Diminished Bone Marrow Oedema and Healing of Insufficiency Fractures in a HIV Patient after Switching Antiviral Therapies
Sebastian Radmer1, Julian Ramin Andresen2, Reimer Andresen3
1 MD, Department of Orthopaedics, Centre for Orthopaedics, Berlin, Germany.
2 BSc (Med), Department of Medical School, Sigmund Freud University, Vienna, Austria.
3 MD, PhD, Department of Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westkuestenklinikum Heide, Academic Teaching Hospital of the Universities of Kiel, Luebeck and Hambu, Heide, Schleswig-Holstein, Germany.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Sebastian Radmer, Bozener Str. 17, Berlin, Germany.
E-mail: sebastian@dr-radmer.de
This is a case report about the recurrent onset of bone marrow oedemas and insufficiency fractures in a 64-year-old male Human Immunodeficiency Virus (HIV)-patient, who was going through an antiviral treatment. The patient experienced stress-related pain and swelling in both ankle joints and feet, and was treated antivirally with Atripla® for several years. Therapeutically, conservative treatment as well as a therapeutic trial with bisphosphonates were performed. As a result of developing renal insufficiency, antiviral therapy was switched to a combination of Prezista® and Norvir®. Only after switching the antiviral therapy, there was a clear clinical improvement of the symptoms. The clinical symptoms correlated well with Magnetic Resonance Imaging (MRI), the features of which are detectable regressive bone marrow oedemas and the healing of insufficiency fractures. The impaired renal function improved to a compensated retention. In the case of HIV patients with unclear joint complaints, the presence of bone marrow oedema should be considered.
Bone marrow oedema syndrome, Fatigue fracture, Human immunodeficiency virus, Medical therapy, Renal insufficiency, Tenofovir
Case Report
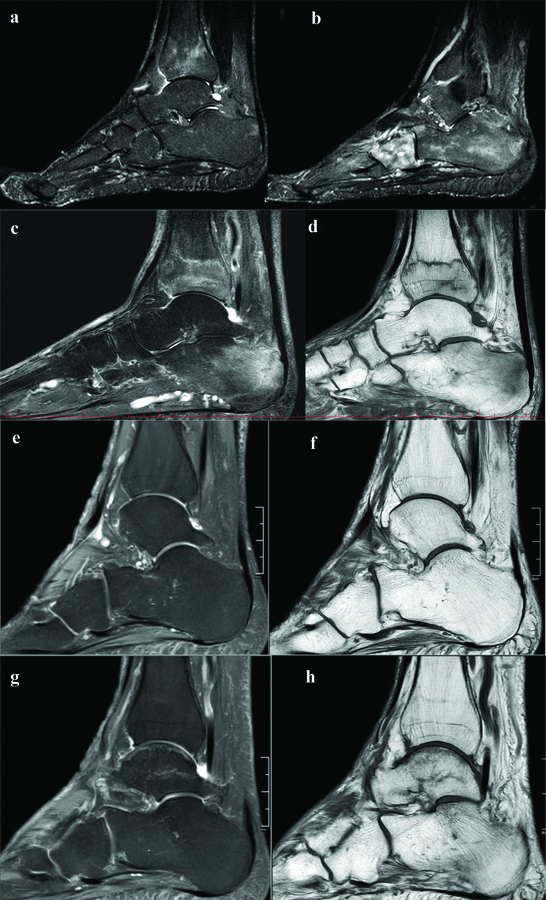
A 64-year-old HIV patient reported in the practice for orthopaedics about recurrent stress related pain and swelling in both ankle joints and feet since five years. The patient was treated with antiviral therapy from Atripla® (Efavirenz, Emtricitabine, Tenofovir) for several years with an undetectable viral load. Trauma to the lower extremities was denied. Except for the HIV-positive status, the patient suffered from no chronic or endocrinological diseases. The blood analysis showed: Leukocytes 4.2 G/l, Erythrocytes 4.72 T/l, Haemoglobin 13.9 g/dL, Haematocrit (HKT) 43.1%, Mean Cell Hemoglobin (MCH) 29.4 pg, Mean Corpuscular Hemoglobin Concentration (MCHC) 32.3 g/dL, Mean Corpuscular Volume (MCV) 91.3 fL, Red Cell Distribution Width (RDW) 14.6%, Thrombocytes 220 G/l, Vit. D 49,6 ng/mL, Testosterone 6.32 ng/mL, Parathyroid Hormone (PTH) 3.22 pmol/L, Sodium (Na) 143 mmol/L, Calcium 2.39 mmol/L and inorganic phosphate 1.13 mmol/l. The vital parameters were in normal limits. The T-score in the bone mineral density measurement by Dual-energy X-ray Absorptiometry (DXA) was 1.5 for the lumbar spine and 1.2 for the right hip. The clinical examination showed doughy skin of the swollen ankles and distinct pressure pain. Walking caused the patient severe ankle pain Visual Analogue Scale 8 (VAS 8). Initially, conventional X-ray in two planes and Magnetic Resonance Imaging (MRI) of both ankle joints were acquired. The conventional images showed no fractures or detectable degenerative changes, nor local reduction of bone mineral content. Initial MRI showed bone marrow oedema in both feet especially in several tarsalia and metatarsalia [Table/Fig-1a-d].
