHC) was done, which was positive for vimentin and Ki-67 index of 20% and negative for S-100, CD34, Isocitrate dehydrogenase-1, epithelial membrane antigen, desmin, and cytokeratin.
MRI face axial view showing a large heterogenous well-defined cystic lesion measuring 5.7×5.7×6.0 cm on the left side, anteriorly involving premolar and molar region and posteriorly extending up to retromolar trigone with fluid contents within (at presentation).
HPE: (a) Islands of cartilage are dispersed within sheets of uniform small round cells (Haematoxylin and Eosin staining 10X). (b) Tumour tissue with hyper and hypocellular areas with tumour cells arranged in sheets separated by fibrous bands and are disposed of in myxoid stroma. (H&E stain 40X).
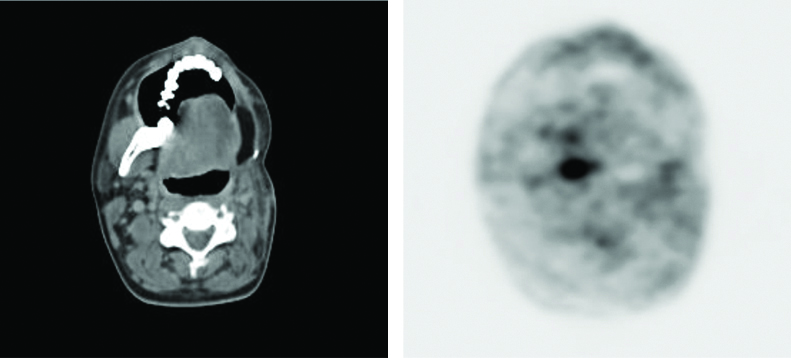
In view of recurrent disease with small recurrence-free interval, large tumour size, and high Ki-67 index, adjuvant radiotherapy to the postoperative tumour bed was planned. The patient received 6000 cGy in 30 fractions radiotherapy at 2 Gy per fraction, five fractions per week for six weeks followed by six cycles of adjuvant ifosfamide and adriamycin-based chemotherapy. Treatment was well-tolerated by the patient, and at three years follow-up there is no evidence of local recurrence or distant metastasis [Table/Fig-3].
PET-CT showing no evidence of FDG avid recurrent/residual lesion in the postoperative bed at three years of follow-up.
Discussion
Chondrosarcoma is a rare primary malignant neoplasm of the head, neck, oral and maxillofacial regions. It is a slow-growing tumour originating from primitive cartilage forming mesenchyme that results in abnormal bone or cartilage growth. These tumours can develop as primary entities or secondary to malignant transformation of benign enchondroma and osteochondroma [1].
The prognosis of chondrosarcoma is associated with the histological grade. Low-grade chondrosarcoma with abundant chondroid matrix and poor cellularity, are localised and show a good prognosis. However, high-grade tumours show more myxoid matrix and high cellularity, easily metastasise, leading to a dismal prognosis [2]. It has skeletal and extraskeletal variants. The skeletal variant typically arises from bones. Extraskeletal variant arises most commonly from soft tissues and is associated with high rates (~40%) of local recurrence, metastasis, and mortality [3].
EMC is a high-grade malignancy and accounts for 2.5% of all soft tissue sarcomas. The most common age group is 50-60 years, with slight male predominance. Approximately, 80% of these cases involve extremities and trunk. Only 5-10% of cases are located in the head and neck region, involving mostly maxilla, nasal septum, cavity, and sphenoid. Its occurrence in the mandible ramus or Temporomandibular Joint (TMJ) is extremely rare [4]. Bindiganavile S et al., demonstrated that there are two factors which can predict the outcome of chondrosarcoma: histological grade and tumour location and the patients with high-grade and axial-location tumours suffered the worst prognosis [5].
In EMC of the mandible region, patient’s symptoms are often misinterpreted as TMJ disorders. HPE and IHC are essential for diagnosis. In IHC cellular proliferation markers Ki-67 and Cyclin B1 are often increased [6]. Radiographic findings include single or multiple radiolucencies with ill-defined borders or ground-glass/sun-burst appearance. Fluorine-18 Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) and MRI are useful for initial staging [7].
Sometimes, EMC may be confused with chondroma but, as chondromas are very rare in the face and jaw so, any cartilaginous tumour arising in this region with an increase in size or pain should be viewed with the suspicion of malignancy [8]. Other differential diagnosis includes myxoid liposarcoma, a myxoid variant of Malignant Fibrous Histiocytoma (MFH), and chondrosarcoma. Myxoid liposarcomas show characteristic lipoblasts with scalloped nuclei against a myxoid background. The myxoid variant of MFH displays marked pleomorphism with histiocyte-like cells. Chondrosarcoma shows a chondroid background and cartilage-like cells embedded within lacunae, rather than chondroblast-like cells lying within myxoid stroma as seen in EMC.
