Introduction
Rickettsial diseases are one of the most covert emerging and remerging zoonosis in India with Scrub typhus being its most common subtype. Its significance lies in its notoriety of being difficult to diagnose early, on when it’s actually easier to treat. The clinicians face multiple dilemmas in diagnosing Rickettsial diseases due to its non-specific signs, diverse presentations and lack of easily available testing facilities at all centers [1]. Clinicians working in non-endemic areas traditionally associate scrub typhus with a classical presentation of fever, rash and a characteristic eschar. The absence of these features leads to a low index of suspicion among treating physicians resulting in under-diagnosis. Three such cases of paediatric scrub typhus with AKI, ARDS and Multi Organ Dysfunction Syndrome (MODS), respectively are described below, each one without any rash or an eschar.
Case Series
Case 1
A 12-year-old female girl was referred with history of fever for six days; cough three days and difficulty in breathing for one day. No history suggestive of tuberculosis or bronchial asthma was there. Neither any visit to farmland or forest was present, though the girl used to play outdoor daily in the local park.
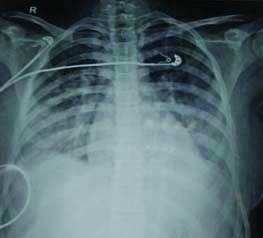
On examination, the child was toxic looking, febrile (102oF) with SpO2 of 84% on admission. Arterial blood gas showed a partial pressure of oxygen (PaO2) of 70 mmHg on 40% inspired oxygen (FiO2). The PaO2/FiO2 ratio (P:F ratio) was 175, suggestive of moderate ARDS. No rash, scar, sinus or eschar was present on the body. Systemic examination showed respiratory distress, nasal flaring and use of accessory muscles of breathing. On palpation, no liver, spleen or lymph nodes were palpable. On auscultation, there were crepitations heard in basal and axillary areas of both lungs. On Cardiovascular System (CVS) examination, the child had tachycardia but no murmur or abnormal heart sounds were heard. Chest radiograph showed bilateral lower and middle lobe pneumonia [Table/Fig-1]. The child had received injection cefotaxime, vancomycin for 3 days before referral. The clinical and laboratory findings are shown in [Table/Fig-2].
Chest radiograph (Case 1) showing bilateral pneumonia.
Clinical and Laboratory features of the three patients (at admission).
| Variables | Case 1 | Case 2 | Case 3 |
|---|
| Clinical findings |
| Age (in years) | 12 years | 3 years | 2 years |
| Gender | Female | Female | Male |
| Place of residence | Urban | Rural | Rural |
| Duration of fever | +; 6 days | +; 7 days | +; 7 days |
| Bodyaches | + | - | - |
| Lymphadenopathy | - | - | - |
| Hepatosplenomegaly | - | + | - |
| Respiratory distress | + | - | + |
| Acute Kidney Injury (AKI) | - | + | - |
| Rash | - | - | - |
| Eschar | - | - | - |
| Defervescence of fever | 2 days | 3 days | 4 days |
| Outcome | Recovered | Recovered | Recovered |
| Laboratory findings |
| SGOT (IU/L) | 28 | 36 | 176 |
| SGPT (IU/L) | 34 | 42 | 52 |
| Serum Creatinine (mg/dL) | 0.6 | 2.1 | 0.8 |
| Platelet count (per mm3) | 1.1 lac | 80,000 | 95,000 |
| Bilirubin (mg/dL) | 0.6 | 0.8 | 5.0 |
| Widal | -ve | -ve | -ve |
| MP | -ve | -ve | -ve |
| Dengue NS1 Ag test and ELISA | -ve | -ve | -ve |
| COVID-19 RT-PCR | -ve | -ve | -ve |
| Urine culture | Sterile | Sterile | Sterile |
| Blood culture | Sterile | Sterile | Sterile |
| CSF culture | Sterile | Sterile | Sterile |
| IgM ELISA for scrub typhus | ++ | ++ | ++ |
SGOT: Serum glutamic oxaloacetic transaminase; SGPT: Serum glutamic pyruvic transaminase; MP: Malarial parasite; NS1 Ag: Non-structural protein 1 antigen; ELISA: Enzyme-linked immunosorbent assay; COVID-19: Coronavirus disease-2019; RT-PCR: Reverse transcription polymerase chain reaction; CSF: Cerebrospinal fluid; IgM: Immunoglobulin M
She was stabilised with non-invasive ventilation (Continuous Positive Airway Pressure (CPAP) at a Positive End Expiratory Pressure (PEEP) of 6-7 cm H2O), fluids and other supportive treatment. Keeping a clinical diagnosis of Pneumonia with ARDS. Common differential diagnoses considered as possible underlying causes (sepsis, bacterial/viral pneumonia, enteric, COVID-19 etc.,) were investigated as per resource availability [Table/Fig-2]. Antibiotics were upgraded to meropenem and vancomycin but no response was elicited. In view of a history of acute febrile illness, pneumonia and thrombocytopenia which showed no response to broad spectrum antibiotics, possibility of diagnosis of scrub typhus pneumonia with ARDS was considered.
