Introduction
Each year approximately, 15 million preterm babies are born worldwide and India has the highest number of preterm births. In 2010, it was estimated that 3,519,100 babies were born preterm in India. Due to advances in neonatal care, the survival rate of these preterm babies are increasing but unfortunately all babies born preterm are vulnerable for serious health problems [1]. ROP is a potentially blinding vasoproliferative disorder of the retina occurring predominantly in premature infants [2]. It is an emerging cause of childhood blindness and can have enormous impact on the quality of life of affected infants [3]. This is a preventable disease with a wide spectrum, either regress spontaneously or progress to severe retinal detachment leading to irreversible blindness [4]. Nearly 50,000 infants become blind from ROP each year globally. There are approximately 1.26 million blind children worldwide and among these 2,80,000 children are from India. ‘Vision 2020: The Right to Sight’ is a global initiative launched by World Health Organisation and International Agency for the Prevention of Blindness (IAPB) to eliminate avoidable blindness by the year 2020 and prevention of blindness in children is given a high priority in this program [5].
Retinopathy of Prematurity, previously known as retrolental fibroplasia, was first recognised in 1942 by Dr. Theodore L Terry. Visual impairment from ROP has been described in three ‘epidemics’. The first epidemic of ROP occurred due to unrestricted use of oxygen. The second epidemic was reported in high income countries because of increased survival rate of very preterm babies [6]. ROP was reported in India over a decade ago and at present; India is