Wide surgical resection is the mainstay of treatment. Neck node metastasis is rare so, neck dissection is not obligatory. Radiotherapy is reserved for high-grade, margin-positive, or recurrent lesions. Gao Z et al., suggested that adjuvant radiotherapy combined with surgery can improve both overall survival and cancer-specific survival of patients with myxoid chondrosarcomas [9]. In EMC role of chemotherapy is debatable but, based on available literature Ifosfamide and Adriamycin based chemotherapy can be considered for recurrent, high-grade lesions with a high proliferative index to decrease loco-regional and distant recurrence.
A five-year recurrence-free survival rates are 40-60 % and in few cases, recurrence may occur even after 10-20 years [3]. Currently, immunotherapies are also being tested for unresectable/metastatic EMC but, the role is still investigational [10].
Conclusion(s)
Individualised treatment after definitive initial surgery and regular follow-up is important. Radiotherapy and chemotherapy seem beneficial in an adjuvant setting for recurrent disease. Poor prognostic factors such as tumour diameter more than 10 cm, early recurrence after surgery, high-grade, high Ki-67 index, and LVI may require aggressive treatment.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Apr 15, 2020
Manual Googling: Mar 02, 2021
iThenticate Software: Mar 22, 2021 (12%)
[1]. Sammartino G, Marenzi G, Howard C, Minimo C, Trosino O, Califano L, Chondrosarcoma of the jaw: A closer look at its managementJournal of Oral and Maxillofacial Surgery 2008 66(11):2349-55.10.1016/j.joms.2006.05.06918940505 [Google Scholar] [CrossRef] [PubMed]
[2]. Chen J, Fong Y, Tang C, Novel strategies for the treatment of chondrosarcomas: Targeting integrinsBioMed Research International 2013 2013:39683910.1155/2013/39683924490159 [Google Scholar] [CrossRef] [PubMed]
[3]. Antonescu C, Argani P, Erlandson R, Healey J, Ladanyi M, Huvos A, Skeletal and extraskeletal myxoid chondrosarcomaCancer 1998 83(8):1504-21.10.1002/(SICI)1097-0142(19981015)83:8<1504::AID-CNCR5>3.0.CO;2-B [Google Scholar] [CrossRef]
[4]. Ramos-Murguialday M, Lasa-Menéndez V, Ignacio Iriarte-Ortabe J, Couce M, Chondrosarcoma of the mandible involving angle, ramus, and condyleJournal of Craniofacial Surgery 2012 23(4):1216-19.10.1097/SCS.0b013e3182565b8022801134 [Google Scholar] [CrossRef] [PubMed]
[5]. Bindiganavile S, Han I, Yun J, Kim H, Long-term outcome of chondrosarcoma: A single institutional experienceCancer Research and Treatment 2015 47(4):897-903.10.4143/crt.2014.13525687868 [Google Scholar] [CrossRef] [PubMed]
[6]. Drilon A, Popat S, Bhuchar G, D’Adamo D, Keohan M, Fisher C, Extraskeletal myxoid chondrosarcomaCancer 2008 113(12):3364-71.10.1002/cncr.2397818951519 [Google Scholar] [CrossRef] [PubMed]
[7]. Platzek I, Beuthien-Baumann B, Schramm G, Maus J, Laniado M, Kotzerke J, FDG PET/MR in initial staging of sarcoma: Initial experience and comparison with conventional imagingClinical Imaging 2017 42:126-32.10.1016/j.clinimag.2016.11.01627951459 [Google Scholar] [CrossRef] [PubMed]
[8]. Shirato T, Onizawa K, Yamagata K, Yusa H, IIjima T, Yoshida H, Chondrosarcoma of the mandibular symphysisOral Oncology Extra 2006 42(6):247-50.10.1016/j.ooe.2006.04.002 [Google Scholar] [CrossRef]
[9]. Gao Z, Lu T, Song H, Gao Z, Ren F, Ouyang P, Prognostic factors and treatment options for patients with high-grade chondrosarcomaMedical Science Monitor 2019 25:8952-67.10.12659/MSM.91795931765367 [Google Scholar] [CrossRef] [PubMed]
[10]. Stacchiotti S, Dagrada G, Morosi C, Negri T, Romanini A, Pilotti S, Extraskeletal myxoid chondrosarcoma: Tumour response to sunitinibClinical Sarcoma Research 2012 2(1):2210.1186/2045-3329-2-2223058004 [Google Scholar] [CrossRef] [PubMed]