Pentasomy X is a rare syndrome with variable phenotype, that affects females with characteristic clinical features such as severe mental retardation with delayed speech, short stature, facial dimorphism, osseous, articular/skeletal/limb abnormalities, and congenital heart defects. Clinical course of the disease seems to be adverse as there has been no evidence of life till adulthood. This case study was of one-month-old girl referred for cytogenetic evaluation that revealed 49,XXXXX karyotype, indicating Pentasomy X syndrome. Studies have mentioned meiotic successive nondisjunction errors in maternal meiosis or combined maternal and paternal origin as a mechanism for Pentasomy X formation which has been supported by genotyping studies using Short Tandem Repeats (STR) X-linked polymorphic markers. An early restricted fetal growth and movements along with increased nuchal fold in pregnancy could suggest referral to prenatal karyotyping studies. Prenatal diagnosis of Pentasomy X syndrome is a challenge due to absence of advanced maternal age and maternal screening markers along with subtle nonspecific Ultrasonography (USG) abnormalities that are detected late in the pregnancy. Hence, there is a strong need of Non Invasive Prenatal Screening (NIPS) with clinical coverage of sex chromosomes in routine pregnancy management along with 3D high resolution USG evaluation as a mandatory workup to rule out Pentasomy X irrespective of advanced maternal age. Management frame work through genetic counseling help patients to adapt to the challenging diagnosis and early interventions for patient management.
Case Report
A case of one-month-old new born female was referred for cytogenetic evaluation from referring Consultant/Paediatrician and Neonatologist, with clinical features of facial dysmorphism, upward slanting palpebral fissure, depressed nasal bridge, deformed pinna and short neck with low hairline. The weight of the baby was 2.045 kg, USG of brain and abdomen were within normal limits. However there was Intrauterine Growth Retardation (IUGR). Detailed antenatal and USG findings were not available as the family belongs to remote location and were with poor socio-economic background.
Ecocardiographic evaluation showed Patent Ductus Arteriosus (PDA) of 2 mm length with a left to right shunt and unregressed Pulmonary Artery Hypertension (PAH). Patent Foramen Ovale (PFO) additional 3 mm fenestration was observed across interatrial septum along with left to right flow and good biventricular systolic function. The baby couldn’t survive and died at a tender age of six months due to adverse clinical manifestations.
The couple had a history of two fetal deaths and absence of advanced maternal age. The third child was normal and five-year-old. The proband was the fourth pregnancy, which was delivered at a tertiary care centre and later expired. However, the causes of first two fetal deaths were not known.
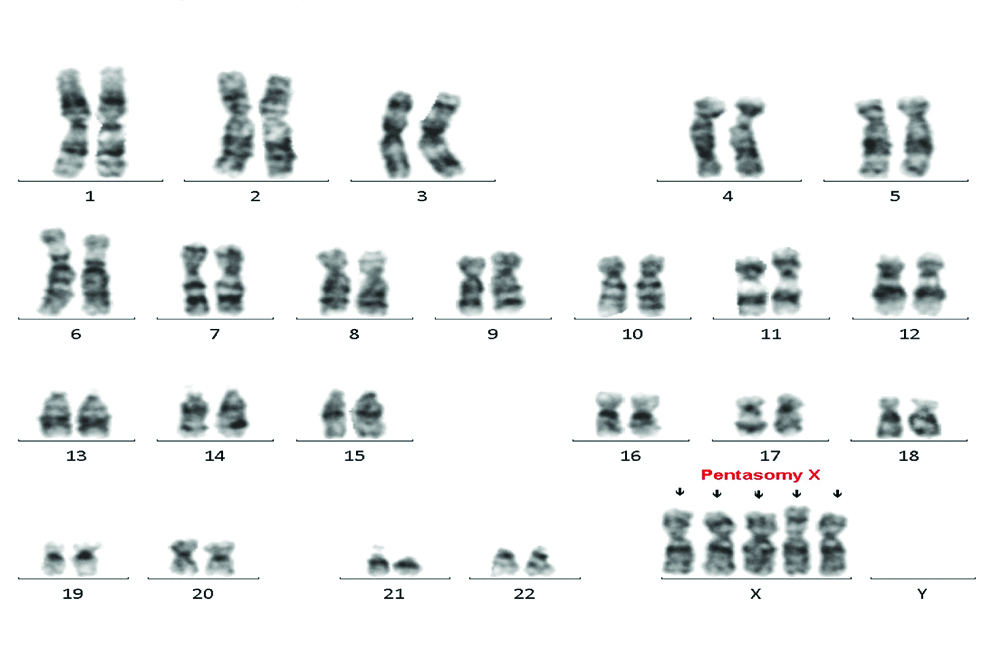
A stimulated peripheral blood culture was set up following standard culture procedure for karyotyping. The cytogenetic evaluation of the Trypsin-Giemsa (GTG) banded slides revealed 49,XXXXX karyotype in all the 20 metaphase cells analysed [Table/Fig-1]. Images were captured using Karyo Imaging Metasystem software (Zeiss), and the karyotype was designated according to International System for Human Cytogenomic Nomenclature (ISCN 2016) nomenclature [1]. Mosaicism was not observed.