facing the “third epidemic” of ROP with an incidence between 38-51.9% in low birth weight infants which varies considerably in different states of the country. This is because of many reasons, the major being the increased survival rate of preterm infants, inadequate and suboptimal care provided in NICUs and low coverage of services for screening and treatment for ROP [7,8].
Neonatal nurses are the pillars of NICU. Their knowledge and clinical expertise for standard practices are essential for preventing ROP related visual impairment. Nurses spent more time with the inpatient preterm babies and are expected to provide developmentally supportive care, monitor desired oxygen targets, ensure aseptic practices in NICU, meet the nutritional needs of these babies with special focus on breast feeding, keep a record of daily weight, plan and prepare the babies for screening and assist the ophthalmologist in screening procedure. In addition, they maintain a good rapport with the parents and provide the necessary information and support to the parents.
Classification of ROP
International Classification of ROP (ICROP) was published in 1984 to standardise terminologies used to describe ROP [9]. It was later revised in 2005. This classification is based on the following criteria:
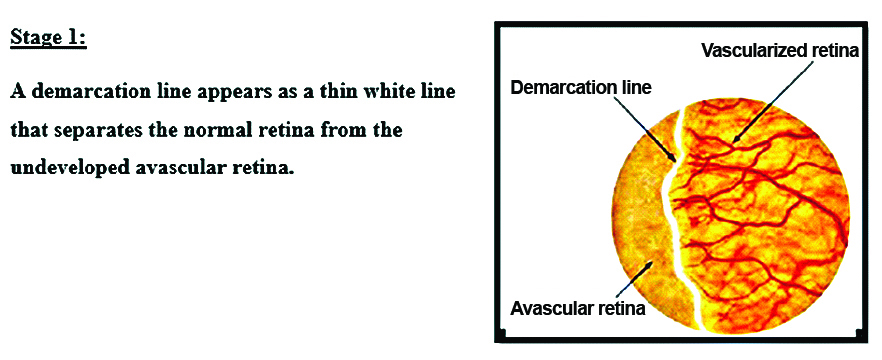
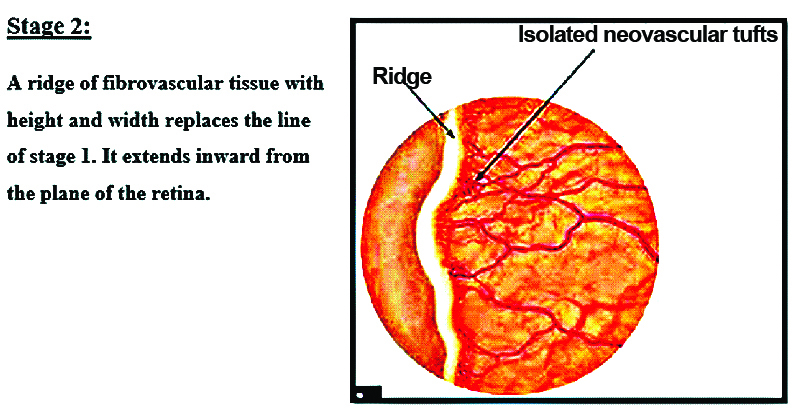
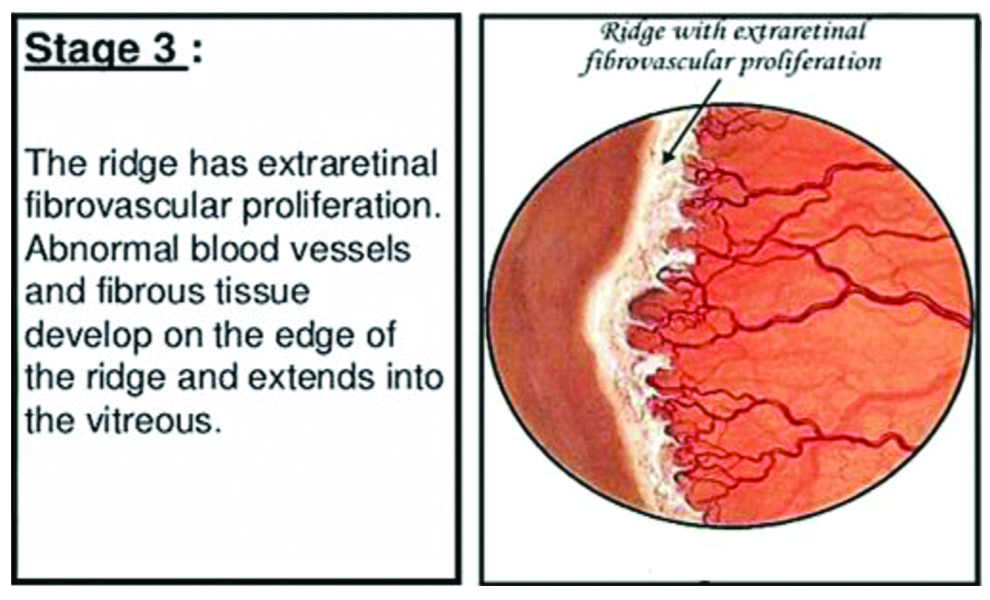
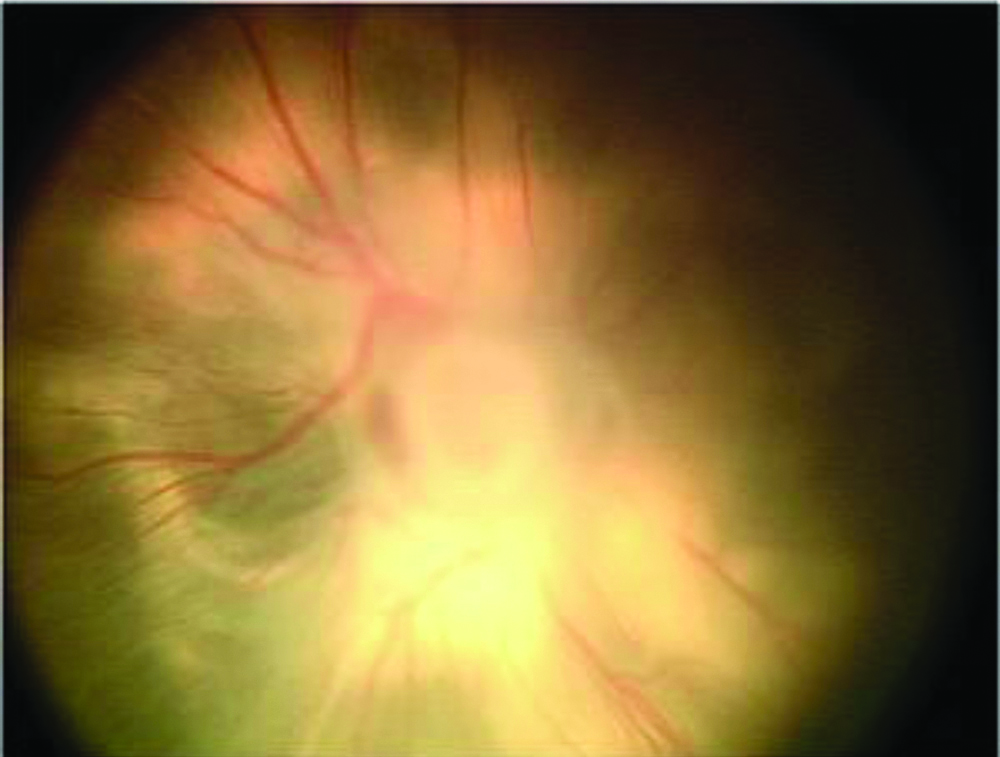
The severity or stages of ROP [Table/Fig-1,2,3,4 and 5]
The location or zone of the disease
Extent of the disease
Presence or absence of plus disease
Presence or absence of aggressive posterior ROP [9]
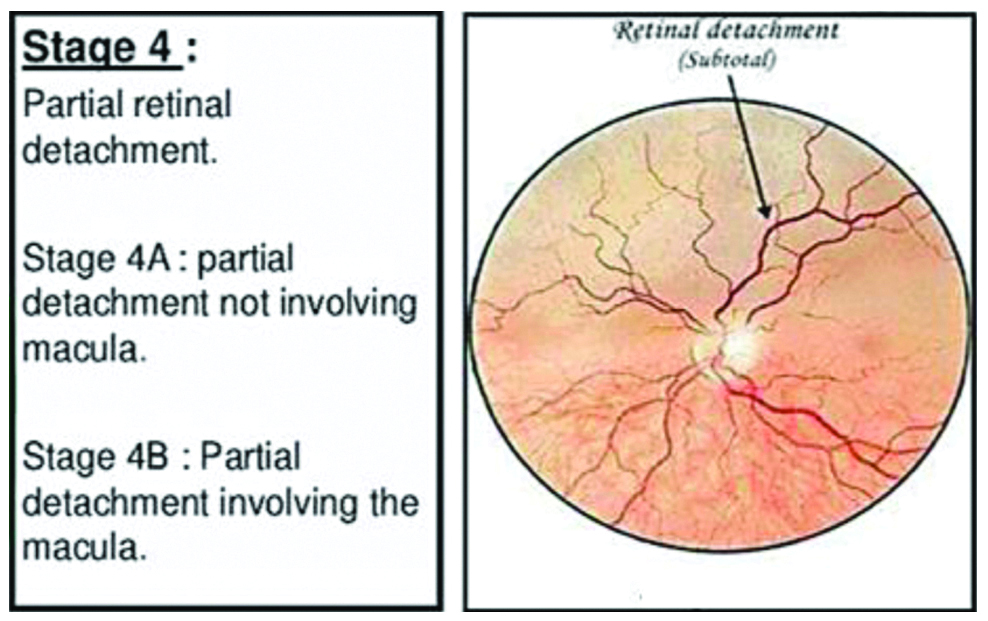
Stage 5- Total retinal detachment.
