The POST is one of the distressing complications in patients receiving general anaesthesia with tracheal intubation. Incidence of POST ranges from 21 to 65% [1]. POST causes undesirable side effects and dissatisfaction in patients who receive general anaesthesia with tracheal intubation [2]. Spine surgeries in prone position necessitates a wire reinforced tracheal tube which possess a larger outer diameter and requires usage of rigid stylet to place the tube. During the perioperative period, patient position is changed twice, from supine to prone after intubation and then prone to supine during extubation which causes a significant irritation because of the movement of the endotracheal tube while changing the position and attributes to more incidence of POST.
Magnesium sulphate which is NMDA receptor antagonist has anti-inflammatory and anti-nociceptive properties by inhibiting NMDA receptor mediated release of neurotransmitters involved in the inflammation and reduce the incidence and severity of POST [8]. Highly selective glucocorticoid dexamethasone exhibits anti-inflammatory and anti-emetic effects which prevents the postoperative tissue injury, oedema, inhibits synthesis of prostaglandins and pain associated with inflammation thereby decreasing the incidence of POST [9,10]. In various studies, the authors compared either intravenous route or nebulisation route and also compared both MgSO4 and dexamethasone with other group of drugs [7,10,11]. However, there are very limited studies comparing these two drugs via nebulisation in preventing POST for surgeries in prone position under general anaesthesia.
This study primarily compared preoperative dexamethasone nebulisation versus MgSO4 nebulisation in reducing the incidence of POST in patients undergoing prone position surgeries under general anaesthesia. The secondary outcome was to grade the severity of POST between the groups and to compare any haemodynamic changes between the two groups.
Materials and Methods
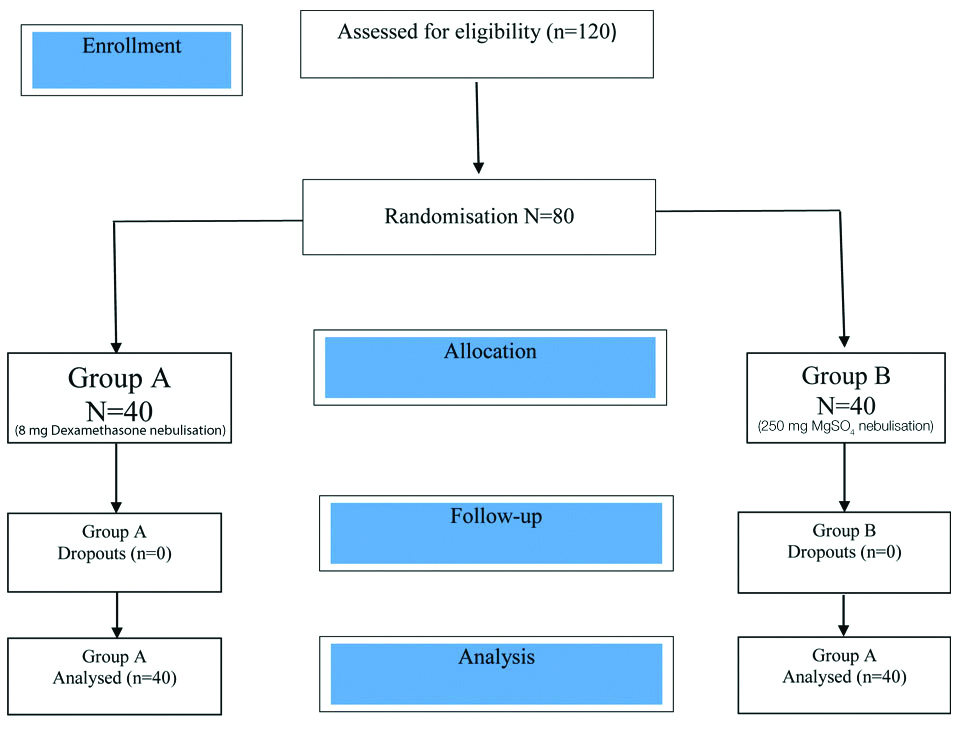
This randomised double blinded trial was conducted in Pondicherry Institute of Medical Sciences from October 2017 to April 2019. after Institutional and Ethical Committee Approval (CTRI NO: 2019/05/019262). From previous study the incidence of POST was taken as 65 (%) and to get a reduction of 50% in the incidence at an alpha error of 0.05 and with a power of 80 (%) [11], the minimum amount of sample required for the study was 35 patients per group. A 10% drop out compensation increased the sample size to 40 patients per group.
