Cellular Testicular Fibroma of Gonadal Stroma with Extensive Myoid Differentiation: A Mimicker of Testicular Leiomyoma
Anuradha CK Rao1, Sanila Rahim2, Nazran Akbar Hussain3
1 Professor, Department of Pathology, Yenepoya Medical College, Mangalore, Karnataka, India.
2 Assistant Professor, Department of Pathology, Yenepoya Medical College, Mangalore, Karnataka, India.
3 Postgraduate, Department of Pathology, Yenepoya Medical College, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanila Rahim, Assistant Professor, Department of Pathology, Yenepoya Medical College, Deralakatte, Mangalore, Karnataka, India.
E-mail: sanila_r@yahoo.com
Fibroma of the testis is a rare benign Sex Cord Stromal Tumour (SCST) of probable gonadal stromal origin, occurring in adult males. Characterised by slow and insidious growth, it is devoid of hormonal association and serum markers. Clinically, it can mimic seminoma and requires histopathological examination for identification. Microscopic characteristics include hypercellular spindle cell areas and hypocellular hyaline plaques. Authors report a case of a 41-year-old male presenting with complaints of lower abdominal pain and dysuria. Ultrasonography (USG) showed enlarged left testis with heterogenous echotexture. With a clinical diagnosis of testicular tumour, orchidectomy was performed. Histology showed a well circumscribed, encapsulated cellular neoplasm comprising of spindle and fusiform cells in fascicles, nodules and bundles. The cells showed fusiform vesicular nuclei and eosinophilic cytoplasm, focal epithelioid cells with grooved nuclei and occasional mitotic figure. Stromal collagen fibres and hyalinisation were noted. Testicular tissue was seen compressed peripherally. The tumour cells demonstrated positive reactivity for Smooth Muscle Actin (SMA), h-Caldesmon and inhibin, negative for S-100 and CD34 (Cluster of Differentiation) on Immunohistochemistry (IHC). Literature review helped in arriving at a diagnosis of cellular Testicular Fibroma (TF) with myoid differentiation. Testicular spindle cell lesions are rare, and comprise of different entities, one of which is TF. Histology and IHC are useful aids in diagnosis. Awareness of the differential diagnosis and the IHC markers can help in arriving at a conclusive diagnosis.
Fibroma, Myoid gonadal stromal tumour, Sex cord stromal tumours, Testis
Case Report
A 41-year-old male presented with complaints of lower abdominal pain and dysuria of uncertain duration. No previous history of any co-morbidities was elicited. Clinical examination detected scrotal mass. USG abdomen and pelvis showed an enlarged left testis, measuring 8.8×6.1 cm having heterogenous echotexture with no evidence of calcification. Provisional diagnosis of testicular malignancy was done clinically. Standard biochemical analyses of blood, urine tests and tumour markers (alpha-fetoprotein and Beta human chorionic gonadotropin) were within the physiological limits. Subsequently, left inguinal orchidectomy was performed; the specimen received in the histopathology laboratory, together with the membranes measured 9.5×8.5×6 cm, and the cord was 5 cm in length. Outer surface was congested. Cut surface showed pale white well circumscribed tumour with homogenous areas and few haemorrhagic areas [Table/Fig-1].
Left orchidectomy specimen, measuring 9.5×8.5×6 cm, showing pale white homogenous appearance on cut section.

