Introduction
Foreign Body (FB) aspiration or ingestion into the respiratory or digestive tract is one of the most common emergencies in the paediatric population. Majority of FB ingestion occurs in children under the age of five years with the peak incidence in between six months and three years of age [1].
All three patients, in this case series, were posted for emergency removal of the FB (Lithium-Ion batteries) under general anaesthesia. The written and informed high risk consent from the parents was obtained for each child. The BB or its remnants was emergently extracted under general anaesthesia. The key findings of each case are depicted in [Table/Fig-1]. The details of the cases are described below:
| Case | Age | Sex (M/F) | Diameter of BB (mm) | Time to presentation and location (CXR) | Intervention | Complications |
|---|
| 1 | 5 months | M | 9.5 | 8 hoursCricopharynx | Rigid laryngoscope and removal with Magill’s forceps | Mild inflammation |
| 2 | 2 years | M | 11.6 | 7 daysLeft nasal cavity | Nasal endoscopic removal of foreign body | Ulceration and necrosis of septum and inferior turbinate. Later developed nasal septal perforation |
| 3 | 1.5 years | F | 20 | 24 hoursPharynx | Rigid oesophagoscopy | Mild inflammation |
M: Male; F: Female; BB: Button battery; mm: Millimetre; CXR: Chest X-ray
Case Series
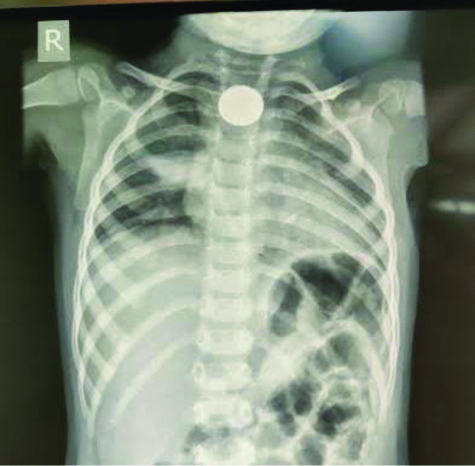
Case 1: A five-month-old male child was brought to the emergency with a history of accidental ingestion of a button battery 8 hours back. The child was febrile (100.2°F) and also had difficulty in breathing and swallowing breast milk. Chest X-ray showed a radio-opaque FB lodged in the cricopharynx [Table/Fig-2].
Button battery in cricopharynx.
The patient was immediately planned for emergency removal of FB by Otorhinolaryngologist (Surgeon). Assessment in the preoperative room revealed tachycardia, tachypnoea, decreased oxygen saturation (up to 82% without oxygen support). Airway examination revealed a short neck and chubby cheeks. After starting oxygen by facemask, the child was wheeled into the Operation Theatre (OT) and standard monitors were attached. The saturation improved to 95%, Heart Rate (HR)-150/min, Respiratory Rate (RR)-46/min. Two paediatric anaesthesiologists were involved in managing this case. Difficult airway cart including fibreoptic bronchoscope was kept ready. The surgeon was prepared for emergency tracheostomy if required. An Intravenous (IV) cannula was inserted following sevoflurane induction and IV glycopyrrolate (10 μg/kg), and ketamine (2 mg/kg) was administered as a part of procedural sedation. Dexamethasone (0.5 mg/kg) IV was also given. The patient was kept on spontaneous ventilation. The surgeon removed the FB with the help of a rigid laryngoscope and a Magill’s forceps. A blackish tar discolouration of the posterior pharyngeal wall was seen.
For further inspection the plane was deepened by IV propofol (1 mg/kg) and rigid bronchoscopy and oesophagoscopy revealed no other abnormalities or oesophagal perforation. A nasogastric feeding tube was inserted for further management in case of a possibility of stricture in future. The child was kept on 100% oxygen and shifted to Post Anaesthesia Care Unit (PACU) where he regained consciousness. Child remained haemodynamically stable, and was allowed oral feeds after 24 hours of the procedure.
Case 2: A two-year-old male, presented with history of foul smelling discharge from left nostril for the seven days and fever for the last five days. There was no specific history regarding FB insertion.
