Cerebral Cysticercosis Masquerading as Eclampsia: A Case Report
Amanjot Kaur1, Beant Singh2
1 Assistant Professor, Department of Obstetrics and Gynaecology, GMC, Patiala, Punjab, India.
2 Professor, Department of Obstetrics and Gynaecology, GMC, Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amanjot Kaur, Assistant Professor, Department of Gynaecology and Obstetrics, GMC and Rajindra Hospital, Patiala, Punjab, India.
E-mail: aman50055@yahoo.com
Neurocysticercosis is a preventable parasitic disease of nervous system caused by Taenia solium. It may present with seizures, focal neurological deficits, decreased visual acuity and altered mental status. Eclampsia is a neurological manifestation of hypertensive disorders of pregnancy presenting as seizures. In common obstetric practice, all cases of unexplained seizures are managed as eclampsia unless proven otherwise. Neurocysticercosis presenting first time in pregnancy with seizures can be confused with eclampsia. The index case was referred to us in a similar manner in the second trimester of pregnancy with a diagnosis of eclampsia. Patient was evaluated further for the cause of seizures and was found to have neurocysticercosis on imaging. She was then conservatively managed and the pregnancy was continued till term rather than termination of pregnancy which is the standard management of eclampsia.
Central nervous system cysticercosis, Generalised tonic clonic seizures, Hypertension, Neurocysticercosis, Parasitic, Pregnancy complications
Case Report
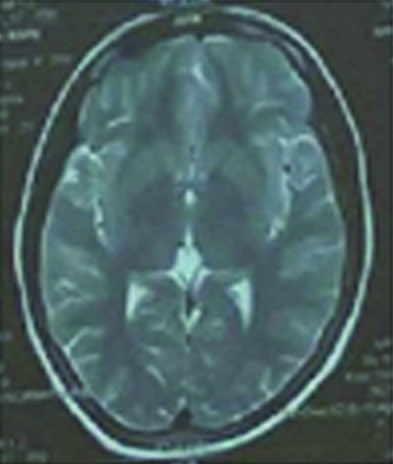
A 20-year-old primigravida at 22 weeks and 3 days of gestation presented with history of an episode of seizure in the morning. It involved tonic clonic activity of all the four limbs associated with uprolling of eyes and loss of bladder control. This patient did not have any prior history of seizure episode or any family history of the same and belonged to rural agricultural background. On presentation to the nearest hospital, the blood pressure of the patient was recorded to be 130/90 mmHg. Keeping a provisional diagnosis of eclampsia in mind, the patient was administered loading dose of magnesium sulfate at the peripheral centre and was referred to higher centre. On reception to higher centre, patient was conscious and oriented to time, place and had stable vitals. Her general physical examination was normal with no evidence of neurological deficit. The abdominal examination was suggestive of 22 weeks pregnancy. Magnesium sulfate prophylaxis was continued. Her complete blood counts, coagulogram, liver and renal function tests, urine analysis and fundus examination was normal. In view of all clinical findings non-consistent with eclampsia-pre-eclampsia syndrome, a Magnetic Resonance Imaging (MRI) was planned. MRI reported two well defined hypointense lesions, one measuring 4.4×5.6 mm in left parietal region (without perilesional oedema) and another measuring 4×4 mm in left frontal region with mild perilesional oedema suggestive of chronic calcified granulomas of neurocysticercosis [Table/Fig-1].
MRI image showing 4.4×5.6 mm granuloma in left parietal region.
Patient was started on tablet levetiracetam 500 mg twice a day (BD) and injection dexamethasone 4 mg i/v BD for five days and then tapered off. Possible adverse effects of the medications were explained to the patient. After observation in the hospital for one week and starting levetiracetam 500 mg BD, patient was discharged from the hospital. There was no further episode of seizure or increased blood pressure. The antenatal period was followed-up as per standard protocol. Patient was induced with dinoprostone gel at 40 weeks gestation and delivered a male baby of 2.965 kg with Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) scores of 8,9.
Discussion
Neurocysticercosis can be confused with eclampsia in a previously undiagnosed patient presenting first time in pregnancy. Eclampsia is the first differential diagnosis in any patient presenting with seizures in the antenatal period. A major reason for this is the fact that the symptoms viz., seizures, visual changes, headache, altered mental status are common in both diseases. However, eclampsia usually presents in the later part of the pregnancy and is usually associated with increased blood pressure. The symptomatology of neurocysticercosis depends on the stage of infection, location of the cysts, and host response to the injury. Fully viable cystic lesions usually remain subclinical unless symptoms are triggered by compression of adjacent structures. Perilesional oedema and seizures are caused by decaying stages (colloidal cysts) or dead cysts (granulomas/calcifications) [1]. While subarachnoid lesions cause stroke and hydrocephalus, ventricular lesions primarily cause hydrocephalus and parenchymal lesions result in seizures. The clinical presentations which have been reported include seizures, hydrocephalus, headache and diplopia [2-6].
