Chest trauma is a major cause of mortality accounting for a substantial proportion of all trauma admissions and death (20-25%) [1]. Both blunt and penetrating trauma can cause disruption of anatomical structures in thoracic cavity and are life threatening unless quickly identified and treated. Blunt trauma accounts for more than 90% of thoracic injuries [2] and road traffic accidents are projected as the commonest cause accounting up to 70% [3]. Blunt chest trauma is commonly caused by sudden deceleration injuries, such as in road traffic accidents or fall from height where deceleration causing the mobile intrathoracic viscera to impact upon the bony structures adjacent to them leading to wide range of injuries. Since blunt chest trauma is associated with significant morbidity and mortality [4], it is crucial for the treating physician to quantify the severity of injury using an appropriate scoring system as it will allow the selection of an appropriate treatment protocol, for predicting intensive care need and ensure the best possible outcome of the patient.
Scales such as Injury Severity Score (ISS) or Trauma Injury Severity Score (TRISS) are widely used, but these being global poly-trauma scales, they underestimated isolated thoracic trauma [5,6]. Scoring systems like Rib fracture score and Pulmonary contusion score are based on isolated anatomy [7,8]. Even though many studies were conducted to assess the validity of various thoracic trauma scales, such studies from South India were limited. Moreover, the association of parameters such as age, mechanism and severity of injury with development of pulmonary complications is still under study.
The aim was to analyse a scoring system with these factors combined, to identify patients with isolated blunt chest trauma at high risk for morbidity and mortality, in order to prioritise intervention, predict and improve the outcome.
Materials and Methods
This was a prospective observational study conducted in the Department of Emergency Medicine and General Surgery of a Tertiary Care Teaching Hospital, in South India over a period of 18 months. The study was initiated after obtaining permission from the Institutional Ethics Committee (IEC reference number: 29/17/IEC/JMMC&RI) and written informed consent was obtained from patient or relatives.
Inclusion and Exclusion criteria: All cases being admitted to the hospital through emergency for blunt chest trauma, either isolated blunt chest trauma or together with associated injuries not requiring surgical intervention or ICU admission in other specialities were included. We excluded patients under the age of 12 years, patients with oesophageal, great vessel and cardiac injuries and with penetrating thoracic injuries.
Sample size: The sample size was estimated using the formula n=z2 (1- ∝ 2) P (1-P)/d2, where, n is the sample size, P is the mortality rate (17.5%), d is the precision (10%), z is the statistic for a level of confidence and z1-α/2=1.96 is the critical value. The sample size according to formula was 56. However, during the study period there were 85 patients of isolated blunt chest trauma who presented to the emergency department and who fulfilled the inclusion criteria. Hence, all 85 patients have been included through consecutive sampling.
The area of chest wall injury including fracture or any other pulmonary or pleural involvement was identified in patients who met the inclusion criteria after thorough clinical evaluation. Demographic parameters, history, vital parameters and necessary investigations were recorded including radiographic images. The scoring system was used at the time of admission and before transferring out from emergency department in order to categorise the patients. The condition of the patient following 48 hours, at the time of discharge and on the 30th day was also recorded.
Scoring criteria: The scoring criteria was adapted from validated thoracic Trauma Severity Score (TTS) developed by Pape H et al., along with few additional criteria like history of smoking and lung disease [9]. In this study, CTS composed of patient factors (age, smoking, and lung disease) and severity of injury (number of fractures, parenchymal involvement, pleural involvement, PaO2/FiO2 ratio) was calculated as given in [Table/Fig-1]. All patients were categorised into low (0-9), medium (10-17) and high risk (18-27) based on the total score. Outcomes were defined as mortality; ICU admission and length of stay; development of complications like pneumonia, Acute Respiratory Distress Syndrome (ARDS), Deep Vein Thrombosis (DVT); and need for interventions like endotracheal intubation, tracheostomy insertion, use of bronchoscopy and lavage, and analgesia requirement. Standard clinical and radiographic criteria were used for diagnosing complications. All the patients were managed as per Airway Breathing Circulation (ABC) protocol on arrival to Emergency Department.