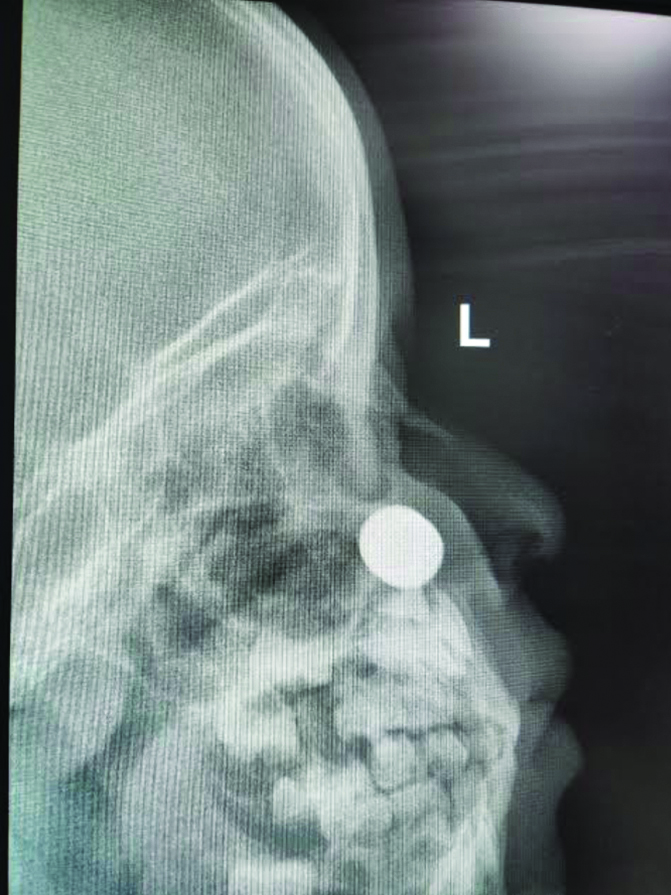
On examination, the child had a high grade fever and foul smelling blackish fluid discharging from the left nostril. A shining FB was spotted between middle concha and septum inside the left nasal cavity. The surrounding skin appeared inflamed. An X-ray (lateral view) of the face was done, which revealed a FB embedded in the left nasal cavity [Table/Fig-3]. Laboratory investigations revealed Haemoglobin 9 g/dL, total leucocyte count 18000/cumm.
Intranasal foreign body (button battery).
The child was posted for emergency nasal endoscopic examination and removal of FB. The patient’s HR-130/min. RR-34/min and Oxygen Saturation (SpO2)-98% on room air. Intravenous (IV) induction was done with propofol (2 mg/kg), fentanyl (1 μg/kg), along with IV glycopyrrolate (10 μg/kg), and dexamethasone (0.5 mg/kg). Rapid sequence induction with succinylcholine (2 mg/kg) was done and child was intubated with a cuffed Endotracheal Tube (ETT) (4.0 mm). Anaesthesia was maintained with the oxygen-air mixture and sevoflurane. Nasal endoscopy was performed, but the BB could not be traced inside the nasal cavity, except some remnants. The impaction had produced ulceration and necrosis of septum and inferior turbinate. The left nasal cavity mucosa was extensively damaged, with exposed blackened septal cartilage laterally along the inferior turbinate. The contra-lateral septal mucosa was intact, but black discolouration was observed. All crusts and necrotic tissues were removed, nasal cavities were irrigated with saline, and topical antibiotic ointment was applied. The child was extubated after adequate suctioning and kept in lateral position along with oxygen face mask.
Postoperatively, the child was shifted to Paediatric Intensive Care Unit (PICU) for observation and kept nil orally for 24 hours. He received IV antibiotics and saline nasal spray. He developed a septal perforation after one month of the procedure due to liquefaction of the nasal mucosa by the alkaline button battery.