The present patient presented with seizure episode at a relatively early gestation. When atypical features are present, or clinical status worsens, in a patient clinically diagnosed as eclampsia, neuroimaging becomes important [2]. While MRI is highly sensitive to identify small non-calcified cysts, oedema, or enhancement around calcifications, and subarachnoid or intraventricular lesions, CT scan is superior to MRI for the evaluation of calcified lesions. CT scan involves radiation; MRI without gadolinium is not associated with teratogenicity and should be the test of choice during any stage of pregnancy [7]. Major differential diagnosis of cerebral neurocysticercosis includes eclampsia, as discussed earlier and tuberculomas. Good history taking, clinical examination, neuroimaging and judicious use of serologic tests helps to clinch the diagnosis. Neurocysticercosis can be treated with minimal interruption to the course of pregnancy. Medical treatment is effective in most cases although surgery may sometimes be indicated [5]. Treatment comprises of antiepileptic drugs with steroid therapy. Major challenges faced during the antenatal period are possible teratogenic effects of antiepileptic drugs and corticosteroid therapy. The risks and benefits of the drugs should be discussed before commencement of therapy. Anti-helminthic drugs should be delayed until postpartum [8].
The pathophysiology of perilesional oedema is still not clear [2]. One school of thought says that it occurs due to intermittent release or recognition of parasite antigen by the host or periodic loss of immune suppression resulting in an inflammatory reaction [9]. However, another hypothesis is that selective calcified lesions have a propensity to cause perilesional oedema through disruption of the blood-brain barrier [10,11]. A prospective study done in Peru was suggestive of presence of perilesional oedema in 50% patients with calcified granulomas presenting with recurring seizures [12]. This suggests the use of concomitant anti-inflammatory agents. The effect of pregnancy on the natural history of the disease is not known due to paucity of existing literature. Possibly, a shift towards type 2 immune response may increase parasite survival and result in disease reactivation and thus clinical symptoms [13]. Various cases which have been reported in the literature have been described in [Table/Fig-2] [2,4,6,14-17].
Various cases of neurocysticercosis discussed in literature [2,4,6,14-17].
| Author | No. of cases | Presentation | Site of lesion | Gestational age | Drug therapy | Surgical management | Outcome |
|---|
| Webb C et al., [2] | 2 | 1. Seizure2. Headache, seizure | Parenchymal (scattered lesion in white matter)Intraventricular(hydrocephalus) | Postpartum day 417 weeks | DivalproexPhenytoin, dexamethasone, mannitol | NoneVP shunt planned | GoodMortality |
| Singhal SR et al., [4] | 2 | 1. Seizure, altered mental status2. Seizure | Parenchymal(frontal)Parenchymal(parietal) | 27 weeks24 weeks | Phenytoin, albendazoleCarbamazepine | NoneNone | GoodGood |
| D’Cruz RF et al., [14] | 1 | Secondary generalised seizures | Parenchymal (right parietal lobe) | 21 weeks | Lamotrigene, levetiracetam | None | Good |
| Padhy SK et al., [6] | 1 | Binocular diplopia, bilateral blurring of vision | Parenchymal (multiple cystic lesions) | 2 weeks postpartum | i/v mannitol,oral acetazolamide, oral antiepileptics | None | Good |
| Saldanha V et al., [15] | 1 | Seizures, coma | Parenchymal(multiple lesions) | 8 dayspostpartum | Phenobarbital, phenytoin | None | Good |
| Ramus RM et al., [16] | 1 | Altered mental status, severe headache | Parenchymal(multiple lesions) and ventricular (hydrocephalus) | 39 weeks | Diphenylhydantoin, praziquantil | Ventriculostomy followed by craniotomy and larval cyst resection after six days of ventriculostomy | Good |
| Sahai S and Sahai A [17] | 2 | 1. Generalised tonic clonic seizures2. Focal seizures | Parenchymal (multiple)Parenchymal(right parietal lobe) | 28 weeks27 weeks | Both cases initially treated as eclampsia, thereafter administered albendazole and anticonvulsants | None | Good |
Conclusion(s)