Chest trauma scoring system.
| Score | 0 | 1 | 2 | 3 | 5 |
|---|
| Age (years) | <30 | 30-40 | 41-54 | 55-70 | >70 |
| Smoking | No | Yes | | | |
| Prior lung disease | No | Yes | | | |
| Number of rib fractures | | <3 | 3-5 | >5 | |
| Rib fracture involvement | | U/L | B/L | | |
| Pulmonary contusion | None | U/L 1 lobe | B/L 1 lobeU/L 2 lobes | B/L 2 lobes | B/L >2 lobes |
| Pleural involvement | None | PTX | HTX/HPTXU/L | HTX/HPTXB/L | TPTX |
| PaO2/FiO2 | >400 | 301-400 | 201-300 | 150-200 | <150 |
For calculation of the total score, all categories are summed. A minimum value of 2 points and a maximum value of 27 points can be achieved. Low risk: 0-9; Medium risk: 10-17; High risk: 18-27. U/L: Unilateral; B/L: Bilateral; PTX: Pneumothorax; HTX: Haemothorax; HPTX: Haemopneumothorax; TPTX: Tension pneumothorax
Statistical Analysis
Quantitative data were presented as mean and Standard Deviation (SD) while categorical variables were expressed as frequencies and percentages. To obtain the association of study variables with morbidity Chi-square/Fischer’s-exact test was applied. The efficacy of CTS in predicting morbidity and complications was expressed using Receiver Operator Curve (ROC) curve. To identify the independent predictors of developing morbidity and complications, logistic regression analysis was done. The p-value <0.05 was taken as value of significance. The statistical software namely Statistical Package for the Social Sciences (SPSS) version 20.0 was used for the analysis of the data. Macintosh Operating System (mac OS) pages and numbers (2018 version) were used to enter data and generate graphs, tables and charts.
Results
In present study population, the most common mode of injury was road traffic accident occurring in 83.5% (n=71). Out of 85 patients, 40 (47.1%) were in the 55-70 age group and mean age of study population was 56 years. Majority were males (80%) with a preponderance of 4:1. Among 85 patients, 24.7% (n=21) were smokers and 22.4% (n=19) had previous lung disease.
Rib fractures were seen in all patients with 64.7% (n=55) having ≥5 rib fractures and 57.6% (n=49) with bilateral rib fractures. Few patients had flail chest (11.8%, n=10) and sternal injuries (2.35%, n=2). In 11, out of 12 patients with unilateral pulmonary contusion, involving two lobes and all 31 patients with bilateral pulmonary contusion involving >2 lobes, had developed complications. Sixty one (71.8%) patients had pleural injuries which included pneumothorax (52.5%, n=32), haemothorax (16.4%, n=10), haemopneumothorax (27.9%, n=17) and tension pneumothorax (3.3%, n=2). Of the 61 patients who had pleural injury, 54 (63.5%) required intercostal drainage and underwent tube thoracostomy. PaO2/FiO2 ratio of <150 was observed in 16 (20.3%), 150-200 in 11 (13.9%), 201-300 in 31 (39.2%), 301-400 in 21 (26.6%), >400 in six patients, respectively.
The morbidities associated with chest injuries were ICU admission (57.6%, n=49), endotracheal tube insertion (16.5%, n=14), tracheostomy (3.5%, n=3) and bronchoscopy (17.6%, n=15). Complications on 30 day follow-up were observed in 54 patients (63.5%). Atelectasis was most commonly seen complication (41.2%, n=35) followed by ARDS, pneumonia, surgical emphysema, empyema, DVT and two patients succumbed to the injuries. Parenteral analgesia was required in 21 (24.7%) and need for intervention for analgesia (epidural and para-vertebral block) was required in 27 (31.8%) patients.