Karyotype showing Pentasomy X.
Discussion
Numerical abnormalities of the sex chromosomes such as 45,X, 47,XXX, 47,XXY, and 47,XYY are relatively common, and occur in approximately 1 of 400 live births. Pentasomy X syndrome is a rare sex chromosomal aneuploidy affecting females with variable clinical manifestations. This syndrome is also known as Poly-X or XXXXX syndrome. Present case of Pentasomy X was an addition to the few number of cases reported in the literature till date [2,3].
The true incidence of Pentasomy X is unknown at present due to very few number of cases reported till date [3,4]. The described clinical features in literature for Pentasomy X include severe mental retardation with delayed speech, short stature, facial dimorphism’s, osseous and articular abnormalities, congenital heart defects, and skeletal/limb abnormalities [3]. The first case of this chromosomal abnormality was reported in 1963 [5]. Since then, only few cases have been reported till date, of which, ~26 are postnatal and five are prenatal cases [4].
Other clinical features like microcephaly, micrognathia, plagiocephaly, hypertelorism, upslanting palpebral fissures, flat nasal bridge and malformations of ears are also observed in some cases. Camptodactyly, clinodactyly, radioulnar synostosis, Immunoglobulin anomalies and an increased susceptibility to infection have also been reported in Pentasomy X cases [6].
The pathogenesis of Pentasomy X syndrome has been hypothesised to be due to successive nondisjunction of the meiotic divisions. The phenotypic manifestations can also be dependent on X chromosome inactivation mechanism.
Markholt S et al., determined the parental origin of the extra set of X chromosomes by application of Restriction Fragment Length Analysis (RFLPs) using polymorphic probes M27beta, L1.28 and st14 [4]. Literature studies support the hypothesis of maternal meiotic nondisjunction in meiosis1 and meiosis 2 as a causative mechanism [4]. Study by Cho YG et al., have suggested that meiotic malfunction, either maternal or combined maternal and paternal in origin could lead to formation of Pentasomy X [2]. The most likely mechanism is nondisjunction of the maternal X chromosomes in both divisions of meiosis to produce an XXXX ovum, and this hypothesis has been supported by molecular analysis of X linked polymorphic microsatellite markers [1]. Genotyping and STR-marker analysis by Markholt S et al., hypothesised that the Pentasomy X syndrome can be caused by duplication of both homologue maternal X chromosomes and concluded that successive nondisjunctions in both the 1st and 2nd maternal meiotic divisions is a probable mechanism [4]. There have been various hypothesis put forth concerning the relationship of the X chromosome constitution, the inactivation process and the phenotypic effect [7].
Also, cases with pentasomy X can show phenotypic variations based on the skewed X chromosome inactivation and presence of more than one active X chromosome as possible mechanisms [8].
As a workup, prenatal diagnosis in future pregnancies for couples and parental chromosomal testing is recommended to rule out balanced translocations or polymorphic variations due to heterochomatin increase that can disturb normal gametogenesis. However, in this case, the couple didn’t turn up for parental karyotyping and inheritance pattern could not be ruled out. As the parents were from interior parts of the regions, more detailed investigations were unavailable.
As per literature, patients with Pentasomy X syndrome have facial abnormality, hypertelorism, epicanthus mongoloid slant of palpebral fissures as facial abnormality which is similar to the Down’s syndrome [2]. For accurate diagnosis, cytogenetic analysis is essential, as occasionally patients can be misdiagnosed as having Down’s syndrome due to overlapping syndromic features [1]. Pentasomy X is independent of parental age as observed for other syndromes.
Medical complications that can arise with this syndrome are problems with normal movement owing to musculoskeletal disorders, malfunction of kidneys due to structural abnormalities, malfunction of heart that can lead to endocarditis, arrhythmia, pulmonary hypertension and heart failure [5]. Additionally intellectual deficiency leading to dependency is a major concern.
Challenges during prenatal diagnosis: Prenatal challenges concerned are, absence of typical echographic signs. As USG prenatal abnormalities are detected late in pregnancy and are subtle and nonspecific. Also there is lack of correlation between advanced maternal age and absence of maternal screening markers as a risk factor.
Only five Pentasomy X cases have been reported prenatally in literature and some of the ultrasonographic findings noted include growth restriction, radioulnarsynostosis, dandy-walker malformation, hydrocephaly, ventricular septal defect, hypertelorism, polyhydramnios, increased nuchal translucency, pleural effusion, subcutaneous edema, ascites and bilateral hand clinodactyly [6]. Hence, there is a strong need of NIPS with clinical coverage of sex chromosomes in routine pregnancy management along with 3D high resolution USG evaluation as a mandatory workup to rule out Pentasomy X irrespective of maternal age. The only indications of an early restricted fetal growth and increased nuchal fold in a mother could probably suggest referral to fetal karyotyping and Fluorescence in Situ Hybridisation (FISH) studies [6,7].