Oral doxycycline (100 mg BD) was thereby started and Enzyme Linked Immune-Sorbent Assay (ELISA) for scrub typhus IgM was sent which came out positive confirming clinical suspicion. The child showed defervescence of fever within 48 hours of starting doxycycline and respiratory distress also settled down. Doxycycline was stopped after seven days and the child discharged after 10 days. On follow-up, the child was afebrile and doing well.
Case 2
A three-year-old female child presented with high grade fever for seven days, generalised oedema for five days and decreased urine output since two days. No history of any medical/renal disease was present in the child or family. Family had a rural background and parents were agricultural workers.
On admission, the child was febrile (103oF) and generalised oedema on the face and whole body was observed. Abdominal examination showed hepatosplenomegaly (liver 4 cm, spleen 3 cm below costal margin) and free fluid in abdomen on ultrasound. On auscultation, CVS and respiratory system was normal. Keeping in mind the clinical picture of acute febrile illness with hepatosplenomegaly, anasarca and oliguria (depicting AKI), various infective aetiologies like sepsis, severe malaria, dengue, complicated enteric fever, hepatitis and Human Immunodeficiency Virus (HIV) were considered as initial differential diagnoses. Relevant investigations were done which ruled these out [Table/Fig-2].
Urine examination showed proteinuria below nephrotic range, occasional Red Blood Cells (RBCs) and a sterile urine culture. Work up for Nephrotic syndrome and Post-streptococcal glomerulonephritis (C3 complement levels, ASO titers, 24 hour urine protein were also normal was also normal). Lab results showed increased urea, creatinine levels and thrombocytopenia. Injection ceftriaxone was started empirically at admission but no response was observed even after 48 hours. In view of clinical picture of acute febrile illness with AKI and thrombocytopenia with investigations ruling out the common differential diagnosis [Table/Fig-2], likelihood of scrub typhus complicated by AKI was considered. IgM ELISA for scrub typhus was sent and doxycycline was started. Within 48-72 hours of starting doxycycline, fever spikes settled and child became afebrile after three days. IgM ELISA for scrub typhus also came positive confirming the clinical diagnoses. Urinary output improved gradually and the child was discharged after 10 days. On follow-up, the child was asymptomatic and doing well.
Case 3
The third case was a two-year-old male child referred with high grade fever for seven days, generalised oedema, respiratory distress and shock (multi-organ failure). The child had received broad spectrum antibiotics like ceftriaxone, vancomycin for three days before referral.
On admission, the child had fever, breathing difficulty, shock and splenomegaly. Investigations including complete haemogram showed leukocytosis with thrombocytopenia (normal platelet morphology) with no atypical cells. Liver function tests were deranged [Table/Fig-2]. Considering clinical scenario that included acute pyrexia with multisystem involvement, common differential diagnoses of septic shock, severe malaria, dengue fever, complicated enteric fever, HIV were considered initially and work-up sent. The child was managed initially with fluid bolus, inotropes, Continuous Positive Airway Pressure (CPAP) and broad-spectrum antibiotics (meropenem, vancomycin, fluconazole) and antimalarials. In view of investigations, ruling out the above first line differentials and child also showing no clinical response after 48 hours, as shown in [Table/Fig-2], possibility of scrub typhus complicated with multi-organ dysfunction and shock was suspected.
