Introduction
Diabetes is a multi-system disorder, and a varied manifestation of diabetes is known in the eye. The ocular manifestations of diabetes are cataract, vascular occlusions, retinopathies, and optic neuropathies [1]. The optic neuropathies in diabetes present with ischaemic neuropathies, diabetic papillopathy, optic atrophy and retrobulbar neuritis. However, the incidence is only 1.58% [2]. Ischaemic optic neuropathy is a more common involvement of optic nerve in diabetes compared to optic neuritis. A study reported an incidence of optic neuritis as 3.7% [3]. Amongst optic neuritis prototypes, retrobulbar neuritis and papillitis is more often associated with demyelinating disease, compared to perineuritis and neuroretinitis which are more associated with infectious and inflammatory pathologies [4,5]. Papillitis presents with disc oedema, moderate dilatation of veins, retinal haemorrhages and severe loss of vision [6]. Non-arteritic ischaemic optic neuropathy is often associated with diabetes, small disc size and good vision at presentation. The anatomically smaller disc in non-arteritic ishaemic optic neuropathy leads to axoplasmic stasis in the nerve fibre layer and then eventually cell death [7-9]. Colour vision defects are present in optic neuritis but may be spared in non-arteritic ischaemic optic neuropathy due to sparing of central vision [10].
Case Series
Case 1
A 55-year-old female complained of pain and progressive loss of vision in the right eye, since one week. She also had diabetes for three years and was on treatment. There was no history of any other neurological or cranial nerve involvement, joint pain or back pain. The visual acuity recorded in the right eye was 4/60 and left eye was 6/9, with pinhole improvement to 6/6 on Snellen’s visual acuity chart. The left eye improved to 6/6 with-0.75 diopters (D). There was no improvement with refractive aid in the right eye.
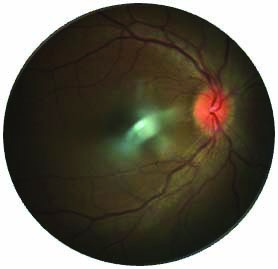
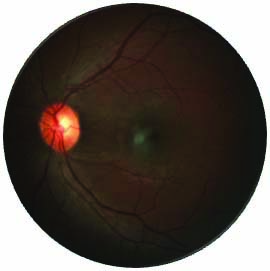
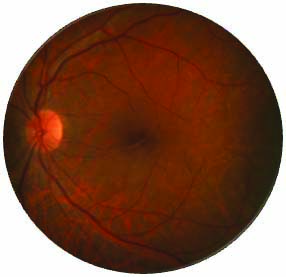
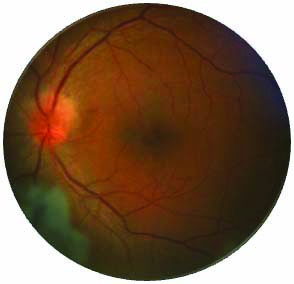
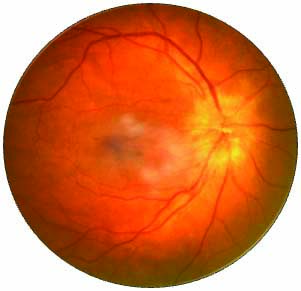
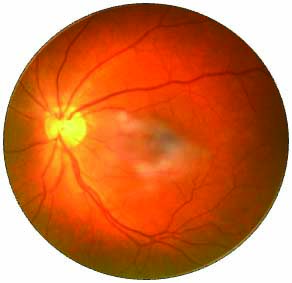
The red colour perception was affected in the right eye compared to the left eye. This was evaluated by showing different shades of red of cloth piece and was tested uniocularly. This was reported as red desaturation in the right eye. On evaluation of the fundus, the right eye fundus showed a disc oedema with disc elevation of 3 D. There were no disc haemorrhages. There were few dot blot haemorrhages in the background qualifying for mild non-proliferative retinopathy of Early Treatment Diabetic Retinopathy Study (ETDRS) classification [Table/Fig-1] [11]. The left eye showed no disc oedema [Table/Fig-2]. The background showed few dot haemorrhages suggestive of mild nonproliferative retinopathy. Confrontation test could not detect any obvious scotoma. The patient was not subjected to perimetry for field defects.