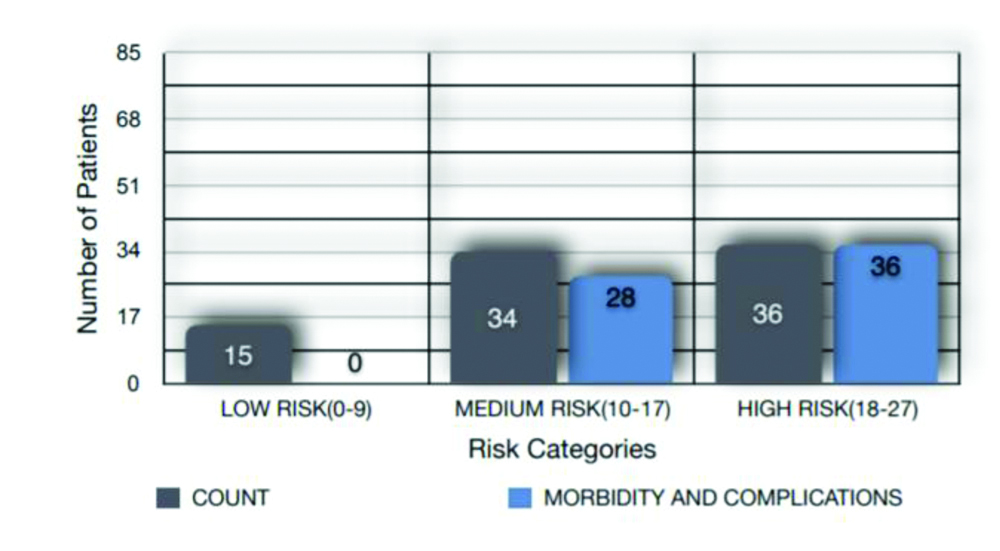
After applying the CTS, 36 (42.4%) were categorised under high risk, 34 (40%) were categorised under medium risk and 15 (17.6%) were categorised under low risk groups. Patients under high risk category had associated morbidity and mortality as seen in two patients with scores of 20 and 22, respectively [Table/Fig-2].
Association with morbidity and complications.
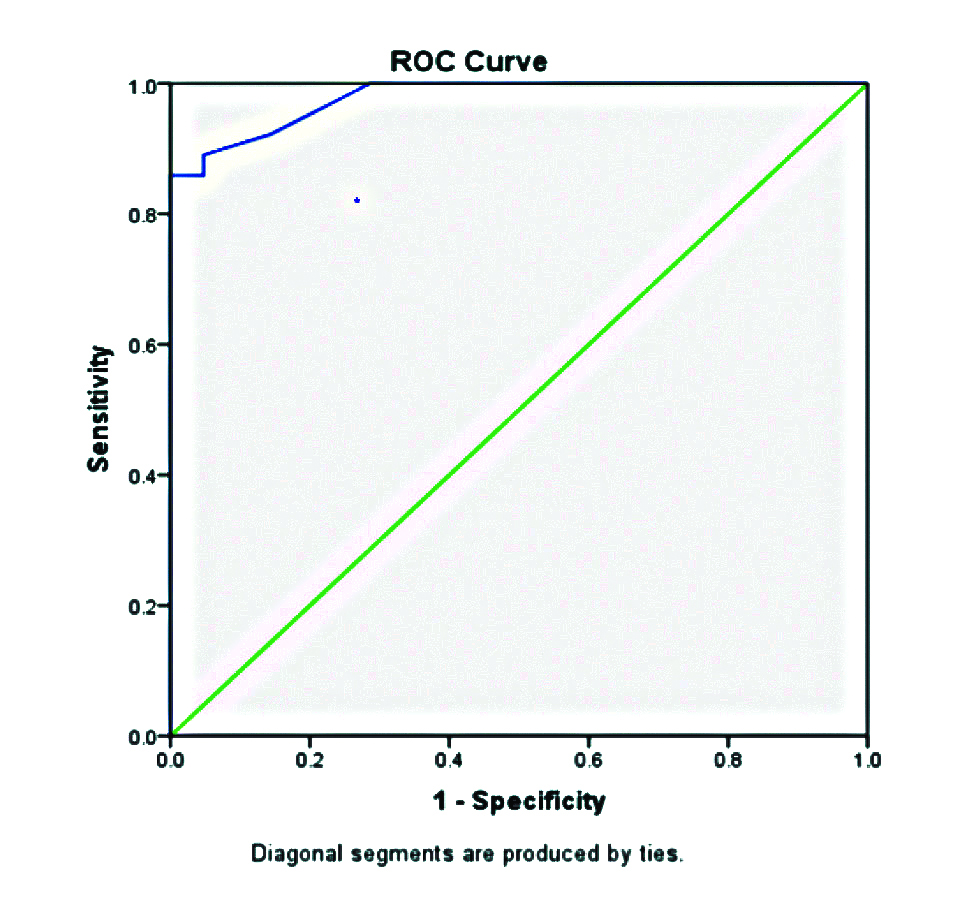
By ROC shown in [Table/Fig-3] (area under curve/AUC-0.979, p-value <0.001), final total score of ≥11.5 was calculated as the most accurate cut-off score value at which the blunt chest wall trauma was considered at risk of developing complications with sensitivity of 89%, specificity of 95%, Positive Predictive Value (PPV) of 98%, Negative Predictive Value (NPV) of 74% and accuracy of 90.6%.