Doxycycline was thereby started empirically and IgM ELISA for scrub typhus was sent which was positive. Child improved with fever showing defervescence within four days of starting doxycycline. The child had complete recovery after seven days of admission and was discharged. On follow-up, he was afebrile and doing well.
Discussion
Paediatric scrub typhus is a zoonotic infection caused by Orientia tsutsugamushi and transmitted via bite of larval mite (chiggers) of the Trombiculidae family [2]. Only, the larval stages transmit the disease and there is no human-to-human transmission. Rodents are the mammalian reservoirs and humans are the accidental host [3]. Scrub typhus can occur in areas with scrub vegetation of low-lying trees, bushes, in river banks, rice fields, farming areas, lawns, parks, poorly maintained kitchen gardens which are inhabited by rodents and chiggers [4].
Rickettsial diseases are considered to be one of the most covert emerging and re-emerging diseases in India. It is now the most common reported rickettsial infection in India [5-7]. However, it is still being underdiagnosed in children especially in plain areas. The three cases reported in the series belonged to the plains with no travel history to hills.
The characteristic early clinical profile of paediatric scrub typhus in children includes high grade fever, myalgia, bodyaches, rash, generalised lymphadenopathy and an eschar [8]. Acute onset fever of undifferentiated origin is the most common presenting feature in children and is commonly associated with myalgia and headache [8]. In a study of 180 children, with acute febrile illness, where common causes of fever were excluded, 24% of children were diagnosed as rickettsial diseases with scrub typhus being the most common [9].
Among dermatological features, a pink macular rash (sparing the palms and soles), spreading centrifugally and later becoming maculo-papular, petechial or haemorrhagic is considered as the hallmark of scrub typhus [8]. However, the presence of rash is not universal in scrub typhus patients. Rathi B et al., while describing a clinical scoring system for rickettsial diseases in central India, documented skin rash in only 23 % (10/43) children diagnosed with scrub typhus while Narvenear KP et al., found rash to be present in 53% (8/15) adults with scrub typhus [10,11]. This absence of either a rash or an eschar in the reported cases could possibly be explained on the basis of variation in cutaneous immunity in scrub typhus and its rarity among south-east Asian and Indian subcontinent population [11,12].
Similarly, an eschar, a crusty necrotic lesion with or without surrounding halo is considered pathognomonic of rickettsial diseases [12]. It is a painless, necrotic, 1 cm diametric lesion resembling the skin burn of a cigarette butt with underlying lymphadenopathy. Despite a diligent search, none of the three children reported were found to have any eschar or rash on physical examination. In the study by Rose W et al., which described the distribution of eschar in paediatric scrub typhus patients, an eschar was found to be present in only 40.8% (176/401) patients [13]. Also, an eschar is not specific to scrub typhus and can be seen in diseases such as anthrax, bacterial ecthyma and rat bite fever [14]. This explains why in the above three cases, the primary physician missed the diagnosis of scrub typhus before referral. The low index of suspicion could also be due to the absence of skin manifestations and low incidence of paediatric scrub in North Indian plains [15].