Right eye of the patient showing disc oedema with hyperaemia. No evidence of significant background retinopathy.
Left eye of the patient showing normal disc findings. No evidence of significant background retinopathy.
On evaluating her systemic parameters, the blood sugar level was 360 mg/dL. Since the patient presented with unilateral disc oedema and signs of inflammatory reactions on the disc, demyelination and raised intracranial pressures was not suspected. Hence, Visual Evoked Potential (VEP) and Magnetic Resonance Imaging (MRI) brain were not done.
Since the glycaemic control was poor, the patient was started on IV methyl prednisolone 1 gm under random blood sugar monitoring and insulin therapy for three days. The patient improved symptomatically from day 1 and rapid improvement in vision was seen. Improvement in dyschromatopsia was also seen. After the intravenous therapy, oral prednisolone was started for 11 days at dose of 1 mg/kg body weight.
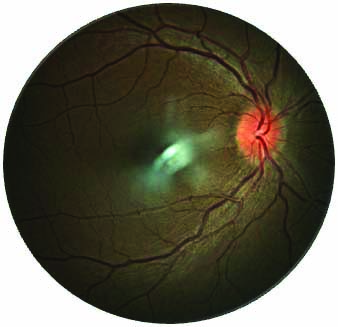
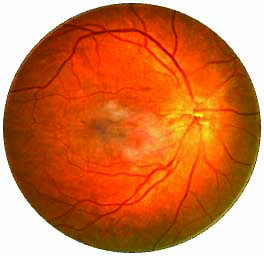
The final visual acuity was observed to be 6/9 in right eye with colour vision regained completely by the end of 11 days. [Table/Fig-3] shows the resolving disc oedema.
Right eye showing resolving disc oedema at day 11 post-treatment.
Case 2
A 42-year-old female presented with the chief complaint of diminution of vision in the right eye since four days, sudden in onset, progressive and associated with mild pain. She was a type 2 diabetic since four years.
On examination, visual acuity in right eye was 5/60 on Snellen’s visual acuity chart without any improvement. Visual acuity in left eye was 6/9 improving to 6/6 with -0.50D sphere. She had impaired colour perception (inability to identify green) and altered red desaturation on evaluation of shades of red. Fundus examination revealed optic disc oedema in right eye with elevation upto 3 disc diopters. There were no haemorrhages on the disc and the background retina did not show any evidence of diabetic retinopathy [Table/Fig-4]. There was no evidence of disc oedema nor any retinopathy features in the left eye of the patient. Left eye retinal examination was within normal limits [Table/Fig-5].
Right eye optic nerve mild disc oedema, hyperaemia and elevation. cup is tilted and full. No evidence background retinopathy.
Left eye fundus within normal limits.
Systemic evaluation revealed a random blood sugar level of 280 mg/dL. She was treated with IV methyprednisolone 1 gm OD (once a day) for three days, followed by tapering doses of oral prednisolone for 14 days along with her anti-diabetic medications. Derangement of sugar was monitored by evaluating the random blood sugar. Color perception and red desaturation returned to normal on day 2 with a visual acuity improving to 6/18 at the end of second day. The visual acuity was 6/12 with improvement in colour vision by the end of day 11. The patient had best corrected visual acuity of 6/9 with -0.5 Dsphere and -0.5 D cylinder at 180° in his right eye. [Table/Fig-6] shows the resolving disc oedema of the patient.
Right eye fundus showing resolving disc oedema at day 3 post-treatment.

Case 3
A 56-year-old male presented with the complaints of diminution of vision of left eye since 10 days, insidious in onset, gradually progressive, associated with mild pain and mild proptosis of the eye. He was a known case of type 2 diabtes mellitus since 10 years and was on treatment.