ROC curve for morbidity.
Receiver Operator Curve - AUC: 0.979, p-value <0.001
In patients with CTS ≥11.5, 98.3% had associated morbidity and complications whereas only 25.9% with CTS <11.5 had associated morbidity (p-value <0.001) [Table/Fig-4]. In univariate analysis of complications in patients with CTS of 11.5 or more, atelectasis (p-value=0.001), surgical emphysema (p-value=0.001), pneumonia (p-value=0.001), ARDS (p-value=0.005), empyema (p-value=0.001) and DVT (p-value=0.027) were found to be significant.
Chest Trauma Score (CTS) cut-off value versus morbidity and complications.
| Score | Morbidity and complications | Total (%) | p-value |
|---|
| Present (%) | Absent (%) |
|---|
| <11.5 | 7 (25.9%) | 20 (74.1%) | 27 (3.8%) | <0.001 |
| ≥11.5 | 57 (98.3%) | 1 (1.7%) | 58 (68.2%) |
| Total | 64 (75.3%) | 21 (24.7%) | 85 (100%) |
Chi-square test was used to analyse score with morbidity and complications
p-value <0.001 considered as significant
In univariate analysis to find association of risk factors with morbidity and complications, age (>54), number of rib fractures (>5), bilateral lung involvement, pulmonary contusion score, pleural involvement and PaO2/FiO2 ratio (<200) were found to be significantly associated with morbidity and complications. Number of rib fractures, pulmonary contusion score and PaO2/FiO2 ratio were the significant predictors for morbidity and complications in binary logistic regression model [Table/Fig-5]. The predictive contribution of each variable was quantified by its Z-score. Pulmonary contusion score was found to be the strongest predictor which was followed by PaO2/FiO2 ratio and number of rib fractures.
Analysis of risk factors with morbidity and complications.
| Variables | Odds ratio | CI (95%) | p-value | Z-score |
|---|
| No. of rib fractures: ≥5 | 10.632 | 1.11-102.18 | 0.041 | 2.047 |
| Pulmonary contusion score | 6.007 | 1.93-18.7 | 0.002 | 3.097 |
| Pao2/Fio2 ratio: ≤200 | 12.859 | 1.41-117.13 | 0.023 | 2.266 |
Logistic regression analysis was used to analyse risk factors with morbidity and complications
p-value <0.001 considered as significant
Discussion
The present study analysed the CTS with respect to risk identification and outcome in 85 patients admitted with blunt chest trauma over 30 days follow-up period. Older age group were more affected in this study {55-70 (47%)} compared with studies by Atri M et al., {31-40 (30.8%)} and Lema MK et al., {21-30 (36%)} [10,11]. A univariate analysis showed that patient with age >54 years, 43 (84.3%) had developed morbidity and complications which was found to be statistically significant (p-0.018). Different studies by Battle CE et al., Bulger EM et al., Harde M et al., and Stitzel JD et al., also showed increased association of morbidity and mortality with elderly patients suffering with blunt chest trauma [12-15].
In the present study, road traffic accidents were responsible for blunt chest injury in the majority (83.5%) and second most common mode of injury was fall from height 12 (14.1%). Similar results were observed in study by Dehghan N et al., [16]. Other studies such as those by Narayanan R et al., (59.7%), Lema MK et al., (50.7%), and Liman ST et al., (67.79%) also showed that the road traffic crashes as the leading cause of chest trauma [1,11,17]. History of smoking and previous lung disease were not significantly associated with morbidity whereas study by Battle CE et al., showed chronic lung disease as significant predictor and smoking as insignificant [12].