After written informed consent, 80 patients undergoing surgery in prone position under general anaesthesia with endotracheal intubation for elective surgery and having met the inclusion criteria were selected.
Inclusion criteria: Patients with ASA [12] I and II of either sex aged 20 to 60 years, Mallampati grade 1 and 2 [13], surgeries lasting less than three hours were included in the study.
Exclusion criteria: Patients with active lower or upper respiratory tract infection, asthma, Chronic obstructive pulmonary disease, women with pregnancy, those patients with Mallampati grade more than 3, known allergies to study drug, patients on chronic medications (NSAID’s, steroids), and ones who required more than one attempt of intubation, or traumatic intubation, known smoker, patients whose intubation may take more than 60 seconds, were excluded from the study.
Patients were grouped as group A and group B by using computer generated random numbers [Table/Fig-1]. All patients in both groups were kept overnight fasting and premeditated with tab ranitidine 150 mg, tab lorazepam 1 mg and tab metoclopramide 10 mg on previous day night before surgery.
After patient arrival to the operation theatre an 18G IV cannula was secured and IV fluids were started. American Society of Anaesthesiologists (ASA) standard monitors like Electrocardiogram (ECG), Non-invasive Blood Pressure (NIBP), and End Tidal Carbon Dioxide (EtCO2) monitoring were attached and baseline parameters like Heat Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP) and oxygen saturation (SPO2) were noted prior to nebulisation, postnebulisation and preinduction. Before giving general anaesthesia, patients received nebulisation of the study drug for 10 minutes with wall mounted oxygen source at 10 L/min (50 psi pressure).
Group A patients received nebulisation with 8 mg dexamethasone in 5 mL of Normal Saline (NS) and Group B patients nebulisation with 250 mg MgSO4 in 5 mL NS.
After nebulisation over a period of five minutes, patients were preoxygenated for three minutes with 100% oxygen via bag and mask and were induced with injection fentanyl 2 micrograms/kg, injection midazolam 20 micrograms/kg, injection propofol 2 mg/kg and injection vecuronium bromide 0.1 mg/kg. Endotracheal intubation was performed with reinforced tube of 8.0-8.5 mm Internal Diameter (ID) for male patients and 7-7.5 mm ID for female patients and tracheal cuff was inflated with air and cuff pressure was maintained at 20 cm of water for every 30 minutes till the end of surgery with the help of cuff pressure monitor. The time for laryngoscopy and time to intubate was documented. In case of traumatic intubation and any more than two attempts for intubation were excluded from the study. After confirmation of flexometallic tube position in trachea, anaesthesia will be maintained with 50:50 mixtures of nitrous oxide and oxygen, isoflurane and maintenance doses of vecuronium bromide. Thirty minutes prior to end of the surgery, injection ondansetron 0.1 mg/kg mg IV and injection paracetamol 15 mg/kg IV will be given. At the end of surgery, with patient adequately anaesthetised, gentle oral suction was done, and isoflurane and nitrous oxide was turned off. Inspiratory oxygen concentration was increased to 100 (%) and after return of spontaneous ventilation, neuromuscular blockade was reversed with injection neostigmine 50 mcg/kg and glycopyrrolate 10 mcg/kg and extubated once patient is fully awake and following oral commands. Patients were shifted to Post Anaesthesia Care Unit (PACU) and monitored and upon arrival to PACU, patient were assessed for incidence and severity of POST at 0 hour. The incidence and severity of POST was assessed from the patients by using the four point scale as mentioned below.
The parameters studied were:
Patients were assessed postoperatively at 0 hour, 4th hour, 6th hour, and 24th hour
Sore throat was defined as continuous throat pain.
Hoarseness was defined as abnormal voice change.
Cough was defined as a sudden noisy expulsion of air from the lungs.