1. The Severity or Stages of ROP
2. Location of Disease
The development of normal blood vessels in retina is from the optic nerve posteriorly to ora serrata anteriorly [Table/Fig-6] [9].
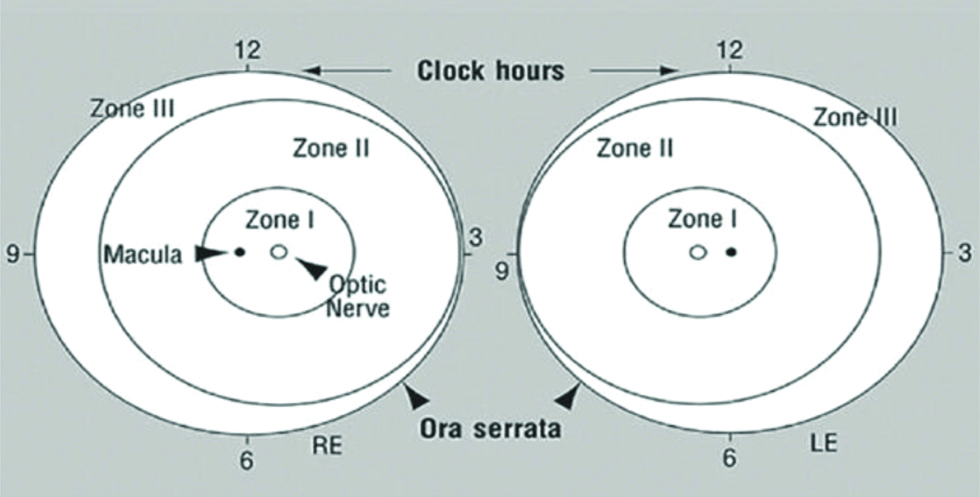
Zone I: A small circle with a radius of twice the distance from the macula to the centre of optic disc.
Zone II: Area of retina surrounding zone I, with a radius of distance from centre of optic disc to the nasal margin of retina.
Zone III: Area of retina from zone II to ora serrata on nasal side and equator on temporal side [10].
3. Extent of Disease
The retina is divided into 12 sectors similar to a clock and the number of clock hours of the eye’s circumference involved is defined as the extent of ROP [11].
4. Presence or Absence of Plus Disease
Plus disease: It is characterised by dilatation and tortuosity of retinal arterioles and venules near the optic disc [11].
5. Presence or Absence of Aggressive Posterior ROP
Aggressive posterior ROP: This is a rare, but rapidly progressing, severe form of ROP. It was previously referred to as “rush disease”. This type of ROP is posteriorly located, with prominent plus disease and nearly always in Zone II. AP-ROP should be recognised and treated within 48 hours as it can progress rapidly to retinal detachment [11,12].
As per the revised ICROP classification (2005):
Prethreshold ROP
Type 1: Zone I with any Stage with plus disease, Zone I with Stage 3 without plus disease, and Zone II with Stage 2 or 3 with plus disease.
Type 2: Zone I with Stage 1 or 2 without plus disease, Zone II with Stage 3 without plus disease [12].
Threshold ROP: This is defined as Zone I or Zone II with Stage 3+ROP extending for five contiguous sectors or eight composite sectors [11,12].
Prevention and Management of ROP
Prevention of blindness related to ROP needs a multidisciplinary team approach. The team consists of obstetricians, neonatologists, ophthalmologists, nurses, paediatricians, health care workers and parents [12]. In addition to prematurity and low birth weight, many studies report other risk factors for development of this disease such as oxygen therapy, mechanical ventilation, sepsis, respiratory distress, blood transfusion, poor weight gain and anaemia [1,13]. Preterm babies are not born with ROP, but develop this during the course of their NICU stay. So, everybody involved in the care of these newborn babies should work collaboratively to reduce the risk of blindness from ROP.