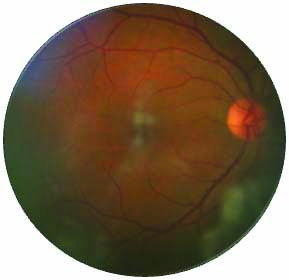
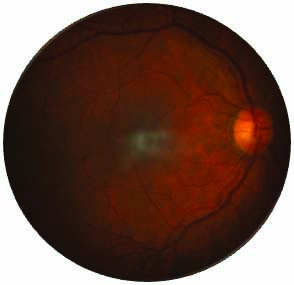
On examination, visual acuity in the right eye was 6/12 improving to 6/9 with -0.75D sphere on Snellen’s visual acuity chart. Visual acuity in the left eye was 3/60 without any improvement. Colour perception was normal on ischiara chart but altered red desaturation was noted. Fundus examination showed few dot blot haemorrhages in background suggestive of mild non-proliferative diabetic retinopathy. The optic disc oedema size was of 3 disc diopters [Table/Fig-7]. The disc oedema was more on the superior and temporal aspect of the disc. There were no disc haemorrhages. Right eye revealed no disc oedema or diabetic retinopathy [Table/Fig-8]. Disc hyperaemia was minimal compared to other cases. CT brain with orbit was done for the proptosis. No intra-orbital abnormality was detected on the Computed Tomography (CT) scan.
Left eye shows disc oedema more on the superior, superonasal and superotemporal quadrant. Disc hyperaemia is mild. No background retinopathy seen.
Right eye fundus within normal limits.
Systemic examination revealed a random blood sugar level of 310 mg/dL. He was treated with IV methyprednisolone 1 g OD for three days, followed by tapering doses of oral prednisolone for 14 days. Colour perception and red desaturation returned to normal on day 2 with no visual improvement. The patient however did not improve even with the complete course of methyl prednisolone and oral corticosteroids [Table/Fig-9]. The patient was lost for follow-up after 15 days, to evaluate the progression.
Left eye fundus showing minimal changes in the disc appearance at day 3 post- treatment.
Case 4
A 50-year-old male presented with the complaints of diminution of vision in right eye since four days, which was sudden in onset, progressive and painless. He was a type 2 diabetic since four years and was on treatment.
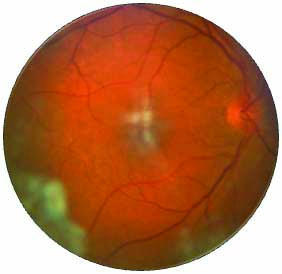
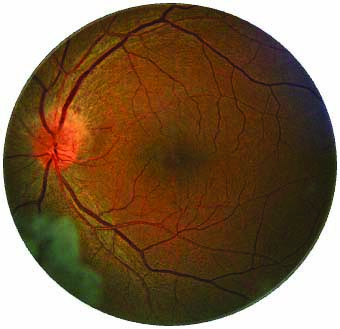
On examination, visual acuity in right eye was 2/60 without any improvement on Snellen’s visual acuity chart. Visual acuity in left eye was 6/18 improving to 6/6 with +0.50D sphere and -1.00D cylinder at 112°. He had an altered red desaturation in the right eye. Fundus examination of right eye revealed optic disc oedema and a disc elevation of 3D [Table/Fig-10]. Disc elevation and disc hyperaemia was significant. There was no evidence of any background retinopathy. Left eye was within normal limits [Table/Fig-11]. Random blood sugar level was 413 mg/dL.
Right eye showing disc hyperaemia, disc oedema, and elevation. No evidence of background retinopathy.
Left eye showing normal disc and retina.
He was treated with intravenous methyprednisolone 1 gm OD for three days, followed by tapering doses of oral prednisolone for 14 days. Colour perception and red desaturation returned to normal on day 2 with a visual acuity improving to 6/12. [Table/Fig-12] shows the resolving disc oedema. The diopteric elevation was evaluated and it showed reduction.
Right eye fundus showing resolving disc oedema at day 3 post-treatment.