The severity of POST was assessed by a four point scale (0-3) as follows:
Sore throat
0 No sore throat at any time since the operation
1 Minimal sore throat
2 Moderate sore throat
3 Severe sore throat
Hoarseness
0 No complaint of hoarseness
1 Minimal change in quality of speech (minimal hoarseness)
2 Moderate change in quality of speech (moderate hoarseness)
3 Gross change in quality of speech (severe hoarseness)
Cough
0 No cough at any time since the operation
1 Minimal cough
2 Moderate cough
3 Severe cough
Statistical Analysis
All data were entered in an Excel®-Sheet for documentation. For statistical analysis, the program SPSS 20.0® for Windows was used. Continuous variables were expressed as mean±SD and were analysed by using student t-test. Categorical variables were expressed in numbers and percentages, and were analysed by using Chi-square test. Overall incidence and mean severity of POST significance were analysed by Fisher-exact test and Mann-Whitney U test, respectively. Statistical significance was defined as p<0.05.
Results
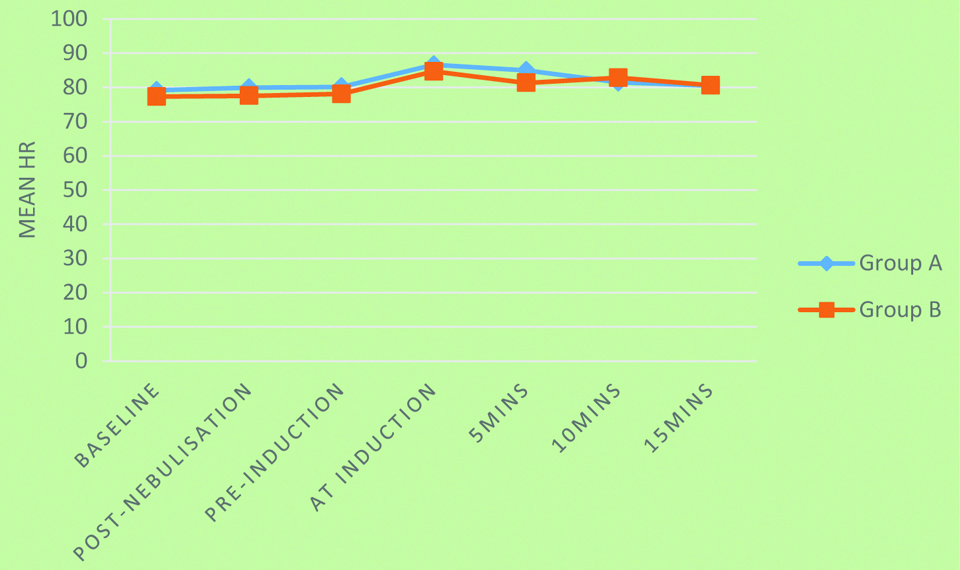
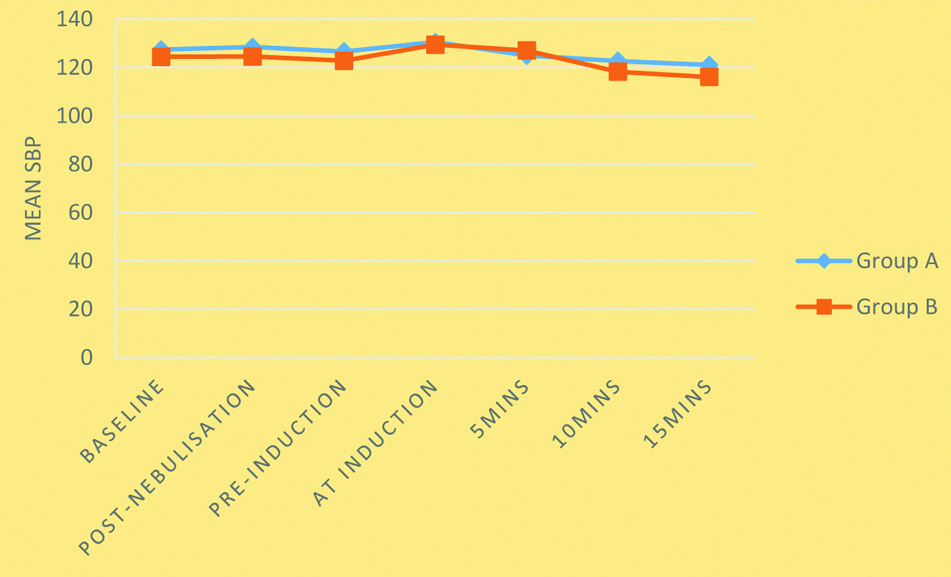