In T2-weighted images of the left foot in the sagittal view a diffuse bone marrow edema can clearly be visualised in the distal tibia, the cuboid and the calcaneum (a,b).
The T2-weighted image of the right foot (c) demonstrates a severe bone marrow oedema in the distal tibia and in the calcaneum. In the T1-weighted image (d) the fracture lines in the distal tibia and in the calcaneum are well depicted. After switching of the antiviral therapy to Prezista®, the bone marrow oedema dissolved almost completely in the left foot (e and f). In the right foot (g and h), there are some residual left
Therapeutically, conservative treatment with dynamic load reduction, physiotherapy, lymphatic drainage, systemic application of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) as well as a therapeutic trial with bisphosphonates (alendronic acid 70 mg/week for 6 months) were performed.
Regular clinical and chemical examinations as well as follow-up MRI were performed. The antiresorptive therapy over six months had no effect on pain severity and manifestation of bone marrow oedema. The conservative treatment showed slight temporary reduction of the symptoms. But the patient suffered from recurring pain exacerbation going along with bone marrow oedema in both feet. In the further course, oedema occurred also in both calcanei and the distal tibial meta- and epiphysis. The patient suffered from insufficiency fractures in both calcanei [Table/Fig-1e-h]. The progressive bone marrow oedemas were accompanied by normal bone specific blood parameters, but there was a significant increase in creatinine and decrease in glomerular filtration rate. As a result of a developing renal insufficiency (stage 3), antiviral therapy was switched to a combination of Prezista® (Darunavir) and Norvir® (Ritanovir).
After switching the anti-viral therapy, the patient showed a clear clinical improvement with pain reduction and improving renal function. The development of the clinical symptoms correlated with the MRI-detectable regressive bone marrow oedemas and the healing of the insufficiency fractures. After 18 months of the therapy adjustment the patient was pain free, and there were no signal alterations in the bone marrow of the left foot and only discrete residual alterations in the right foot on MRI scans. The insufficiency fractures were completely consolidated. The impaired renal function improved to a compensated retention (stage 2). The patient was still free of viral load.
Discussion
Severe pain, swelling and impaired function of one or more joints without a traumatic event could be the symptoms of Bone Marrow Oedema Syndrome (BMES). Typical locations are the joint adjacent areas of bones of the lower extremities and vertebrae. The syndrome most commonly occurs in middle-aged men and young women, with an incidence of 3 to 1 in men and women [1]. The diagnosis is made by MRI which shows a typical pattern of changes in signal intensities with diffuse decrease in T1w images and diffuse increase in strongly T2w fat suppressed images [2].