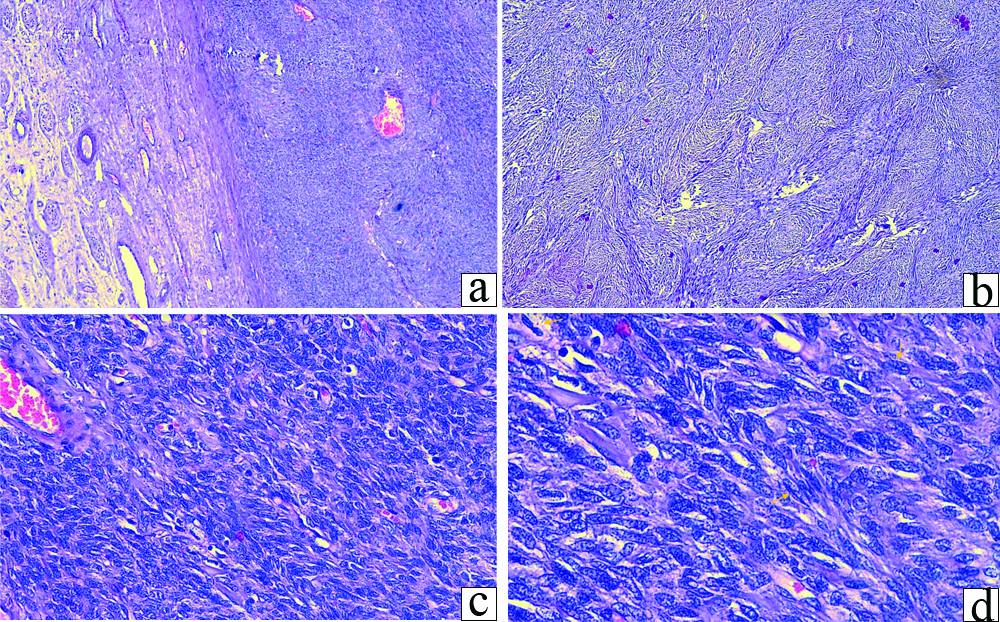
Microscopic examination showed an encapsulated cellular neoplasm comprising of spindle and fusiform cells arranged in interlacing and intersecting fascicles, nodules and bundles [Table/Fig-2a,b]. The cells showed fusiform vesicular nuclei and eosinophilic cytoplasm [Table/Fig-2c]. One mitotic figure per 10 High Power Field (HPF) noted. Few areas showed epithelioid cell morphology with grooved nuclei [Table/Fig-2d]. Stromal collagen fibers and hyalinasation was also seen. The testicular tissue was seen compressed peripherally by the tumour tissue with seminiferous tubules showing marked reduction in germ cell population, interstitial cells and leydig cells.
a) Microscopic examination shows an encapsulated cellular neoplasm (H&E, 4x); b) Spindled and fusiform cells in storiform pattern and vague nodules (H&E, 4x); c) Cells show