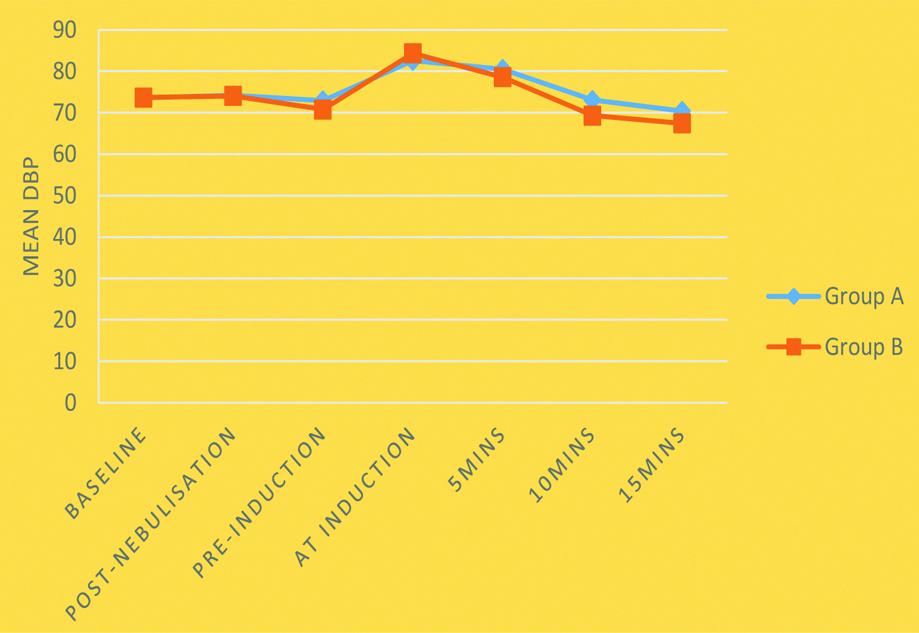
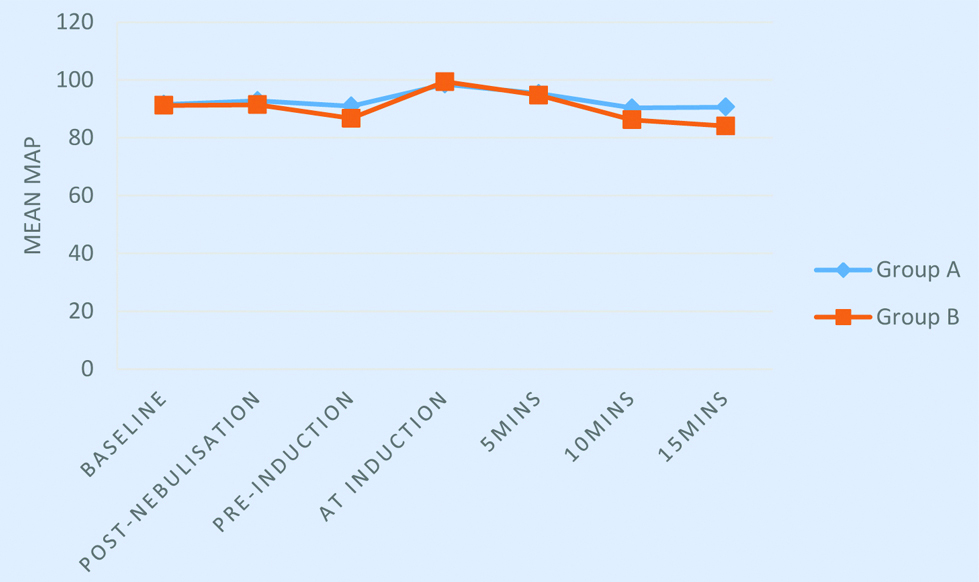
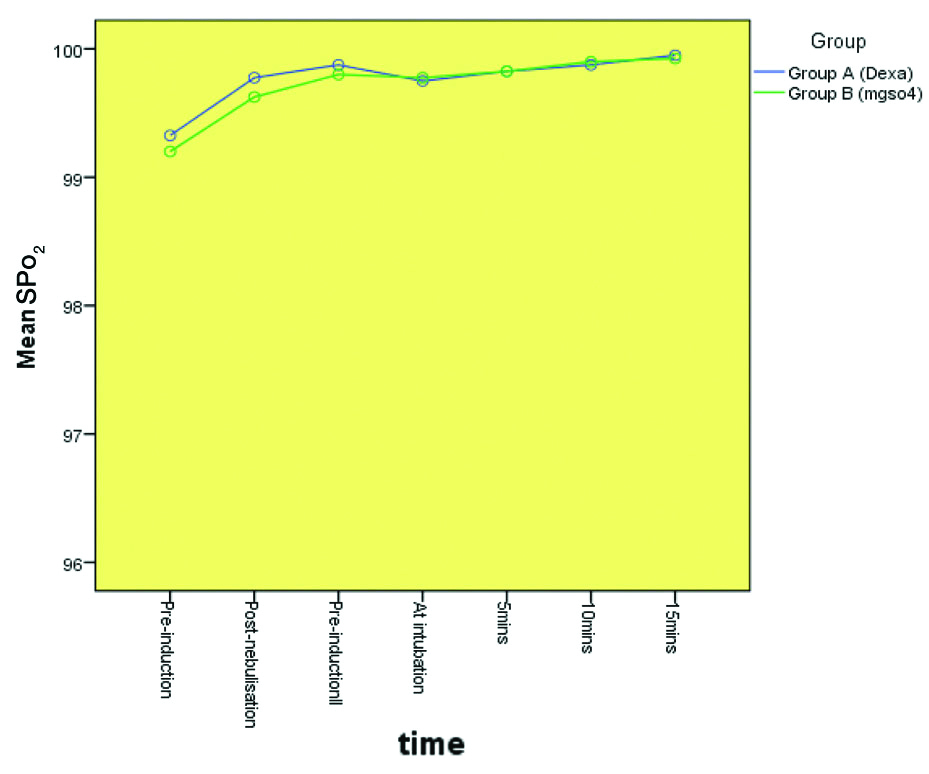
Eighty patients, belonging to ASA Physical status I and II undergoing surgeries under general anaesthesia in prone position, were included in the study. They were randomly divided into Dexamethasone (Group A) and MgSO4 group (Group B) and were evaluated for efficacy of dexamethasone and MgSO4 nebulisation preoperatively in attenuating the POST. On comparing the demographic profile [Table/Fig-2] there was no statistically significant difference between two groups. On comparing the surgical duration there was no statistically significant difference between the two groups [Table/Fig-3]. The haemodynamic parameters such as Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP) and Mean Arterial Pressure (MAP) did not show statistically significant difference between both the groups following prenebulisation and postnebulisation [Table/Fig-4,5,6,7 and 8]. The overall incidence of sore throat in group A was 37.5% and in group B was 20%. At immediate postoperative 0 hours and 24 