Causes for BMES can be mechanical, metabolic, ischemic, inflammatory, degenerative or infiltrative neoplasm. BMES can occur as a solitary entity and it can be accompanied by loss of bone mineral density in the affected areas (transient osteoporosis). In addition to the general risk factors for the pathological reduction of bone mineral density like abuse of alcohol and nicotine, the use of opiates and glucocorticoids, inactivity, low body weight and vitamine D deficiency, HIV positive patients are exposed to specific risk factors. Chronic inflammation can cause imbalance to the bone formation system through the stimulating effects of proinflammatory cytokines such as IL-6 or Tumor Necrosis Factor (TNF)α on bone resorption. Proteins of the Human Immunodeficiency Virus (HIV) itself might be responsible for the activation of osteoclasts and the inhibition of osteoblast acitivity. Antiretroviral therapy has been associated with bone loss. The extent of the effect on bone loss varies between different antiretroviral class substances. Tenofovir is known to cause nephrotoxicity in the proximal tubule leading to hypophosphatemia, a strong stimulus for production of Parathyroid Hormone (PTH) which activates bone resorption. Reduced renal function might lead to a decrease in the 1-α-hydroxylation of 25-hydroxyvitamin D, a precursor of active vitamin D [3]. Therefore, in HIV positive patients with joint pain, the existence of BMES should be considered [4].
The etiology of BMES is not completely understood. Usually BMESs are, in contrast to osteonecrosis, self-limiting and heal spontaneously under conservative therapy within 3-10 months [5]. A positive effect of bisphosophonates has been shown [6]. There are also drugs which may potentially result in bone marrow oedema [7].
In present case, the patient suffered from recurring BMES and insufficiency fractures that did not respond to conservative therapy or administration of bisphosphonates. A possible reason could be the Tenofovir induced renal dysfunction and the dysregulation of the bone metabolism with increased phosphate elimination and increased bone resorption [8].
Conclusion(s)
In the case of HIV patients with unclear joint complaints, the presence of bone marrow oedema should be considered. In the present case, the BMES could originate by an increased phosphate excretion by the potentially nephrotoxic Tenofovir. In case of increasing renal impairment, medications containing Tenofovir should be replaced with alternative antiviral agents.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 07, 2020
Manual Googling: Jan 03, 2021
iThenticate Software: Jan 23, 2021 (15%)
[1]. Starr AM, Wessely MA, Albastaki U, Pierre-Jerome C, Kettner NW, Bone marrow edema: Pathophysiology, differential diagnosis, and imagingActa Radiol 2008 49(7):771-86.10.1080/0284185080216102318608031 [Google Scholar] [CrossRef] [PubMed]
[2]. Hayes CW, Conway WF, Daniel WW, MR imaging of bone marrow edema pattern: transient osteoporosis, transient bone marrow edema syndrome, or osteonecrosisRadiographics 1993 13(5):1001-11.10.1148/radiographics.13.5.82105868210586 [Google Scholar] [CrossRef] [PubMed]
[3]. Castronuovo D, Cacopardo B, Pinzone MR, Di Rosa M, Martelotta F, Schioppa O, Bone disease in the setting of HIV infection: Update and review of the literatureEur Rev Med Pharmacol Sci 2013 17(18):2413-19. [Google Scholar]
[4]. Vera JH, Walker AE, Kinderlerer A, Cooke GS, Transient bone marrow oedema syndrome in an HIV-infected patient on highly active antiretroviral therapyInt J STD AIDS 2012 23(3):213-15.10.1258/ijsa.2009.00935822581878 [Google Scholar] [CrossRef] [PubMed]
[5]. Wilson AJ, Murphy WA, Hardy DC, Totty WG, Transient osteoporosis: Transient bone marrow edema?Radiology 1988 167(3):757-60.10.1148/radiology.167.3.33631363363136 [Google Scholar] [CrossRef] [PubMed]
[6]. Bartl C, Imhoff A, Bartl R, Treatment of bone marrow edema syndrome with intravenous ibandronateArch Orthop Trauma Surg 2012 132(12):1781-88.10.1007/s00402-012-1617-123053191 [Google Scholar] [CrossRef] [PubMed]
[7]. Triplett J, Vijayan S, Prince R, Kermode A, Dimethyl fumarate-associated transient bone marrow oedema syndromeMult Scler 2019 25(6):876-79.10.1177/135245851879113230051766 [Google Scholar] [CrossRef] [PubMed]
[8]. Parsonage MJ, Wilkins EG, Snowden N, Issa BG, Savage MW, The development of hypophosphataemic osteomalacia with myopathy in two patients with HIV infection receiving tenofovir therapyHIV Med 2005 6(5):341-46.10.1111/j.1468-1293.2005.00318.x16156882 [Google Scholar] [CrossRef] [PubMed]