Nurses Perspectives
Neonatal nurses are the back bone of the NICUs. ROP is considered as an indicator of the quality of neonatal inpatient care especially nursing care. Nurses with specialist knowledge and skills are essential in providing best practices for prevention of ROP [14]. They act as primary caregivers, practice rationale uses of oxygen, pulse oximetry and immediate management of apnoeic episodes, support for adequate weight gain. Nurses act as clinical advocate by protecting them from unnecessary interventions and pain. They are the team co-ordinators in NICU. Nurse leaders are involved in planning and implementation of appropriate protocols and mentoring junior staff in prevention of ROP. They provide necessary information to the family throughout the continuum of care. As a member of comprehensive child services team, nurses are involved in all the three levels of prevention of this potentially blinding disorder. Nurses working in community can also contribute significantly [15]. Nurses counsel the mothers at risk of preterm delivery to deliver in well-equipped facilities. It is also the nurses’ responsibility to prepare the infants for screening and assist the ophthalmologist during the eye examination. Nurses also counsel the parents regarding the importance of attending the appointments after discharge.
Nurses Role in Primary Prevention
Primary prevention of ROP includes strategies to reduce the rate of premature birth by improving quality of obstetric and neonatal care. India is a developing country and majority of people live in rural areas. They have minimum access and availability of optimum health care facilities. Community health workers especially nurse and Accredited Social Health Activist (ASHA) workers play an important role in providing cost-effective interventions for a healthy pregnancy and a better neonatal outcome.
A significant proportion of preterm babies (who are born between >20 and <37 weeks of gestation) experience lifelong disabilities and health issues [16]. Nurses working in hospitals as well as in community can take initiative in following:
Creating public awareness to prevent preterm births by controlling biological, clinical and socio-behavioural risk factors in women of child bearing age. Education should focus on:
Measures to avoid teenage pregnancies.
Maintain adequate pre pregnancy body weight.
Iron and Folic acid supplementation.
Control and proper management of chronic diseases.
Cessation of harmful health habits e.g., smoking, alcoholism, substance abuse.
Judicious use of infertility treatment.
Improve mental health.
Proper screening and management of high risk pregnancies.
Special care in pregnancies with bad obstetrical histories e.g., Cervical encirclage, use of vaginal progesterone.
Use of antenatal steroid in women with preterm labour before 34 weeks and also in cases of premature rupture of membrane under 32 weeks gestation.
Care of preterm delivery- Care during “Golden Hour” to maximise survival and minimise morbidity
Prevention of hypothermia in labour room.
Avoid initial 100% oxygen administration and preferable use of nasal Continuous Positive Airway Pressure (CPAP) rather than mechanical or manual ventilation [17].
Safe and standard practices in NICU which can be summarised as POINTS of care. (P-pain control, O-judicious use of Oxygen, I-infection control measures, N-adequate nutrition, T-thermoregulation, S-supportive care) [18]-
Pain increases the babies need for oxygen and worsen respiratory distress. It makes the babies unstable. Avoid unnecessary painful procedures, anticipate pain and take pain relieving measures such as oral glucose/sucrose or swaddling during procedures.
Oxygen supplementation. Ensure that oxygen saturation is between 89-94% and set alarms accordingly. Use of blenders and CPAP are preferable.
Practice infection control measures strictly. Neonatal infections, especially fungal infections, are also risk factors for ROP. Frequent hand washing and following aseptic techniques are important responsibilities of nurses. Being the co-ordinator of neonatal care in NICU, the nurse incharge should ensure that the team members are practising standard precautions for prevention of infections.
Provide adequate nutrition and monitor weight gain. Use breast milk as far as possible but supplement extra calories and proteins. Recent studies reported that post-natal weight gain predicts the risk of ROP.
Thermoregulation. Prevention of hypothermia is of utmost importance and Kangaroo Mother Care can be promoted to keep the baby warm, to increase maternal breast milk production as well as to improve child parent bonding. Use a plastic bag or occlusive wrapping to prevent heat loss.
Supportive developmental care for normal neuromuscular development. Reduce the stress of preterm babies as this can lead to fluctuations in oxygen saturation. Minimise bright lights and sounds in NICU. Position babies comfortably with their limbs supported. Swaddling, minimal handling of the babies and clustering of nursing procedures are recommended as these will provide adequate periods of uninterrupted sleep.
Avoid blood transfusions as far as possible.
Prevention of anaemia. Delayed cord clamping is advised. In premature new-borns, anaemia is often exacerbated by withdrawing too much blood for laboratory tests too often.
Standard neonatal care practices, good infrastructure and availability of resources also need attention. Pulse oximeters, oxygen blenders and CPAP units should be available in sufficient number [19].
Nurses Role in Secondary Prevention
Secondary prevention includes screening and treatment of ROP. This disease is asymptomatic in its early course and starts only two three weeks after birth thus providing adequate time for early detection and treatment [20].
Screening Guidelines
Screening guidelines vary from region to region. The 2019 ROP screening guidelines published by the American Academy of Paediatrics and American Academy of Ophthalmology (AAP/AAO) recommend screening of all infants with gestational age of less than or equal to 30 weeks and/or birth weight ≤1500 g, or with unstable clinical course as per the treating neonatologist’s suggestion [21].