hours none of the patients complained of sore throat in both the groups and at 0, 4, 6, 24 hours none of the patients complained of cough and hoarseness in both the groups. At 6 hours, there was a statistically significant difference between both the groups (p=0.026) [Table/Fig-9,10 and 11]. MgSO4 group significantly reduced sore throat at 6 hours comparing to dexamethasone group.
| Demographic profile (mean) | Group A | Group B | p-value |
|---|
| Age (years) | 36.13±7.796 | 39.13±8.428 | 0.102 |
| Sex (M:F) | 24:16 | 20:20 | 0.369* |
| Height (cm) | 166.50±6.575 | 164.28±7.589 | 0.165 |
| Weight (kg) | 62.43±8.578 | 60.15±9.828 | 0.273 |
| ASA (I:II) | 33:7 | 32:8 | 0.775* |
Student’ unpaired t-test/*Chi-square test used to calculate the p-values
Mean duration of surgery in minutes (Mins.).
| Group | Mean | Std. DDeviation | p-value |
|---|
| Duration of Surgery_(Mins.) | Group A (Dexa) | 107.95 | 27.597 | 0.695 |
| Group B (MgSO4) | 110.18 | 22.785 |
| Total | 109.06 | 25.170 |
(Student’s unpaired t-test used for calculating p-values; Dexa: Dexamethasone; MgSO4: Magnesium sulphate
Mean HR among groups.