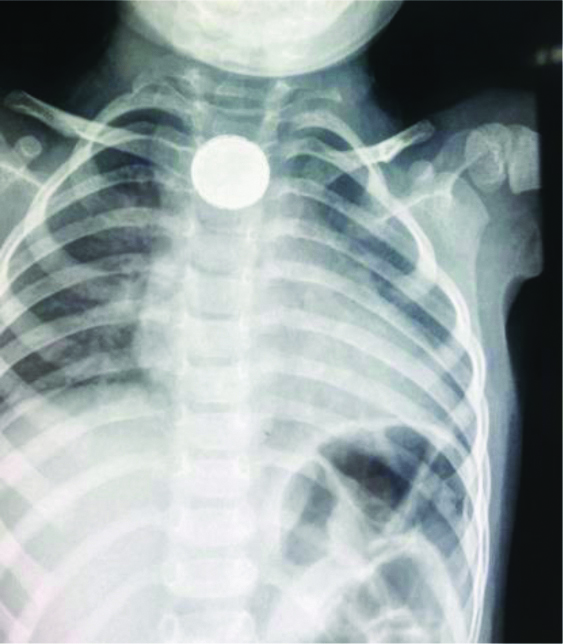
Case 3: A one and a half-year-old female child presented with 24 hours of cough, excessive crying, increased oral secretions, and refusal to eat. Her parents gave an alleged history of BB ingestion while playing with a remote control device. A chest radiograph of the neck anterior posterior view revealed a radiopaque BB in the pharynx [Table/Fig-4].
Button battery in the pharynx.
An emergency rigid oesophagoscopy was planned under general anaesthesia. An IV access was secured in the preoperative room and the child was shifted to the OT. The vitals were: HR-140/min, RR-30/min, and SpO2-98% on room air. She was sedated with ketamine (2 mg/kg) and fentanyl (1 μg/kg) along with glycopyrrolate (10 μg/kg) and dexamethasone (0.5 mg/kg), and 100% oxygen was given via facemask. The otorhinolaryngologist removed the BB with the help of an endoscope. On further examination, no mucosal ulceration or bleeding was seen. The postprocedure course was uneventful. The patient was kept for overnight observation and discharged on the next day.
Discussion
The Button Battery (BB) are small round batteries found in electronics gadgets. The incidence of BB related emergencies in children has increased over the past two decades since its first description in 1977 [2]. The smooth and shiny appearance makes BB attractive to children, and they often place it inadvertently in the ear or nose and accidentally aspirate or swallow it [3].
Several mechanisms of injury have been suggested such as direct corrosive damage, chemical toxicity depending on the contents (manganese, silver, mercury, lithium, or zinc), mucosal burns from electrical current, and pressure necrosis [4]. The leaked alkaline electrolyte solution can cause the dissolution of protein and collagen, saponification of lipids, dehydration of tissue cells resulting in extensive tissue injury [5].
Non-specific symptoms such as fever, irritability, cough, dysphonia, dyspnoea, stridor, and choking and gastrointestinal complaints including vomiting, drooling, dysphagia can occur [6]. The complications following BB ingestion or inhalation depends on the site and the duration of impaction. A child of <5 years of age with a BB ≥20 mm in diameter impacted in the oesophagus at the level of the aortic arch or those with hematemesis or haemoptysis is at a highest risk for significant morbidity and mortality [7].
In infants and children as the pulmonary gas exchange is already reduced thus, maintaining the airway for adequate ventilation and oxygenation for rigid bronchoscopy is a challenging procedure. In the case of acute respiratory distress and hypoxemia with FB, inhalational anaesthesia with monitoring along with gently assisted ventilation and early intubation is important. Muscle relaxant is usually not given because of the degree of total airway obstruction.
In a child with a most stable condition an IV induction with IV induction agents (e.g., sodium thiopental, ketamine or propofol) is used [8]. In this series, ketamine hydrochloride was the preferred (case 1 and 3) drug in emergency situation as it prevents bronchospasm, is cardio-stable and maintains cough reflex thereby preventing aspiration in full stomach patients [9]. In this series, succinylcholine was used in anticipation of short intervention time for the satisfactory muscle relaxation.
Here, both the patients presented within 24 hours and there was mild inflammation of local tissues, while in one case which presented after seven days, BB was dissolved and local liquefaction of nasal septum by the alkaline BB was seen. The recent BB ingestion management guideline from the National Capital Poison Center recommends immediate removal of BB (preferably within 2 hours of ingestion) to avoid morbidity and mortality [10]. The oral administration of mitigating liquids like sucralfate or honey in children older than 12 months of age has been proposed while waiting for the surgery to decrease the depth of alkaline burns to adjacent tissue. Hence, vigilant monitoring and manual ventilation is preferable. After the procedure ends, patients should be returned to consciousness quickly with the airway reflexes intact to protect the recently instrumented airway.
After removal of the FB, the patient should be observed postoperatively and follow-up subsequently since the ongoing alkali damage may continue for a long duration [11]. The authors observed septum perforation in the second child following removal of BB residue, as a result of liquefaction of nasal septum.