In India, it is seen that more mature and heavier babies also develop sight threatening ROP due to the variation in quality of neonatal care across the country. So, the guidelines were revised and now it is recommended to screen all babies with gestational age ≤34 weeks and those with >34 weeks with risk factors if the gestational age is known, or all infants ≤2000 g birth weight if gestational age is unknown [22,23]. To avoid confusions about the timing of first screening Jalali S et al., recommend “day 30 day 20” strategy i.e., first ROP screening should be done strictly before “day 30” of post-natal life and by “day 20” of life in smaller babies (<30 weeks and/or birth weight <1200 g). Better compliance is seen with this day 30 day 20 strategy as it is easy to remember the date of birth of these babies by all health care providers [24]. Screening is performed by an expert using indirect ophthalmoscopy.
Role of Nurses in ROP Screening
Record weight and gestational age at birth.
Monitor weight gain during NICU admission.
Select babies eligible for screening.
Counsel the parents regarding screening procedure.
Dilate eyes one hour before examination using a topical agent.
Keep the baby nil per oral one hour prior to procedure.
Position the baby comfortably, take adequate pain control measures.
Ensure hand washing, use sterile articles only during procedure.
Monitor vital signs.
Documentation of procedure, fix next appointment.
Treatment
ROP can advance rapidly and any delay in treatment will reduce the chances of success. So, it should be considered as a medical emergency and treatment is warranted within 48 hours of diagnosis in severe form and as soon as possible in APROP. Cryotherapy was the initial treatment modality, but less frequently used now-a-day. Currently, laser photocoagulation is the treatment of choice because of more precision and less unfavourable side-effects [25]. Adequate and timely laser treatment has a success rate of around 90%. In case of severe ROP and those who do not respond to laser photocoagulation, anti-Vascular Endothelial Growth Factor (anti-VEGF) is also used. But it is not used as first line therapy. There are controversies regarding long term complications of this treatment on eye as well as the possibility of developing systemic complications like developmental delay [8,26]. Use of propranolol, treatment with Insulin like Growth Factor-1 (IGF-1), vitamin E and gene therapy are also under investigation for the treatment of this disease. Surgical interventions such as scleral buckling, lens sparing vitrectomy, lensectomy with vitrectomy or open sky vitrectomy may be needed to treat stage 4 and 5 of ROP and these procedures are performed only by paediatric retinal surgeons [2].
Nurses Role in Counselling of Parents
Frequent eye examinations may be needed during the NICU stay and parents should be informed regarding the importance of performing screening procedure. ROP screening may require multiple visits even after discharge from NICU. Non-compliance and failure to follow-up regularly are the most common challenges in ROP screening. Parents need to be made aware of the disease process and the importance of frequent follow-up so that adverse events can be prevented. Rapid progression of disease and need for early intervention such as laser therapy should be communicated to parents [27]. Nurses in NICU can play a major role in counselling the parents as they have frequent interaction with them. Ophthalmologists should reassure the parents that laser treatment will not cause any harm to their child. Community health nurses in rural area can also play a pivotal role in counselling the parents during their home visits. Public awareness should be raised through print and electronic media and by placing hoardings by celebrities regarding ROP [16].
Barriers for Early Identification and Management of ROP
ROP is emerging as a major public health problem and a developing country like India has many hurdles to overcome for the effective implementation of screening and treatment strategies. Of course, the escalation and standardisation of neonatal care have led to better survival of preterm babies, but availability of ROP screening and treatment is not in pace with that which in turn lead to increased visual morbidity due to ROP [28]. A recent study conducted in India reports that non-availability of trained personnel, ignorance of parents and health care personnel, distance of point of care are some of the factors for delay in seeking proper care [29].
a. Lack of resources
Lack of resources in terms of man, money and materials exist in our country. Inadequate infrastructure in many of the neonatal care units also add to the problem. Scarcity exists in availability of equipments and supplies such as pulse oximeters, CPAP units and air oxygen blenders for maintaining the proper oxygen saturation. Disposable and sterile items should be adequately available for individualised infant care to prevent infection. Indirect ophthalmoscope for screening and laser machines for treatment of ROP should be readily available. Indian ROP Society reports that there are only <200 specialists who are skilled in ROP screening nationwide which act as a major hindrance for timely identification of cases [30]. In service education of the care providers in NICUs by conducting regular education programs, workshops and training is essential to bridge the gap. Maintain the recommended nurse patient ratio and skill mix in NICU so that individual attention can be made while caring these high risk babies.
b. Lack of awareness among medical professionals including nurses
Recent studies report that awareness among paediatricians about ROP is poor and babies are referred to ophthalmologists for ROP screening too late when they notice a white reflex or the parent’s complaint of the same. By the time the baby may be irreversibly blind [31-33]. Capacity building by conducting regular medical education programs, training and workshops on ROP screening and management for ophthalmologists, neonatologists and paediatricians may help to enhance the knowledge and skill. It is desired to establish a better rapport between them; for which proper communication is also mandatory [34]. A recent study conducted in Kerala reported that majority of the neonatal nurses working in a tertiary care setting were having moderate level of knowledge regarding ROP, but were unable to interpret the screening results documented by the ophthalmologist [35].
Nurses should be educated regarding the modifiable risk factors and the need for standard practises in NICU to reduce the visual morbidity. Experienced nurses with skill in handling neonates should be posted in NICU. ROP should be given due importance in the curriculum of doctors and nurses in all levels. In case of non-availability of trained ophthalmologists, telescreening is another option and recent studies have show that nurses and other non-physicians can be trained successfully in telescreening and can be utilised in areas where trained ophthalmologists are not available [36].
c. Lack of communication and co-ordination.