Repeated Measures ANOVA was used; p-value=0.081; HR: Heart rate
Mean SBP among groups.
Repeated Measures ANOVA was used; p-value=0.018; SBP: Systolic blood pressure
Mean DBP among groups.
Repeated Measures ANOVA was used; p-value=0.057; DBP: Diastolic blood pressure
Mean MAP among groups.
Repeated Measures ANOVA was used; p-value=0.048; MAP: Mean arterial pressure
Mean SPO2 among groups.
Repeated Measures ANOVA was used; p-value=0.519; Dexa: Dexamethasone; MgSO4: Magnesium sulphate
Sore throat among study participants.
| Sore throat | Group | Total | p-value |
|---|
| Group A (Dexa) | Group B (MgSo4) |
|---|
| 0 hour | Absent | 40 | 40 | 80 | nil |
| 4th hour | Present | 9 | 8 | 17 | 0.785 |
| Absent | 31 | 32 | 63 |
| 6th hour | Present | 6 | 0 | 6 | 0.026 |
| Absent | 34 | 40 | 74 |
| 24th hour | Absent | 40 | 40 | 80 | nil |
None of the patient complained of cough and hoarseness between the two groups; Chi-square test/Fisher’s-Exact test were used to calculate the p-values; Dexa: Dexamethasone; MgSO4: Magnesium sulphate
Severity of sore throat among the groups.
| Hours | Severity | Dexa | MgSo4 | p-value (Chi-square test) |
|---|
| 0 | Grade 0 | | | |
| Grade 1 | NIL | NIL | NA |
| Grade 2 | | | |
| Grade 3 | | | |
| 4 | Grade 0 | 0 | 0 | |
| Grade 1 | 5 | 4 | 0.785 |
| Grade 2 | 4 | 4 | |
| Grade 3 | 0 | 0 | |
| 6 | Grade 0 | 0 | 0 | |
| Grade 1 | 3 | 0 | 0.026* |
| Grade 2 | 3 | 0 | |
| Grade 3 | 0 | 0 | |
| 24 | Grade 0 | | | |
| Grade 1 | NIL | NIL | NA |
| Grade 2 | | | |
| Grade 3 | | | |
Dexa: Dexamethasone; MgSO4: Magnesium sulphate
Mean severity score among study participants according to groups [10].
| Mean severity score | Group | Mean | Std. Deviation | p-value* |
|---|
| 0 hour severity score | Group A (Dexa) | 0 | 0 | 1.000 |
| Group B (MgSO4) | 0 | 0 |
| 4 hours severity score | Group A (Dexa) | 0.33 | 0.656 | 0.808 |
| Group B (MgSO4) | 0.30 | 0.648 |
| 6 hours severity score | Group A (Dexa) | 0.23 | 0.577 | 0.011 |
| Group B (MgSO4) | 0 | 0 |
| 24 hours severity score | Group A (Dexa) | 0 | 0 | 1.000 |
| Group B (MgSO4) | 0 | 0 |
*Mann-Whitney U test; p-value<0.05 significant; Dexa: Dexamethasone; MgSO4: Magnesium sulphate
Discussion
This study determined the effect of preoperative dexamethasone nebulisation and MgSO4 nebulisation in attenuating postoperative sore throat in prone position surgeries under general anaesthesia with endotracheal intubation.
Results showed that the overall incidence of sore throat in dexamethasone group was 37.5% and MgSO4 group was 20%. At 0 hours, after extubation none of the patients had sore throat in both the groups. At 6 hours, the incidence of sore throat in dexamethasone group was 6 (15%) and none in MgSO4 group. Hence, it statistically as well clinically lowered the incidence of POST at 6 hours when compared to dexamethasone group (p=0.026). At 24 hours, none of the patient had sore throat and no haemodynamic changes were seen. These results correlates well with the study conducted by Yadav M et al., which showed MgSO4 is effective in reducing incidence of POST [4]. This study showed that nebulisation with MgSO4 significantly reduced the incidence of sore throat in 2nd and 4th hour on swallowing comparing to saline nebulisation. Pain during swallowing was significantly reduced in MgSO4 group at 4 hours postsurgery compared to normal saline group (p=0.046).