fusiform vesicular nuclei and eosinophilic cytoplasm (H&E, 20x); d) Focal epithelioid cells with grooved nuclei (arrow marked) seen (H&E, 40x).
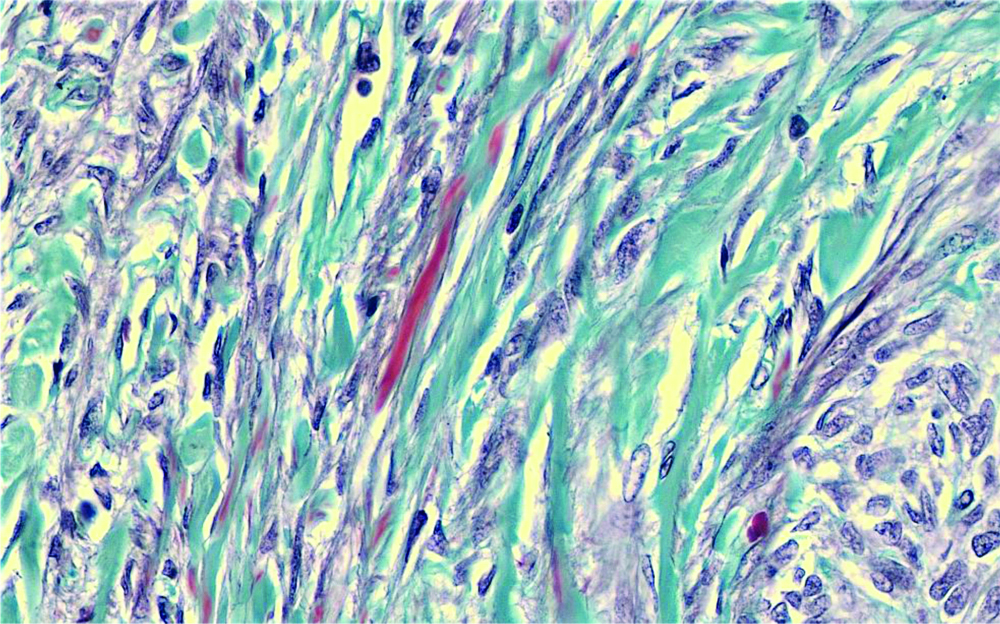
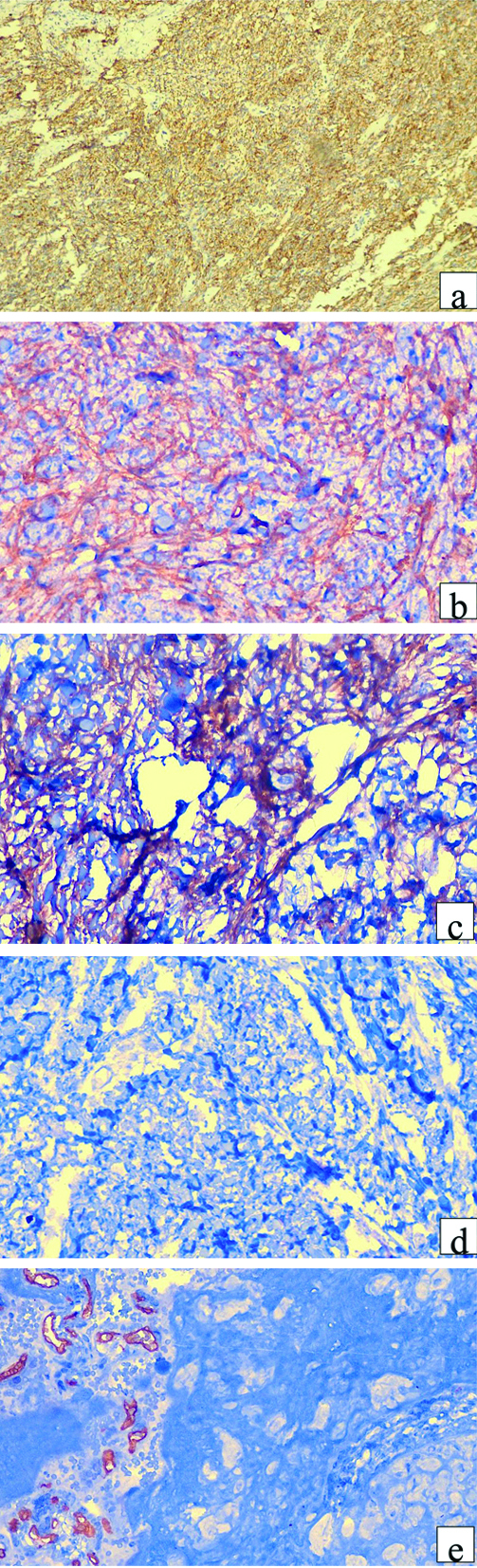
Masson Trichrome (MT) showed focal cytoplasmic fibrils staining red and resembling smooth muscles along with interspersed green fibrous tissue [Table/Fig-3]. A diagnosis of TF of gonadal stromal origin was considered, with a differential diagnosis of testicular leiomyoma because of the MT stain features. IHC was performed, with the spindle cells showing diffuse strong positivity for inhibin, focal positivity for h-caldesmon and SMA [Table/Fig-4]; the cells were negative for CD34 and S-100. A final diagnosis of cellular TF with extensive myoid differentiation was made. Patient was discharged postsurgery, and was subsequently lost to follow-up.