Case 5
A 35-year-old female with history of diabetes since one year, came with sudden diminution of vision in the left eye since three days. Random blood sugar was found to be 220 mg/dL at presentation. The fundus evaluation showed disc oedema with disc elevation of 2-3 diopters [Table/Fig-13]. There was presence of hyperaemia, however it was a little obscured due to the tussellated background retina. The presenting vision was 2 meters finger counting on presentation. The background retina did not show any retinopathy features. The right eye was having a visual acuity of 6/12 with pin hole improving to 6/6 with a cylindrical correction of -0.75 diopters at 90° axis.
Left eye showing disc oedema, disc hyperaemia and severely tusselated background retina.

The fundus in the right eye was normal [Table/Fig-14]. The patient was started on the intravenous methyl prednisolone 1 gm per kg body weight for three days followed by oral prednisolone for next 11 days. The patient gained vision to 6/18 with improvement in colour vision by the end of three days. The vision improved to 6/9 by the end of 11 days. The disc oedema showed a significant improvement after 3 days on the diopteric elevation [Table/Fig-15].
Right eye showing normal retina and disc on follow-up.
Left eye fundus showing resolving disc oedema on follow-up.

Discussion
Optic neuropathy manifestations in diabetes are in the form of anterior ischaemic optic neuropathy, posterior optic neuropathy, diabetic papillopathy and rarely optic neuritis [9].
Papillitis has rarely been reported in diabetes. The patients in this case series were found to be in the age range of 35 to 60 years. They presented with profound visual loss, as against that seen in Non-arteritic anterior ischaemic optic neuropathy. The patients also had red desaturation at the time of presentation. Both the visual deficits were found to be reversible. The patients experienced mild pain along with loss of vision. The diopteric elevation of disc oedema in this case series ranged between 2 to 3 disc diopters. The disc oedema was not associated with peripapillary haemorrhages. All patients had hyperglycaemic at the time of presentation. The sugar levels in the patients ranged between 300 to 420 mg/dL on a random blood sugar evaluation.
The patients had minimal diabetic retinopathy and most of the patients had uniocular involvement. A 14 patient case series by Skillern PG and Lockhart G, reported diabetic neuropathy with minimal retinopathy. They postulated the cause of neuropathy to be toxic metabolic changes due to hyperglycaemia. Retinopathy in diabetes is an outcome of microvascular occlusion and microvascular leakage. Minimal background retinopathy with predominant optic neuropathy at the time of presentation was prominent in the case series [10].
The cause for papillitis includes metabolic causes such as diabetes, hypertension, uveitis and multiple sclerosis. Waite JH and Beetham WP, have suggested increased susceptibility of optic nerves to inflammatory mediators that are released in diabetes. The inflammatory mediators are released due to oxidative stress and the alternate metabolic pathways in diabetes [12]. The neuropathies in diabetes are also postulated to be a disturbance of Schwann cell metabolism and also related to the end products of sorbitol pathway [13,14]. There is also a possibility of ischemia of the optic nerve vasculature, leading to pseudopapllitis-like picture [15].
The study by Sinha AK found most of the cases had post-neuritic type of optic neuropathy. This study also reported minimal retinopathy in their case series [16]. Bouomrani S et al., have reported non-arteritic anterior ischemic optic neuropathy to be more common than papillitis however it is in contrast to this case series [17].
Hyperglycaemic state in diabetes is known to cause vascular endothelial dysfunction. There is increased polyol and protein kinase C activity in diabetes causing generation of Advanced Glycation End products (AGE’S) chronic oxidative damage leading to chronic inflammation and aggregation of leucocytes [18-22]. Diacyl-Glycerol (DAG) and Protein Kinase C (PKC) cause inflammation, neovascularisation and alter retinal haemodynamics, which lead to progression of diabetic changes in the eyes [23].
According to the above said pathological factors, alternative metabolic pathway end-products, inflammation and oxidative stress may be the cause of papillitis as a manifestation in all the index cases, as all the cases were in a state of hyperglycaemia at the time of presentation.