In present study, among 55 patients with rib fractures ≥5, 53 (96.4%) developed morbidity and complications (p-value <0.001). It was observed that a direct association of increasing number of rib fractures and pulmonary complications exists. Studies by Harde M et al., Unsworth A et al., and Chen J et al., also observed similar correlation between rib fractures and pulmonary complications following blunt chest trauma [14,18,19] The mean score of the patients with pulmonary contusion who developed morbidity and complications was 3.7±1.4 (p-value <0.001). Similarly, the mean score of patients with pleural involvement who developed complications was 2.2±1.1 (p-value <0.001). It was also observed that all those who had a rib fracture of ≥5, had associated pleural injuries. This was consistent with earlier data literature as seen in Cohn SM and DuBose JJ and Al-Koudmani I et al., [20,21], But Harde M et al., observed that development of complications following chest trauma associated with increasing number of rib fractures, high pulmonary contusion and bilateral injury individually but they were statistically not significant [14]. In 53 out of 64 (82.8%) patients with PaO2/FiO2 ≤200, developed morbidity and complications (p-value <0.001), which was similar with the findings in previous studies [22-24].
Of those patients with CTS ≥11.5, the length of stay was significantly longer (7 days), compared to those with score of <11.5. Other studies by Lema MK et al., Liman ST et al., Novakov I et al., and Kasabe PS et al., showed the average duration of hospital stay to be 4.5, 13.7, 8.7 and 8.97, respectively [11,17,25,26]. Among 54 patients having complications, only three had a CTS <11.5 (p-value <0.05). Higher CTS significantly associated with increased need of mechanical ventilation, requirement of intercostal drainage, complications like atelectasis, pneumonia, surgical emphysema, DVT etc. This findings were consistent with studies of Harde M et al., Chen J et al., and Pressley CM et al., [14,19,27]. These studies demonstrated a positive association between high CTS scores and prevalence of mortality also. But in present study, mortality was seen in two patients, both of whom had CTS ≥11.5 which was not significant.
The current medical literature has very few scoring systems that are specific only for chest injuries. The ideal scoring system for chest injuries would be: site specific, valid, reproducible, highly sensitive and specific, encompass both the bony chest injury and the parenchymal lung injury, easy to calculate for clinicians and provide an instant score.
On application of the study score, it was observed that higher CTS significantly attributed to higher risks of morbidity with worsening outcomes. The ROC curve analysis showed that, the CTS ≥11.5 was 89% sensitive and 95% specific for predicting the outcome of thoracic trauma patients. The probability of developing complications for CTS <11.5 was 25.9%. Thus, giving promising results proved the present study scoring system may assist in the prioritisation of patients, proper resource utilisation and earlier implementation of treatment strategies.
Many studies which analyse different scoring systems to assess the prognosis in chest trauma had been published over the years [Table/Fig-6] [12,14,19,22-24,28,29]. Majority of these studies demonstrated that scoring systems which combined both anatomical and physiological parameters emerged as strong outcome predictors [30].
Clinical studies on different scoring criteria to assess the prediction of outcome in chest trauma patients [12,14,19,22-24,28,29].