Masson Trichrome (MT) stain (40X): Cells showed focal positivity for smooth muscle (red), and diffuse positivity for fibrous tissue (green).
IHC: Shows positivity for inhibin (a; 4x), SMA (b; 40x), h-caldesmon (focally) (c; 40x) and negative for S-100 (d; 20x) and CD34 (e; 20x).
Discussion
TF are extremely rare benign testicular neoplasms which belongs to the fibroma group under SCST of the testis, comprising 4-6% of all adult testicular tumours [1,2]. TF are thought to be derived from either gonadal stroma, peritubular myoid cells or tunica albuginea [3,4] and resemble their ovarian counterpart histopathologically [1]. Patients range in age from teenage to elderly, with a mean age of presentation being 45 years. The age of presentation of the patient in present case was comparable with the other cases reported in the literature [1,5]. These tumours are not usually associated with any hormonal changes, as in present case and commonly present with slow growing mass, occasionally associated with pain.
These tumours usually present at the centre of the parenchyma of the testis, seen abutting the tunica albuginea or rete testis. The size varies from 0.5-8 cm (mean-2 cm), and as in the present case, are grossly well circumscribed, firm and white on cut surface [4]. Microscopically, these tumours are composed of fibrous spindle cell components, rarely admixed with sex cord elements [3]. The spindle cells are arranged in a form of swirl or fascicles, separated by fibrocollagen and hyalinised stroma with capillaries. Mitotic figures are infrequent, accounting for 1 to 2 per 10 HPF [4]. Cellular fibromas have scanty collagen. A case reported by Darías MJL showed nodular and hyalinising fibrous proliferation which was also seen in present case [5]. To reveal the sex-cord stromal component, IHC of inhibin positivity is needed [6]. IHC is found to be variable, and may not be diagnostic [7]; hence diagnosis relies on exclusion of other entities. These tumours usually express vimentin along with SMA, calretinin, CD56. Frequent expression of S100 and Cytokeratin (CK) has also been reported [3]. Diffuse to patchy inhibin positivity in testicular fibrothecomas has been reported by Zhang M et al., [7]. This case presented with diffuse strong positivity for inhibin, focal positivity for h-caldesmon and SMA; the cells were however negative for CD34 and S-100.
Rare cases have been reported, especially in fibrothecomas with ominous microscopic features such as atypia, focal minimal invasion into normal testicular parenchyma; however, all cases have reported to be behaving as benign tumours [7].
Histopathological differential diagnosis include all other testicular and paratesticular spindle cell neoplasms. One of the greatest mimicker of TF is leiomyoma of the testis and paratesticular region, which shows diffuse positivity for the smooth muscle markers, but however, will be negative for inhibin [3]. Other important differential is myoid gonadal stromal tumour, which is one of the emerging entity, composed of spindle shaped cells showing features of muscle and gonadal stroma. On IHC these show positivity with S-100 (strong) and inhibin (focal and weak) [4,8]. Another entity to be considered is the solitary fibrous tumour, having spindle to oval cells with staghorn pattern of vascular network and IHC positive with CD34. Whereas, fibromas lack staghorn pattern of vascular network and are negative for CD34 [3]. Neurofibroma, can rarely be considered positive for S-100 protein, but negative for Actin, desmin, MIC2 and inhibin on IHC [1]. Unclassified sex cord stromal tumours have incomplete sertoli cell differentiation and show strong S-100 positivity. A rare differential includes fibrosarcoma, which is composed of tumour cells with prominent atypia, along with numerous mitotic figures which is not seen in TF [Table/Fig-5].