Apart from the varied early clinical features, a wide-ranging group of systemic manifestations and complications are attributed to scrub typhus. These include neurological, gastrointestinal, respiratory and renal features. Emphasis must be given to the fact that these systemic features can also be the initial presentations paediatric scrub typhus [14]. The three-year-old girl (case 2) who presented with AKI brings to light an often unnoticed and under diagnosed cause of tropical community acquired AKI. This, in part, was due to the referring physician not suspecting paediatric scrub typhus in the absence of a rash and eschar, plus the paucity of literature documenting AKI in paediatric scrub typhus patients [16,17]. This is because renal injury in children is often postulated to be a consequence of MODS secondary to sepsis [2]. However, in scrub typhus, AKI is believed to be mainly caused by impaired renal perfusion due to volume depletion or increased vascular permeability accompanied with systemic vasculitis, leading to vascular endothelial damage. This hypothesis was postulated by Dumler JS et al., in their study evaluating the clinical and laboratory features in 80 children with scrub typhus in southern Texas, USA [18]. It was further corroborated by a study from Allen AC and Spitz S, who compared the organ wise pathology of scrub typhus with other rickettsial diseases. They found intra-capillary form of acute diffuse Glomerulonephritis in 30% (19/64) of scrub typhus cases. The mechanism of renal injury was damage to glomerular capillaries endothelium shown by swelling, hyperplasia and karyorrhexis of endothelial cells and glomerular venules. There was moderate to severe ischemia of glomerular capillaries found universally in patients with Glomerulonephritis [19].
Pulmonary manifestations of scrub typhus had been variably reported in adults as cough or pneumonia at one end to fatal ARDS in extreme cases. ARDS, MODS and AKI are complications of scrub typhus which usually occur during the second week of illness leading to a delay in the initiation of appropriate treatment [20]. These complications are postulated to be due to endothelial injury leading to increased vascular permeability and capillary leak, oedema, hypovolemia and ischemia. This was corroborated in studies by Narvenear KP et al., in their study on 15 scrub typhus patients wherein around 46% (7/15) cases had evidence of capillary leak syndrome, oedema and shock in them [11]. However, the three children reported had a shorter incubation period and had severe complications within first week of illness only, which is also uncommon.
An early diagnosis based on clinical features supported by relevant investigations holds the key towards a good outcome in paediatric scrub typhus. Immunofluoresence Assays (IFA) are considered gold standards but the cost and technical expertise is prohibitive. Therefore, it is usually reserved for research purposes. IgM ELISA is perhaps the most sensitive test available for scrub typhus and its sensitivity matches that of IFA [14,15]. In all the index cases, IgM ELISA was positive for scrub typhus and clinical outcome supported the serological diagnosis. Doxycycline is the drug of choice for treating Rickettsial diseases in children and found safe in all paediatric age groups [14]. Response to doxycycline is dramatic and remission of fever usually occurs within 48-72 hours. Alternate drugs used are azithromycin, clarithromycin or chloramphenicol. All the three cases reported responded well to doxycycline with a successful outcome.
Conclusion(s)
The authors conclude by emphasising that scrub typhus is often an under-diagnosed disease among Indian children. This is especially true in non-endemic areas like plains of north India where few adult cases had been reported. Although, careful examination for an eschar or rash is an important clue guiding the diagnosis of scrub typhus, but the disease should never be excluded solely on the basis of their absence, especially when it’s timely treatment with a low cost drug doxycycline can lead to successful outcomes.