Unfortunately, a communication gap exists between the care providers in neonatal care units. Ophthalmologists, neonatologists, paediatricians and neonatal nurses should work as a team for better clinical outcome of preterm infants. Nurses should take the initiative in planning and conducting screening examinations as per suggestions of neonatologists/ophthalmologists in NICU and ensure that all eligible babies are screened on time. Parents should be made aware of the need for screening, compliance with follow-up and treatment. Usually parents are confident with the neonatologists as well as the nurses because they have frequent interaction with them [14].
Role of Nurse in Tertiary Prevention
ROP requires repeated consultations even after discharge from hospital. Parents should be adequately convinced regarding this before they leave NICU. Nurses should make sure that these children are attending the Ophthalmology Department regularly and undergoing necessary examinations. Community health nurses may also be involved by making home visits and reinforcing the need for continuation of treatment. Long-term visual rehabilitation is the key to achieve optimal visual outcomes. Tertiary prevention includes treating complications to prevent visual disabilities or improve visual function by correction of refractive errors. Many of these children need to wear spectacles from early childhood and repeated counselling of parents may be necessary [37]. Lack of screening is the most common reason for stage 5 ROP in India. If all preterm babies at risk are screened on time, stage 4 or 5 ROP can be prevented from occurring which will reduce the chance for visual disabilities. Sometimes, even after laser treatment disease progresses to stage 4 or 5. Resolution of treated ROP may end up with vision impairing ocular morbidities such as refractive errors especially high myopia, strabismus, amblyopia, cataract, glaucoma and cortical visual impairment [38]. It may become necessary to have long term follow-up by paediatric ophthalmologists regarding which, parents need to be informed [39]. Good vision from early infancy is essential for normal child development as vision co-ordinate other sensory inputs and helps the child to understand his environment and develop psychomotor and cognitive functions. Visual rehabilitation of the affected children is also important. They need to be helped to achieve physical, social, emotional and spiritual independence and optimum quality of life. Blind children should receive special education and trained for leading a productive life. Parental and social support is of utmost important in bringing up these children. Rehabilitation services of these children should be integrated into the health system to ensure the continuity of care [40].
Scope of Nurses
International standards for neonatal care should be established globally to foster better survival and neonatal outcomes. There is a potential for developing a cadre of specialist ROP nurses, but unfortunately there are very few formal training programs for neonatal nurses in our country. Competency based training should be conducted emphasising the role of nurses in prevention and management of ROP. Accreditation for neonatal nurses as a specialist will provide opportunities for career development and better understanding of multiple dimensions of their roles. For making a sustainable change, leadership from within the nursing profession should come up and experienced neonatal nurses can mentor the junior staff to improve quality of care in NICU [14]. Nurses can be trained for ROP screening and there are research findings which showed nurses are capable to perform ROP screening as it is carried out by an expert paediatric ophthalmologist [41,42]. This can be practised in tertiary care settings as a specialised area for developing nursing leadership in prevention of ROP. Nurses in community also can be prepared for telescreening and may be utilised for bridging the gap whenever experts are not available especially in rural areas.
Conclusion(s)
It is very difficult to predict or control premature birth, but high quality obstetric and neonatal care, timely screening and treatment of ROP can reduce the number of infants becoming blind or visually impaired. Realising its importance, ROP is included in newborn screening program under Rashtriya Bal Swasthya Karyakram (RBSK) by the Government of India. Competency-based training of medical professionals including neonatologists, paediatricians, ophthalmologists and nurses should be conducted regularly. Nurses, being the cot side caregivers in NICU are responsible for providing standard practices for optimal neuro-developmental outcomes of preterm infants. They act as advocates by protecting these babies from unnecessary exposure to risk factors during the NICU admission. Creating awareness regarding ROP among the public and all the stakeholders involved in care of preterm babies is essential to prevent avoidable visual impairment. Forget about all egos and politics, work as a team of neonatologists, nursing staff and ophthalmologists for healthy survival of preterm infants.