Comparison of differential diagnosis: Histopathologial Examination (HPE) and Immunohistochemistry (IHC) [1,3,4,7].
| Tumour | Classical HPE features | Immunohistochemistry |
|---|
| S100 | CD34 | Inhibin | SMA | CD56 |
|---|
| Fibroma | Spindle cells in swirl or fascicles, Fibrocollagenous, hyalinised stroma with capillaries, infrequent mitoses | -/+ | - | +/- Diffuse / focal | + | + |
| Leiomyoma | Whorled pattern of smooth muscle bundles | - | - | - | + | + |
| Solitary fibrous tumour | Spindle to oval cells Staghorn pattern of vascular network | - | + | - | + | - |
| Myoid gonadal stromal tumour | Circumscribed, densely packed, uniform spindle cells in short fasciclesProminent intervening collagen deposit | +, diffuse | - | +/- (focal only) | + | - |
| Neurofibroma | Proliferation of hypocellular bland serpentine spindle cells | + diffuse | + | - | - | - |
| Unclassified sex cord stromal tumour | Variable components of epithelial cells of sex cord type | + other markers : depends on HPE | | | | |
| Fibrosarcoma | Tumour cells with prominent atypia, frequent mitoses, necrosis | - | +/- | - | - | - |
CD: Cluster of differentiation; SMA: Smooth muscle actin
Histopathologically, testicular fibromas are benign cellular spindle cell tumours which can be mistaken for other entities; histology and IHC can aid in differentiation, with diagnosis usually being one of exclusion.
Conclusion(s)
Testicular spindle cell lesions are rare, comprising a small group of entities of varied origin. TF is an important member of this group, which is benign in nature and amenable to therapy with surgical resection. A testicular tumour in an adult male presenting as a tumour of insidious onset, a combination of hypoechoic lesion on ultrasonogram limited to testicular confines, the classical histopathological features armed with IHC markers can help in arriving at a conclusive diagnosis.
CD: Cluster of differentiation; SMA: Smooth muscle actin
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? No
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 21, 2020
Manual Googling: Feb 02, 2021
iThenticate Software: Mar 22, 2021 (8%)
[1]. Tegeltija D, Lovrenski A, Panjković M, Eri Ž, Klem I, Testicular (gonadal stromal) fibroma: Case reportArch Oncol 2012 20(1-2):26-27.10.2298/AOO1202026T [Google Scholar] [CrossRef]
[2]. Sarier M, Tunc M, Ozel E, Duman I, Kaya S, Hoscan MB, Evaluation of histopathologic results of testicular tumours in antalya: Multi-center studyBull Urooncol 2020 19:64-67.10.4274/uob.galenos.2019.1412 [Google Scholar] [CrossRef]
[3]. Unal B, Ipekci T, Hoscan MB, A rare testicular spindle cell tumour: Fibroma of gonadal stromal originInt J Adv Case Reports 2015 2(20):1234-36. [Google Scholar]
[4]. Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE, The 2016 WHO classification of tumours of the urinary system and male genital organs-part b: Prostate and bladder tumoursEur Urol 2016 70(1):106-19.10.1016/j.eururo.2016.02.02826996659 [Google Scholar] [CrossRef] [PubMed]
[5]. Darías MJL, Testicular fibromaRev Cub Med Mil 2016 45(3):391-96. [Google Scholar]
[6]. Jabbour MN, Zaatari GS, Tfayli AH, Abdul-Karim FW, Testicular fibromaJ Urol 2012 188(5):1944-45.10.1016/j.juro.2012.08.05722999552 [Google Scholar] [CrossRef] [PubMed]
[7]. Zhang M, Kao CS, Ulbright TM, Epstein JI, Testicular fibrothecoma: A morphologic and immunohistochemical study of 16 casesAm J Surg Pathol 2013 37(8):1208-14.10.1097/PAS.0b013e318286c12923715159 [Google Scholar] [CrossRef] [PubMed]
[8]. Kao CS, Ulbright TM, Myoid gonadal stromal tumour: A clinicopathologic study of three cases of a distinctive testicular tumourAm J Clin Pathol 2014 142(5):675-82.10.1309/AJCPGSCD1DGNZ0QO25319984 [Google Scholar] [CrossRef] [PubMed]