[1]. Rathi N, Rickettsial diseases in India- A long way aheadPediatric Infect Dis 2015 7:61-63.10.1016/j.pid.2016.01.004 [Google Scholar] [CrossRef]
[2]. Raoult D, Scrub typhus. In Mandell GL, Bennet JE, Daolin R, edsPrinciples and practice of infectious diseases 2005 6th edPhiladelphiaElsevier Churchill Livingstone:2309-10. [Google Scholar]
[3]. Rahi M, Gupte MD, Bhargava A, Verghese GM, Arora R, DHR-ICMR Guidelines for diagnosis and management of Rickettsial diseases in IndiaIndian J Med R 2015 141(4):417-22.10.4103/0971-5916.15927926112842 [Google Scholar] [CrossRef] [PubMed]
[4]. Mittal V, Gupta N, Bhattacharya D, Kumar K, Ichhpujani RL, Singh S, Serological evidence of Rickettsial infections in DelhiInd J Med Res 2012 135(4):538-41. [Google Scholar]
[5]. Mahajan SK, Rolain JM, Sankhyan N, Kaushal RK, Raoult D, Pediatric scrub typhus in Indian HimalayasIndian J Pediatr 2008 75(9):947-49.10.1007/s12098-008-0198-z [Google Scholar] [CrossRef]
[6]. Kumar K, Saxena VK, Thomas TG, Lal S, Outbreak investigation of scrub typhus in Himachal Pradesh (India)J Commun Dis 2004 36(4):277-83. [Google Scholar]
[7]. Bhat NK, Dhar M, Mittal G, Shirazi N, Rawat A, Kalra BP, Scrub typhus in children at a tertiary care hospital in North IndiaIran J Pediatr 2014 24(4):387-92. [Google Scholar]
[8]. Rathi N, Rathi A, Rickettsial infections: Indian perspectiveIndian Pediatr 2010 47(2):157-64.10.1007/s13312-010-0024-320228429 [Google Scholar] [CrossRef] [PubMed]
[9]. Somashekhar HR, Prabhakar DM, Sreeja P, Elizabeth M, Didier R, Jean MR, Magnitude and features of scrub typhus and spotted fever in children in IndiaJ Trop Pediatr 2006 52(3):228-29.10.1093/tropej/fmi09616291832 [Google Scholar] [CrossRef] [PubMed]
[10]. Rathi B, Rathi A, goodman MH, Aghai ZH, Rickettsial diseases in central India: Proposed clinical scoring system for early detection of spotted feverIndian Pediatr 2011 48(11):867-72.10.1007/s13312-011-0141-721555807 [Google Scholar] [CrossRef] [PubMed]
[11]. Narvenear KP, Rodrigues S, Nevrekar RP, Dias L, Dias A, Vaz M, Scrub typhus in patients reporting with acute febrile illness at a tertiary health care institution in GoaIndian J Med Res 2012 136(6):1020-24. [Google Scholar]
[12]. Mahajan SK, Rolain JM, Kashyap R, Bakshi D, Sharma V, Prasher BS, Scrub typhus in HimalayasEmerg Infect Dis 2006 12(10):1590-92.10.3201/eid1210.05169717176580 [Google Scholar] [CrossRef] [PubMed]
[13]. Rose W, Rajan JR, Punnen A, Ghosh U, Distribution of eschar in pediatric scrub typhusJ Trop Pediatr 2016 62(5):415-20.10.1093/tropej/fmw02727122479 [Google Scholar] [CrossRef] [PubMed]
[14]. Rathi N, Kulkarni A, Yewale V, IAP guidelines on rickettsial diseases in childrenIndian Pediatr 2017 54:223-29.10.1007/s13312-017-1035-028361787 [Google Scholar] [CrossRef] [PubMed]
[15]. Chaudhry D, Garg A, Singh I, Tandon C, Saini R, Rickettsial diseases in Haryana: Not an uncommon entityJ Assoc Physicians India 2009 57(4):334-37. [Google Scholar]
[16]. Kumar V, Kumar V, Yadav AK, Iyengar S, Bhalla A, Sharma N, Scrub typhus is an under recognized cause of Acute febrile illness with acute kidney injury in IndiaPLOS Negl Trop Dis 2014 8(1):e260510.1371/journal.pntd.000260524498445 [Google Scholar] [CrossRef] [PubMed]
[17]. Yen TH, Chang CT, Lin JL, Jiang JR, Lee KF, Scrub typhus: A frequently overlooked cause of acute renal failureRen Fail 2003 25(3):397-410.10.1081/JDI-12002115212803503 [Google Scholar] [CrossRef] [PubMed]
[18]. Dumler JS, Taylor JP, Walker DH, Clinical and laboratory features of murine typhus in south Texas, 1980 through 1987JAMA 1991 266(10):1365-70.10.1001/jama.1991.034701000570331880866 [Google Scholar] [CrossRef] [PubMed]
[19]. Allen AC, Spitz S, A comparative study of the pathology of scrub typhus (Tsutsugamushi Disease) and other rickettsial diseasesAm J Pathol 1945 21(4):603-81. [Google Scholar]
[20]. Wang CC, Liu SF, Liu JW, Chung YH, Su MC, Lin MC, Acute respiratory distress syndrome in scrub typhusAm J Trop Med Hyg 2007 76(6):1148-52.10.4269/ajtmh.2007.76.114817556627 [Google Scholar] [CrossRef] [PubMed]