In present study, the patient’s ultrasonographic findings apart from showing IUGR there were absence of strong indications for prenatal testing and hence this abnormality was missed as prenatal testing was not done. Detailed obstetric ultrasonographic investigation of proband was unavailable to correlate with present pentasomy X findings.
Studies have shown that fetuses born following Intracytoplasmic Sperm Injection (ICSI) have demonstrated an increased rate of chromosomal abnormalities specifically the sex chromosome aneuploidies predominantly of the paternal origin. Such cases can be detected by first trimester nuchal translucency measurement done as part of routine ultra sound screening and this becomes a mandatory testing in all ICSI pregnancies [9,10].
Prognosis and treatment: Prognosis is generally poor with severity based on the clinical features and complications which can be assessed on a case-by-case basis. Considering lack of complete cure, treatment is mostly given to manage the signs and symptoms with surgical intervention, physical therapy and special education whenever necessary [11].
Conclusion(s)
Counseling for effective communication to understand the disorder, explain the recurrence risk and management of challenges associated would help couples to take early interventions for better care and management of the child. Couples can be supported by involving in associated supportive groups to build up confidence and cope up with the challenges. As there is very minimal recurrence risk of Pentasomy X and is unpredictable due to lack of strong ultrasonographic indications, for future pregnancy management expecting parents and related family members need a mandatory molecular NIPS tool and three-dimensional ultrasound to detect any helpful indicative echographic prognostic signs. Parental karyotyping will be important prior to conception to rule out balanced translocations that may possibly be another cause for bad obstetric history. As the occurrence of this disorder is rare, consideration of prenatal testing should be done as per there commendations by the referring clinician. Overall management framework through genetic counseling will help couples and families to adapt to the challenging diagnosis and plan early interventions for management.
[1]. McGowan-Jordan J, Simons A, Schmid M, ISCN; An International System for Human Cytogenomic Nomenclature 2016 Ottawa, ONKarger Publications [Google Scholar]
[2]. Cho YG, Kim DS, Lee HS, Cho SC, Choi SI, A case of 49,XXXXX in which the extra X chromosomes were maternal in originJ Clin Pathol 2004 57(9):1004-06.10.1136/jcp.2004.01747515333671 [Google Scholar] [CrossRef] [PubMed]
[3]. Kassai RI, Hamada H, Furuta Cho K, Abe K, Deng HX, Penta X Syndrome: A case report with review of the literatureAm J Med Genet 1991 40(1):51-56.10.1002/ajmg.13204001101887850 [Google Scholar] [CrossRef] [PubMed]
[4]. Markholt S, Graakjaer J, Thim SB, Høst B, Skytte AB, A case of penta X syndrome caused by nondisjunction in maternal meiosis 1 and 2Clin Case Rep 2017 5(7):1136-40.10.1002/ccr3.100428680612 [Google Scholar] [CrossRef] [PubMed]
[5]. Kesaree N, Woolley PV, A phenotypic female with 49 chromosomes, presumable XXXXXJ Pediatr 1963 :1099-1103.10.1016/S0022-3476(63)80190-0 [Google Scholar] [CrossRef]
[6]. Pirollo LM, Salehi LB, Sarta S, Cassone M, Capogna MV, Piccione E, A new case of prenatally diagnosed pentasomy X: Review of the literatureCase Rep Obstet Gynecol 2015 2015:93520210.1155/2015/93520225699192 [Google Scholar] [CrossRef] [PubMed]
[7]. Therman E, Denniston C, Sarto GE, Ulber M, X chromosome constitution and the human female phenotypeHuman Genetics 1980 54:133-43.10.1007/BF002789617390488 [Google Scholar] [CrossRef] [PubMed]
[8]. Moraes LM, Cardoso LC, Moura VL, Moreira MA, Menezes AN, Llerena Jr JC, Detailed analysis of X chromosome inactivation in a 49,XXXXX pentasomyMol Cytogenet 2009 2(20):01-13.10.1186/1755-8166-2-2019811657 [Google Scholar] [CrossRef] [PubMed]
[9]. Samli H, Solak M, Imirzalioglu N, Beyatli Y, Simşek S, Kahraman S, Fetal chromosomal analysis of pregnancies following intracytoplasmic sperm injection with amniotic tissue culturePrenatal Diagnosis 2003 23(10):847-50.10.1002/pd.70614558031 [Google Scholar] [CrossRef] [PubMed]
[10]. Cheng PJ, Chueh HY, Shaw SW, Hsu JJ, Hsieh TT, Soong YK, X pentasomy in an intracytoplasmic sperm injection pregnancy detected by nuchal translucency testingFetal Diagn Ther 2008 24(3):299-303.10.1159/00015865318818504 [Google Scholar] [CrossRef] [PubMed]
[11]. Schoubben E, Decaestecker K, Quaegebeur K, Danneels L, Mortier G, Cornette L, Tetrasomy and pentasomy of the X chromosomeEur J Pediatr 2011 170(1):1325-27.10.1007/s00431-011-1491-921590264 [Google Scholar] [CrossRef] [PubMed]