Neurocysticercosis should be considered as a differential diagnosis in patients presenting with seizures for the first time in pregnancy, specially those living in endemic areas. All patients diagnosed as eclampsia clinically with atypical features should undergo neuroimaging. While the effect of pregnancy on neurocysticercosis needs further research, that of neurocysticercosis on pregnancy remains negligible unless the disease is non-parenchymal and life threatening.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 23, 2020
Manual Googling: Nov 28, 2020
iThenticate Software: Jan 27, 2021 (6%)
[1]. Webb CM, White AC Jr, Update on the diagnosis and management of neurocysticercosisCurr Infect Dis Rep 2016 18(12):4410.1007/s11908-016-0547-427787774 [Google Scholar] [CrossRef] [PubMed]
[2]. Webb C, Rosa M, Olson G, Cabada M, Neurocysticercosis in pregnancyAJP Rep 2018 8(2):e51-e56.10.1055/s-0038-163961529637011 [Google Scholar] [CrossRef] [PubMed]
[3]. Gardner E, Chang M, Mancuso P, Chaney SE, Neurocysticercosis in pregnancy: Not just another headacheNurs Womens Health 2012 16(2):118-24.10.1111/j.1751-486X.2012.01717.x22900769 [Google Scholar] [CrossRef] [PubMed]
[4]. Singhal SR, Nanda S, Singhal SK, Neurocysticercosis as an important differential of seizures in pregnancy: Two case reportsJournal of Medical Case Reports 2011 5:20610.1186/1752-1947-5-20621615888 [Google Scholar] [CrossRef] [PubMed]
[5]. Saurez VR, Iannucci TA, Neurocysticercosis in pregnancy: A case initially diagnosed as eclampsiaObstet Gynecol 1999 93(5 Pt 2):816-18.10.1016/S0029-7844(98)00342-1 [Google Scholar] [CrossRef]
[6]. Padhy SK, Phuljhele S, Rathi A, Mandal S, Not just another diplopia: Neurocysticercosis in a postpartum womanBMJ Case Rep 2018 :bcr201822738810.1136/bcr-2018-22738830366900 [Google Scholar] [CrossRef] [PubMed]
[7]. Del Brutto OH, Nash TE, White AC Jr, Rajshekhar V, Wilkins PP, Singh G, Revised diagnostic criteria for neurocysticercosisJ Neurol Sci 2017 372:202-10.10.1016/j.jns.2016.11.04528017213 [Google Scholar] [CrossRef] [PubMed]
[8]. Nash T, Bartelt L, Korpe PS, Lopes B, Houpt ER, Case report: Calcified neurocysticercus, perilesional edema and histologic inflammationAm J Trop Med Hyg 2014 90:318-21.10.4269/ajtmh.13-058924394477 [Google Scholar] [CrossRef] [PubMed]
[9]. Nash T, Pretell EJ, Lescano AG, Bustos JA, Gilman RH, Gonzalez AE, Perilesional brain oedema and seizure activity in patients with calcified neurocysticercosis: A prospective cohort and nested case-control studyLancet Neurol 2008 7:1099-105.10.1016/S1474-4422(08)70243-6 [Google Scholar] [CrossRef]
[10]. Vargas-Villavicencio JA, Larralde C, De Leon-Nava MA, Morales-Montor J, Regulation of the immune response to cestode infection by progesterone is due to its metabolism to estradiolMicrobes Infect 2005 7:485-93.10.1016/j.micinf.2004.12.01515804489 [Google Scholar] [CrossRef] [PubMed]
[11]. Flisser A, Madrazo I, Plancarte A, Schantz P, Allan J, Craig P, Neurological symptoms in occult neurocysticercosis after single taeniacidal dose of praziquantelLancet 1993 342(8873):748 [Google Scholar]
[12]. Nash T, Edema surrounding calcified intracranial cysticerci: Clinical manifestations, natural history and treatmentPathogens Global Health 2012 106:275-79.10.1016/0140-6736(93)91743-6 [Google Scholar] [CrossRef]
[13]. Sheth T, Pillon L, Keystone J, Kucharczyk W, Persistent MR contrast enhancement of calcified neurocysticercosis lesionsAm J Neuroradiol 1998 19:79-82.10.1179/2047773212Y.000000002623265551 [Google Scholar] [CrossRef] [PubMed]
[14]. D’Cruz RF, Ng SM, Dassan P, Neurocysticercosis in pregnancy: Maternal and fetal outcomesOxf Med Case Reports 2016 2016(7):138-40.10.1093/omcr/omw01927471595 [Google Scholar] [CrossRef] [PubMed]
[15]. Saldanha V, Saldanha G, Reys RP, Benson CA, Noormahomed EV, Neurocysticercosis in child bearing women: An overlooked condition in mozambique and a potentially missed diagnosis in women presenting with eclampsiaEC Microbiol 2018 14(11):736-40.Epub 2018 Oct 29. PMID: 31681909; PMCID: PMC6824723 [Google Scholar]
[16]. Ramus RM, Girson M, Twickler DM, Wendel GD, Acute obstructive hydrocephalus due to cysticercosis during pregnancyInfect Dis Obstet Gynecol 1994 1(4):198-201.10.1155/S106474499400008618475345 [Google Scholar] [CrossRef] [PubMed]
[17]. Sahai S, Sahai A, Pica causing neurocysticercosis in pregnancy presenting as eclampsia: A report of two casesJ Obstet Gynaecol India 2013 63(1):68-69.Epub 2012 May 210.1007/s13224-012-0139-724431605 [Google Scholar] [CrossRef] [PubMed]