Salama A and El Badawy A, compared 8 mg dexamethasone nebulisation and saline nebulisation 15 minutes before general anaesthesia with endotracheal intubation, on arrival to the PACU. After extubation, results showed that POST significantly reduced in the dexamethasone group than in the saline group at the following intervals: 2 hours after extubation (p=0.009); 4 hours after extubation (p-value<0.001); and 12 hours after extubation (p=0.002), which was very similar to the index study where dexamethasone nebulisation decreased POST but not as good as MgSO4 [1].
MgSO4 is better when administered as nebulisation comparing to IV form in reducing the POST. Even dexamethasone acts better in inhaled route compared to IV [6]. Park JH et al., compared MgSO4 30 mg/kg/h IV followed by 10 mg/kg/h by continuous infusion until the end of surgery and dexamethasone 8 mg IV [14]. POST was assessed till 48 hours after the surgery. The overall incidence of POST in MgSO4 group was 68.5 % and 61.5% in dexamethasone group, assessed on swallowing. It was found that prophylactic MgSO4 is non-inferior than dexamethasone for the prevention of POST in patients undergoing lumbar spine surgeries under general anaesthesia in prone position. In this present study, POST in prone position spine surgeries under general anaesthesia showed MgSO4 nebulisation is superior to dexamethasone nebulisation in attenuating POST; but the total incidence was much less in the present study when compared to the study by Park JH et al. [14].
Severity of POST was assessed using four point scale which has a score ranging from 0 to 3. In Yadav M et al., study also found that MgSO4 nebulisation significantly decreased POST at 4 and 24 hour [4]. This is similar to the present study where MgSO4 nebulisation attenuated sore throat comparing to dexamethasone group at 6 hours which is statistically significant and at 24 hours none of these patients had sore throat.
MgSO4 is NMDA receptor antagonist that decreases the the inflammation and nociception thereby it is used to reduce the severity of POST. Administering through nebulisation is the best way to prevent POST as demonstrated by Gupta S et al., compared to the efficacy of nebulised MgSO4. They studied 40 patients belonging to ASA I and II, undergoing elective open cholecystectomy and were randomised in two groups [15]. One group received 3 mL of saline nebulisation and another group received 3 mL of 225 mg of isotonic MgSO4 nebulisation for 15 minutes before induction of general anaesthesia. They assessed the severity of sore throat at 0, 2, 4 and 24 hours postoperatively and found that MgSO4 nebulisation significantly reduced the severity of POST at all time points (p<0.05). Similar findings were stated by Jain S and Barasker S, in their study where a three-group comparison was done between nebulisation with MgSO4, with ketamine and with normal saline [16].
The haemodynamic parameters such as HR, SBP, DBP and MAP did not show statistically significant difference between both the groups following prenebulisation and postnebulisation. Similar outcomes were reported by Rajan S et al., [5] and Salma AK and El Badawy A, [1].
Limitation(s)
Fixed dose was used and least effective dose was not identified. From this present study it is difficult to interpret whether 8 mg of dexamethasone nebulisation is as efficacious as 250 mg of MgSO4 nebulisation.
Conclusion(s)
The present study concludes nebulisation with MgSO4 250 mg before endotracheal intubation significantly reduces the incidence and severity of POST in prone position surgeries compared to dexamethasone nebulisation and there was no statistically significant haemodynamic variability between the two groups.
Student’ unpaired t-test/*Chi-square test used to calculate the p-values
(Student’s unpaired t-test used for calculating p-values; Dexa: Dexamethasone; MgSO4: Magnesium sulphate
None of the patient complained of cough and hoarseness between the two groups; Chi-square test/Fisher’s-Exact test were used to calculate the p-values; Dexa: Dexamethasone; MgSO4: Magnesium sulphate
Dexa: Dexamethasone; MgSO4: Magnesium sulphate
*Mann-Whitney U test; p-value<0.05 significant; Dexa: Dexamethasone; MgSO4: Magnesium sulphate