[1]. Preterm Birth [Internet]. World Health Organisations. 2018 [cited 2020 Jul 3]. Available from: https://www.who.int/news-room/fact-sheets/detail/preterm-birth [Google Scholar]
[2]. Radhakrishnan N, Pillai GS, Kiran KR, Lekshmypriya A, Retinopathy of prematurity-An overviewKerala J Ophthalmol 2017 29(3):15410.4103/kjo.kjo_111_17 [Google Scholar] [CrossRef]
[3]. Goyal A, Giridhar A, Gopalakrishnan M, Real-world scenario of retinopathy of prematurity in KeralaKerala J Ophthalmol 2017 29(1):3010.4103/kjo.kjo_45_17 [Google Scholar] [CrossRef]
[4]. Akkawi MT, Shehadeh MM, Shams AN, Al-Hardan DM, Omar LJ, Almahmoud OH, Incidence and risk factors of retinopathy of prematurity in three neonatal intensive care units in PalestineBMC Ophthalmol 2019 19(1):18910.1186/s12886-019-1180-431429728 [Google Scholar] [CrossRef] [PubMed]
[5]. World Health Organisation. Vision 2020 [Internet]. WHO Regional Office for South-East Asia. 19-20 December 2007 [cited 2020 May 5]. Available from: https://apps.who.int/iris/handle/10665/206523 [Google Scholar]
[6]. Vinekar A, Dogra M, Azad RV, Gilbert C, Gopal L, Trese M, The changing scenario of retinopathy of prematurity in middle and low income countries: Unique solutions for unique problemsIndian J Ophthalmol 2019 67(6):71710.4103/ijo.IJO_496_1931124475 [Google Scholar] [CrossRef] [PubMed]
[7]. Vinekar A, Dogra MR, Sangtam T, Narang A, Gupta A, Retinopathy of prematurity in Asian Indian babies weighing greater than 1250 gms at birth: Ten-year data from a tertiary carecentre in a developing countryIndian J Ophthalmol 2007 55:331-36.10.4103/0301-4738.3381717699940 [Google Scholar] [CrossRef] [PubMed]
[8]. Coe K, Nursing update on retinopathy of prematurityJ Obstet Gynecol Neonatal Nurs 2007 36(3):288-92.10.1111/j.1552-6909.2007.00151.x17489936 [Google Scholar] [CrossRef] [PubMed]
[9]. Bossi E, Koerner F, Retinopathy of prematurity (Retrolental fibroplasia): Old and new factsHelv Paediatr Acta 1982 37(5):413-20. [Google Scholar]
[10]. Molinari A, Weaver D, Jalali S, Classifying retinopathy of prematurityCommunity Eye Health 2017 30(99):55 [Google Scholar]
[11]. International Committee for the Classification of Retinopathy of PrematurityThe International Classification of Retinopathy of Prematurity RevisitedArch Ophthalmol 2005 123(7):991-99.10.1001/archopht.123.7.99116009843 [Google Scholar] [CrossRef] [PubMed]
[12]. Darlow BA, Gilbert CE, Quiroga AM, Setting up and improving retinopathy of prematurity programs: Interaction of neonatology, nursing and ophthalmologyClin Perinatol 2013 40(2):215-27.10.1016/j.clp.2013.02.00623719306 [Google Scholar] [CrossRef] [PubMed]
[13]. Jagannath A, Wavare C, Biju J, Incidence and risk factors of retinopathy of prematurity in a tertiary eye care centre in Southern IndiaInternational J Current Med and Applied Sci 2016 12(2):99-106. [Google Scholar]
[14]. Kalyan GE, Moxon SA, The role of neonatal nurses in the prevention of retinopathy of prematurityIndian Pediatrics 2016 53:S143-50. [Google Scholar]
[15]. Quiroga A, Moxon S, Preventing sight-threatening ROP: The role of nurses in reducing the riskCommunity Eye Health 2017 30(99):53 [Google Scholar]
[16]. Kiranmayee PS, Kalluri V, India to gear up to the challenge of “third epidemic” of retinopathy of prematurity in the worldIndian J Ophthalmol 2019 67(6):72610.4103/ijo.IJO_700_1831124480 [Google Scholar] [CrossRef] [PubMed]
[17]. Murki S, Kadam S, Role of neonatal team including nurses in prevention of retinopathy of prematurityCommunity Eye Health 2018 31(101):11-15. [Google Scholar]
[18]. Deodari A, Darlow BA, Preventing sight-threatening ROP: Neonatologist’s perspectivesCommunity Eye health 2017 30(99):50-52. [Google Scholar]
[19]. Katoch D, Dogra M, The role of advocacy and communication in reducing ROP in IndiaCommunity Eye Health 2018 31(101):32-34. [Google Scholar]
[20]. Hosamani S, Kumar S, Vinekar A, Vallabha K, Biradar S, Warad V, Comparison of tele screening for retinopathy of prematurity screening and impact of neonatal team support in government and private centers in rural Bijapur district of Southern IndiaJ Vision Sci 2015 1(2):15-20. [Google Scholar]
[21]. Fierson WM, American Academy of Pediatrics Section on OphthalmologyScreening examination of premature infants for retinopathy of prematurityPediatrics 2018 142(6):e2018306110.1542/peds.2018-306130478242 [Google Scholar] [CrossRef] [PubMed]
[22]. Rashtriya Bal Swasthya Karyakram Ministry of Health & Family Welfare Government of India. Guideline for universal eye screening in newborn including Retinopathy of Prematurity [Internet]. June 2017 [cited 2020 Jun 3]. Available from: https://nhm.gov.in/images/pdf/programmes/RBSK/Resource_Documents/Revised_ROP_Guidelines-Web_Optimized.pdf [Google Scholar]