Leukostasis is the causative factor for capillary occlusion in diabetics [24]. This has been postulated as one of the causes of diabetic retinopathy. Since the retinopathic changes were found to be less in this case series, it can be presumed that capillary occlusion was relatively less in these patients. This feature also favours the diagnosis against non-arteritic ischaemic optic neuropathy as capillary occlusion is the cause of non-arteritic ischaemic optic neuropathy in diabetes.
It has been reported that systemic immunosuppression can also be tried instead of chronic oral steroids in cases of optic neuritis not associated with demyelinating diseases [25]. The treatment protocol for optic neuritis was followed in this case series since it was suspected to be following inflammatory origin with uncontrolled diabetes mellitus.
In the study by Skillern PG and Lockhart G, the patients had optic nerve involvement with features suggestive of papillitis, (a form of optic neuritis); all of them were started on Intravenous Methyl Prednisolone at the dose of 1 gm IV for three days. They were monitored for blood sugar and shifted to insulin whenever necessary. This was followed with oral steroids at a dose of 1 mg/kg body weight for next 11 days. Improvement in visual acuity and colour vision was seen in most of the cases [10].
Conclusion(s)
Papillitis though rare can be a manifestation in diabetes. The salient features that were found in present case series were mild ocular pain, with disc oedema to a range of 2 to 3 disc diopters, absence of background retinopathy and profound visual loss. The patients were also in a state of hyperglycaemia at the time of presentation of papillitis.
Hence, papillitis should be a differential diagnosis in patient with deranged systemic glycaemic control and optic neuropathy as a presentation.
[1]. Jeganathan V, Wang J, Wong T, Ocular associations of diabetes other than diabetic retinopathyDiabete Care 2008 31(9):1905-12.10.2337/dc08-034218753669 [Google Scholar] [CrossRef] [PubMed]
[2]. Lee J, Han J, Yang M, Oh S, Population-based incidence of pediatric and adult optic neuritis and the risk of multiple sclerosisOphthalmology 2020 127(3):417-25.10.1016/j.ophtha.2019.09.03231732227 [Google Scholar] [CrossRef] [PubMed]
[3]. Pau D, Al Zubidi N, Yalamanchili S, Plant GT, Lee AG, Optic neuritisEye (Lond) 2011 25(7):833-42.10.1038/eye.2011.8121527960 [Google Scholar] [CrossRef] [PubMed]
[4]. Current Diagnosis & Treatment: Pediatrics, 21 ed Chapter 16. Eye Diseases of the Optic Nerve. 2021 [Google Scholar]
[5]. Mansour AM, Shoch D, Logani S, Optic disk size in ischemic optic neuropathyAm J Ophthalmol 1988 106(5):587-89.10.1016/0002-9394(88)90591-0 [Google Scholar] [CrossRef]
[6]. Riva CE, Hero M, Titze P, Petrig B, Autoregulation of human optic nerve head blood flow in response to acute changes in ocular perfusion pressureGraefes Arch Clin Exp Ophthalmol 1997 235(10):618-26.10.1007/BF009469379349945 [Google Scholar] [CrossRef] [PubMed]
[7]. Hayreh SS, Zimmerman MB, Nonarteritic anterior ischemic optic neuropathy: Natural history of visual outcomeOphthalmology 2008 115(2):298-305.e2.10.1016/j.ophtha.2007.05.02717698200 [Google Scholar] [CrossRef] [PubMed]
[8]. Rizzo JF 3rd, Lessell S, Optic neuritis and ischemic optic neuropathy. Overlapping clinical profilesArch Ophthalmol 1991 109(12):1668-72.10.1001/archopht.1991.010801200520241841572 [Google Scholar] [CrossRef] [PubMed]