| Study | Scoring system criteria | Results |
|---|
| Battle CE [12]n=511 | Prognostic model used age, number of RIBFX, chronic lung disease, cardiovascular disease, use of pre-injury anti-coagulants, smoking status, oxygen saturations and respiratory rate on initial assessment in the emergency department | Significant predictors of the development of complications were age, number of RIBFX, chronic lung disease, use of pre-injury anticoagulants and oxygen saturation levels |
| Harde M et al., [14]n=30 | CTS was calculated by scores of age, severity of pulmonary contusion, number of RIBFX and presence of bilateral RIBFX with score ranges from 2-12 | High CTS (≥5) associated with pneumonia, increased requirement of mechanical ventilation and mortality in chest trauma (p-value <0.001)ROC-AUC for mortality shows that the test was acceptable (0.75) and at CTS score 5.5 maximum sensitivity is 87.5% and specificity is 68% |
| Chen J et al., [19]n=1361 | CTS was defined by age, severity of pulmonary contusion, number of RIBFX, and the presence of bilateral RIBFX with a maximum score of 12. | Patients with a CTS ≥5 were older with greater Injury Severity Scores and had a greater prevalence of pneumonia, tracheostomy and mortality (odds ratio 3.99, 95% confidence interval 1.92-8.31, p-0.001) |
| Zahran MR et al., [22] n=284 | TTSS [9] | At a cut-off value of ≥7, TTSS was 100% sensitive and 97.73% specific to poor and fatal prognosis, and was significantly associated with ARDS and need for mechanical ventilation (p-value <0.001; AUC=0.998). |
| Elbaih AH et al., [23]n=30 | TTSS [9] | TTSS with a score of >7 was100% sensitive and 100% specific for prediction of poor outcome (death and ICU admission) with 100% positive predictive value and 100% negative predictive value |
| Sharma AK et al., [24]n=110 | TTSS [9] | TTSS had direct correlation with need for oxygenation, ventilator need, duration of hospital stay, mortality or outcome in chest trauma patients.Significant correlation between TTSS and outcome of patients (p-value=0.0003) demonstrated with maximum mortality for TTSS 16-20. |
| Moon SH et al., [28]n=228 | Comparison of TTSS [9], TRISS [6] | Statistically significant association between the TRISS and in-hospital mortality (p-value <0.001)Association between the TTSS and in-hospital mortality was not statistically significant (p-value=0.547).The ROC curve demonstrated adequate discrimination, as demonstrated by an area under the curve value of 0.787 for the TRISS. At a cut-off value of 25.9%, the TRISS had a sensitivity of 83.6% and specificity of 73.5% to predict in-hospital mortality. |
| Mommsen P et al., [29]n=278 | Comparison of TTSS [9], PCS [8], Wagner score [30] | Among the examined thoracic trauma scores only the TTSS was an independent predictor of mortality.With the TTS showing the best prediction power, the TTS, PCS, and Wagner-score were independent predictors of ventilation time, length of ICU stay, and the development of post-traumatic ARDS and MODS. |
RIBFX: Rib fracture; CTS: Chest trauma score; ROC: Receiver operating characteristic curve; AUC: Area under curve; TTSS: Thoracic trauma severity score; ARDS: Acute respiratory syndrome; ICU: Intensive care unit; TRISS: Trauma injury severity score; PCS: Pulmonary contusion score; MODS: Multi organ dysfunction syndrome; n-sample size
Limitation(s)
Present study had a small sample size and was conducted at a single centre. Significance of other associated injuries in the analysis of results has not been considered as this study was for isolated blunt chest trauma.
Conclusion(s)
Blunt chest trauma patients are often difficult to manage with frequent onset of delayed complications and associated morbidity and mortality. Patient factors like age more than 54 years, number of rib fractures, pulmonary contusion and PaO2/FiO2 ratio were found to be significant predictors of morbidity and mortality in isolated blunt chest trauma. CTS devised in this study, has shown that more is the CTS score (≥11.5) more the chance of occurrence of complications. This makes it a useful prognostic tool to assess the risk and predict the outcomes in isolated blunt thoracic trauma.
For calculation of the total score, all categories are summed. A minimum value of 2 points and a maximum value of 27 points can be achieved. Low risk: 0-9; Medium risk: 10-17; High risk: 18-27. U/L: Unilateral; B/L: Bilateral; PTX: Pneumothorax; HTX: Haemothorax; HPTX: Haemopneumothorax; TPTX: Tension pneumothorax
Chi-square test was used to analyse score with morbidity and complications
p-value <0.001 considered as significant
Logistic regression analysis was used to analyse risk factors with morbidity and complications
p-value <0.001 considered as significant
RIBFX: Rib fracture; CTS: Chest trauma score; ROC: Receiver operating characteristic curve; AUC: Area under curve; TTSS: Thoracic trauma severity score; ARDS: Acute respiratory syndrome; ICU: Intensive care unit; TRISS: Trauma injury severity score; PCS: Pulmonary contusion score; MODS: Multi organ dysfunction syndrome; n-sample size