Children should be observed after bronchoscopy in the postanaesthesia recovery room for stridor, respiratory distress, haemorrhage, and bronchospasm and a chest radiograph must be done to rule out barotrauma or pneumothorax [12]. Success depends on proper clinical history, X-ray chest and appropriate surgical and anaesthetic management.
In the index cases, prompt removal of the impacted FB (BB or its remnants) by the Ear Nose Throat (ENT) surgeon helped in achieving smooth and uneventful anaesthesia.
Conclusion(s)
Button Battery (BB) impaction in aerodigestive tract is a dangerous form of FB aspiration or ingestion in the paediatric population and early removal of BB is very important and real emergency. A multidisciplinary approach along with the team includes an emergency physician, anaesthesiologist, otorhinolaryngologist or paediatric surgeon, pulmonologist or paediatric gastroenterologist and radiologist. Anaesthesiologist also play a pivotal role in the perioperative management in such cases.
M: Male; F: Female; BB: Button battery; mm: Millimetre; CXR: Chest X-ray
[1]. Kendigelen P, The anaesthetic consideration of tracheobronchial foreign body aspiration in childrenJ Thorac Dis 2016 8(12):3803-07.10.21037/jtd.2016.12.6928149580 [Google Scholar] [CrossRef] [PubMed]
[2]. Bakshi SS, Button battery ingestionBalkan Med J 2018 35(2):212-13.10.4274/balkanmedj.2017.052328958977 [Google Scholar] [CrossRef] [PubMed]
[3]. Thabet MH, Basha WM, Askar S, Button battery foreign bodies in children: Hazards, management, and recommendationsBiomed Res Int 2013 2013:84609110.1155/2013/84609123936851 [Google Scholar] [CrossRef] [PubMed]
[4]. McRae D, Premachandra DJ, Gatland DJ, Button batteries in the ear, nose and cervical esophagus: A destructive foreign bodyJournal of Otolaryngology 1989 18(6):317-19. [Google Scholar]
[5]. Jatana KR, Litovitz T, Reilly JS, Koltai PJ, Riders G, Jacobs IN, Paediatric button battery injuries: 2013 task force updateInt J Paediatr Otorhinolaryngol 2013 77:1392-99.10.1016/j.ijporl.2013.06.00623896385 [Google Scholar] [CrossRef] [PubMed]
[6]. Leinwand K, Brumbaugh DE, Kramer RE, Button battery ingestion in children: A paradigm for management of severe paediatric foreign body ingestionsGastrointest Endosc Clin N Am 2016 26(1):99-118.10.1016/j.giec.2015.08.00326616899 [Google Scholar] [CrossRef] [PubMed]
[7]. Brumbaugh DE, Colson SB, Sandoval JA, Karrer FM, Bealer JF, Litovitz T, Management of button battery-induced hemorrhage in childrenJ Paediatr Gastroenterol Nutr 2011 52(5):585-89.10.1097/MPG.0b013e3181f9891621502830 [Google Scholar] [CrossRef] [PubMed]
[8]. Duan Q, Zhang F, Wang G, Wang H, Li H, Zhao J, Vocal cord paralysis following lithium button battery ingestion in childrenEur J Paediatr [Internet] 2020 Available from: http://dx.doi.org/10.1007/s00431-020-03830-110.1007/s00431-020-03830-133048238 [Google Scholar] [CrossRef] [PubMed]
[9]. Gregory GA, Anaesthesia for Thoracic surgeryIn: Paediatric Anaesthesia 2002 4th edition:449-51. [Google Scholar]
[10]. National capital poison center button battery ingestion triage and treatment guideline [Internet]. Poison.org. [cited 2020 Nov 22]. Available from: https://www.poison.org/battery/guideline [Google Scholar]
[11]. Hoagland MA, Ing RJ, Jatana KR, Jacobs IN, Chatterjee D, Anaesthetic implications of the new guidelines for button battery ingestion in childrenAnaesth Analg 2020 130(3):665-72.10.1213/ANE.000000000000402930829672 [Google Scholar] [CrossRef] [PubMed]
[12]. Ryan. Anaesthesia for Otolaryngology Procedures. In: A Practice of Anaesthesia for Infants and Children, 3rd edition 2001; 468-69 [Google Scholar]