[9]. Moro F, Doro D, Diabetic optic neuropathies: Clinical featuresMetab Pediatr Syst Ophthalmol (1985) 1986 9(2-4):65-70. [Google Scholar]
[10]. Skillern PG, lockhart G, Optic neuritis and uncontrolled diabetes mellitus in 14 patientsAnnals of Internal Medicine 1959 51:468-75.10.7326/0003-4819-51-3-46813856362 [Google Scholar] [CrossRef] [PubMed]
[11]. Treatment and Clinical Guidelines for photocoagulation of Diabetic Macular oedemaEarly treatment Diabetic retionopathy study report 2. Early treatment Diabetic retinopathy study Research GroupOphthalmology 1987 94(7):761-74.10.1016/S0161-6420(87)33527-4 [Google Scholar] [CrossRef]
[12]. Waite JH, Beetham WP, The visual mechanism in diabetes mellitusNew England J Med 1935 212:367-429.10.1056/NEJM193502282120901 [Google Scholar] [CrossRef]
[13]. Thomas PK, Lascelles RG, Schwann-cell abnormalities in diabetic neuropathyLancet 1965 1(7400):1355-57.10.1016/S0140-6736(65)92154-9 [Google Scholar] [CrossRef]
[14]. Gabbay K, Merola L, Field R, Sorbitol pathway: Presence in nerve and cord with substrate accumulation in diabetesScience 1966 151(3707):209-10.10.1126/science.151.3707.2095907911 [Google Scholar] [CrossRef] [PubMed]
[15]. François J, Vascular pseudopapillitis: Ischemic optic neuropathyAnn Ophthalmol 1976 8(8):901-19. [Google Scholar]
[16]. Sinha AK, Optic nerve involvement in diabetes mellitusIndian J Ophthalmol 1983 31:435-37. [Google Scholar]
[17]. Bouomrani S, Hamed MB, Regaïeg N, Belgacem N, Baïli H, Béji M, Bilateral retrobulbar optic neuritis revealing type 1 diabetes mellitusE Cronicon Neurology 2018 10(6):446-49. [Google Scholar]
[18]. Naruse K, Nakamura J, Hamada Y, Nakayama M, Chaya S, Komori T, Aldose reductase inhibition prevents glucose-induced apoptosis in cultured bovine retinal microvascular pericytesExperimental Eye Research 2000 71(3):309-15.10.1006/exer.2000.088210973739 [Google Scholar] [CrossRef] [PubMed]
[19]. Kowluru R, Diabetic retinopathy: Mitochondrial dysfunction and retinal capillary cell deathAntioxidants & Redox Signaling 2005 7(11-12):158110.1089/ars.2005.7.158116356121 [Google Scholar] [CrossRef] [PubMed]
[20]. Stitt A, The role of advanced glycation in the pathogenesis of diabetic retinopathyExperimental and Molecular Pathology 2003 75(1):95-108.10.1016/S0014-4800(03)00035-2 [Google Scholar] [CrossRef]
[21]. Chu J, Ali Y, Diabetic retinopathy: A reviewDrug Development Research 2008 69(1):01-14.10.1002/ddr.20222 [Google Scholar] [CrossRef]
[22]. Tarr JM, Kaul K, Chopra M, Kohner E, Chibber R, Pathophysiology of diabetic retinopathyISRN Ophthalmology 2013 2013:34356010.1155/2013/34356024563789 [Google Scholar] [CrossRef] [PubMed]
[23]. Klein B, The relation of markers of inflammation and endothelial dysfunction to the prevalence and progression of diabetic retinopathyArchives of Ophthalmology 2009 127(9):117510.1001/archophthalmol.2009.17219752427 [Google Scholar] [CrossRef] [PubMed]
[24]. Nguyen T, Alibrahim E, Islam F, Klein R, Klein B, Cotch M, Inflammatory, haemostatic, and other novel biomarkers for diabetic retinopathy: The multi-ethnic study of atherosclerosisDiabetes Care 2009 32(9):1704-09.10.2337/dc09-010219549733 [Google Scholar] [CrossRef] [PubMed]
[25]. Myers TD, Smith JR, Wertheim MS, Use of corticosteroids sparing systemic immunosuppression for treatment of corticoid dependent optic neuritis not associated with demyelinating diseaseBr Journal of Ophthalmology 2004 17:03-08. [Google Scholar]