[23]. Jalali S, Anand R, Kumar H, Dogra MR, Azad R, Gopal L, Programme planning and screening strategy in retinopathy of prematurityIndian J Ophthalmol 2003 51(1):89 [Google Scholar]
[24]. Honavar SG, Do we need India-specific retinopathy of prematurity screening guidelines?Indian J Ophthalmol 2019 67:711-16.10.4103/ijo.IJO_973_1931124474 [Google Scholar] [CrossRef] [PubMed]
[25]. Sen P, Rao C, Bansal N, Retinopathy of prematurity: An updateSci J Med & Vis Res Foun 2015 33(24):93-96. [Google Scholar]
[26]. Quinn G, Gilbert C, Treating ROP: How and whenCommunity Eye health/International Centre for Eye Health 2017 30(99):59 [Google Scholar]
[27]. Vijayalekshmi P, Gilbert C, Following up children born pretermCommunity Eye Health 2017 30(99):62 [Google Scholar]
[28]. Uhumwangho OM, Israel-Aina YT, Awareness and screening for retinopathy of prematurity among paediatricians in NigeriaJournal of the West African College of Surgeons 2013 3(3):33 [Google Scholar]
[29]. Akkawi MT, Qaddumi JA, Issa HR, Yaseen LJ, Awareness of retinopathy of prematurity among paediatricians in West Bank, Palestine: A descriptive studyBMC Ophthalmol 2018 18(1):19510.1186/s12886-018-0876-130103708 [Google Scholar] [CrossRef] [PubMed]
[30]. Vinekar A, Azad R, The Indian Retinopathy of Prematurity (iROP) society: Challenges aheadIndian J Ophthalmol 2019 67(6):72210.4103/ijo.IJO_852_1931124477 [Google Scholar] [CrossRef] [PubMed]
[31]. Sathiamohanraj SR, Shah PK, Senthilkumar D, Narendran V, Kalpana N, Awareness of retinopathy of prematurity among paediatricians in a tier two city of South IndiaOman Journal of Ophthalmol 2011 4(2):77-80.10.4103/0974-620X.8365821897623 [Google Scholar] [CrossRef] [PubMed]
[32]. Raiturcar TP, Cacodcar JA, Dubhashi A, Aguiar M, Knowledge, attitude, and practice study on awareness of retinopathy of prematurity among paediatricians in GoaJ Clin Neonatology 2019 8(2):10610.4103/jcn.JCN_13_19 [Google Scholar] [CrossRef]
[33]. Padhi TR, Badhani A, Mahajan S, Savla LP, Sutar S, Jalali S, Barriers to timely presentation for appropriate care of retinopathy of prematurity in Odisha, Eastern IndiaIndian J Ophthalmol 2019 67(6):82410.4103/ijo.IJO_972_1831124495 [Google Scholar] [CrossRef] [PubMed]
[34]. Hariharan L, Gilbert CE, Quinn GE, Barg FK, Lomuto C, Quiroga A, Reducing blindness from Retinopathy of Prematurity (ROP) in Argentina through collaboration, advocacy and policy implementationHealth Policy and Planning 2018 33(5):654-65.10.1093/heapol/czy00429668967 [Google Scholar] [CrossRef] [PubMed]
[35]. Bindu Sankar B, Pappa P, A study to assess knowledge regarding prevention and management of ROP among nurses working in tertiary care centre KeralaIJNER 2018 6(3):263-65.10.5958/2454-2660.2018.00060.1 [Google Scholar] [CrossRef]
[36]. Vinekar A, Gilbert C, Mangat Dogra MK, Shainesh G, Shetty B, Bauer N, The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reportingIndian J Ophthalmol 2014 62(1):4110.4103/0301-4738.12617824492500 [Google Scholar] [CrossRef] [PubMed]
[37]. Kuerschner DR, Does my child really need to wear these glasses? A review of retinopathy of prematurity and long-term outcomesNewborn and Infant Nursing Reviews 2003 3(3):110-17.10.1016/S1527-3369(03)00036-9 [Google Scholar] [CrossRef]
[38]. Sathar A, Abbas S, Nujum ZT, Benson JL, Sreedevi GP, Saraswathyamma SK, Visual outcome of preterm infants screened in a tertiary care hospitalMiddle East Afr J Ophthalmol 2019 26(3):158-62.Available from: http://www.meajo.org/article.asp10.4103/meajo.MEAJO_64_1731619904 [Google Scholar] [CrossRef] [PubMed]
[39]. Shetty SP, Shetty J, Shenoy R, Amin H, The incidence, risk factors and outcome of retinopathy of prematurity at a tertiary care centre in South IndiaIOSR Journal of Dental and Medical Sciences 2015 114(6):77-83. [Google Scholar]
[40]. Kulkarni S, Gilbert C, Kakade N, Dole K, Deshpande CM, Azad R, Habilitation services for children blind from retinopathy of prematurity: Health care professionals’ perspective in MaharashtraIndian J Ophthalmol 2019 67(6):92810.4103/ijo.IJO_573_1831124517 [Google Scholar] [CrossRef] [PubMed]
[41]. Shah SP, Wu Z, Iverson S, Dai S, Specialist nurse screening for retinopathy of prematurity- A pilot studyAsia Pacific Journal Ophthalmol (Phila) 2013 2(5):300-04.10.1097/APO.0b013e31829dc72b26107033 [Google Scholar] [CrossRef] [PubMed]
[42]. Jervis J, Shearer K, Staines M, Mitchell L, Lewis J, Powel R, Implementation of a digital imaging program for ROPJournal of Pediatrics and Child Health 2017 53(2):49-50.10.1111/jpc.13494_143 [Google Scholar] [CrossRef]