The ED often encounters patients in trauma complaining of severe pain with closed or compound fractures of long bones. Safe and effective pain control poses a challenge both to alleviate its severity and arrange remedial measures. In comparison to other long bones fractures, femur fractures are extremely painful due to the large muscle groups surrounding it and causing severe spasm. Pain management in patients with femur fractures is challenging during manipulation, application of splintage and shifting and positioning for radiological investigations. Any motion of the limb to arrange remedial measures triggers and aggravates the pain. It is imperative in ED to optimally manage and provide quick and effective remedies to facilitate desired analgesia in initial management of such cases. Reduction in pain decreases the anxiety and apprehension of the patient with the fracture. Quick pain relief and tranquil ambience enhance the confidence of the patient in emergency care and has positive influence on other neighbouring patients in waiting. Systemic analgesics (Opioids and Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)) and nerve blocks has been utilised for providing pain relief to patients with the fractured femur. Use of opioid medications and resultant poor pain control has been found to be associated with acute confusion states in the elderly and to certain extent in all others age groups [1]. It is well-established that any Procedural Sedation and Analgesia (PSA) has its own associated complications such as airway or circulatory compromise [2]. Moreover, it is totally uncertain that patients are with empty or full stomach which is of prime consideration in administration of conventional analgesics in emergency procedures. Also, it is imperative to add that patients, who receive PSA, would require close monitoring during and after the procedure for several hours which will be consuming disproportionately the trained medical man power in ED [2].
The FNB is an easy, fast, safe and effective means of providing pain relief to patients with fracture of the femur (neck femur, per-trochanteric femur, shaft femur or distal femur) with minimum amount of anaesthetic drugs [3-6]. After a successful block, the subsequent requirement of opioids or NSAIDS is considerably reduced. This helps in avoiding potential side effects such as nausea, vomiting, sedation, delirium and respiratory depression, and gastrointestinal side effects. These adverse effects are more noticeable in elderly patients and in patients with co-morbidities who may face one or many detrimental effects [6-8]. Several methods of the nerve block have been reported in literature. The traditional landmark-based technique of FNB is inherited with the risks of a “blind” procedure and may result in inadvertent arterial puncture on injection. Moreover, nerve stimulators are not readily available in the ED and its safe application requires additional training. Use of ultrasound guided nerve block has been advocated by Bhoi S et al., and it can improve the efficacy and safety of the FNB [2]. However, it is reported by several investigators that the utilisation of the FNB in the ED is low at 7% in Australia and 10% in the United Kingdom [9,10]. This has been attributed to the limited experience, inadequate training and infrequent clinical exposure of ultrasound based procedures amongst the doctors in the department. Ultrasonography with proper probe placement and choice of frequency facilitates the identification of relevant neurovascular-anatomical structures and continuous needle tip visualisation for guiding to the targeted nerve and region. This may even provide visualisation of spread of Local Anaesthetic (LA) for its effective concentration in desired topology. Ultrasound-guided FNB provides quick, safe, and effective acute pain relief and could therefore, be a valuable tool adding to current pain management regimes in ED [2,10]. This study was done with the purpose of establishing the efficacy of USG guided FNB in alleviating pain in fractures of the femur and its effect on patient anxiety.
Materials and Methods
This study was conducted at a tertiary care 1100 bedded multispecialty teaching hospital. This was a prospective interventional study conducted in the 30 bedded department of emergency medicine. The period of study was from January 2020 to June 2020. The study was undertaken after obtaining ethical clearance from the institute (IEC No.62/20). Prior to the start of study, a pilot study was conducted and the sample size determination was based on the previous studies [11,12]. The sample size was estimated on the basis of a single proportion design and the mean was calculated. The target population from which sample was randomly selected considered as 5,000. The present study assumed that the margin of error 11%, population proportion 50% and confidence level of 95%. The sample size actually obtained for this study was 79 patients. The actual number of patients enrolled was 84.
Inclusion criteria: Inclusion criteria for patients were all simple femur fracture patients (including proximal, mid shaft and distal), aged 20-70 years with haemodynamic stability.
Exclusion criteria: Pregnant patients, extremes of age (<20 years, >70 years), haemorrhagic diasthesis, polytrauma patients, segmental fractures, open fractures, patients with cardiac and respiratory instability, patients with the major life threatening co-morbidities, hypersensitivity to amide LA and patients with local pathology in the femoral triangle.
Study Procedure
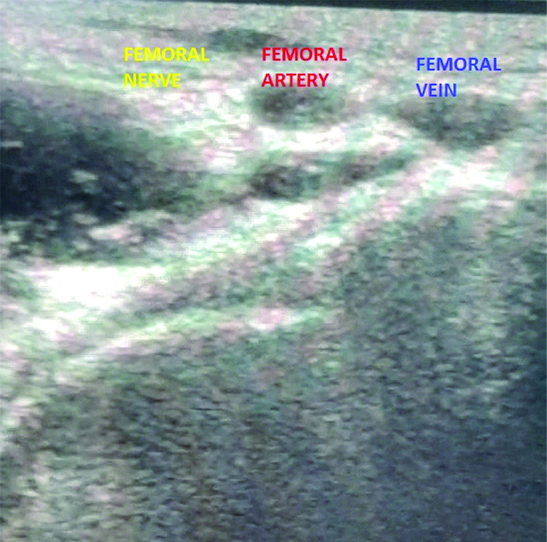
All trauma patients who fulfilled inclusion criteria within six months period were included. The present study divided all the fractures into two major groups, fractures around the hip (Neck of Femur (NOF) fractures and Trochanteric fractures) and fractures of the shaft (Shaft of Femur (SOF) fractures and Distal Femur (DF) fractures). Patients once received in the ambulance bay were triaged by the emergency team and shifted to the emergency bay. Primary survey and secondary survey along with resuscitation measures and primary management was instituted as per Advanced Trauma Life Support (ATLS) guidelines and specific injury. Epidemiological data were collected including age, sex, etc. Simultaneously Visual Analogue Scale (VAS) [13] pain scale and Hamilton Anxiety Score (HAM-A) [14] were recorded. The patient was asked to subjectively state regarding ease and comfort during shifting and orthopaedic manipulations as poor or satisfactory, when immediately shifting to trauma bay at arrival. The VAS score is determined by measuring the distance (mm) on the 100 mm line between the “no pain” mark and the patient’s mark, providing a range of scores from 0-100. Patients usually describe their pain as none, mild, moderate, or severe. To replicate this, the following cut points have been recommended: no pain (0-4 mm), mild pain (5-44 mm), moderate pain (45-74 mm), and severe pain (75-100 mm) [13]. The HAM-A score measures the anxiety level, and is commonly used in clinical and research settings. The scale has 14 questions; and measures both mental and physical anxiety. Each item is scored on a scale of 0 (not present) to 4 (severe), with a total score range of 0-56. A <17 shows mild severity, 18-24 shows mild to moderate severity and 25-30 shows moderate to severe [14]. Patients who fulfilled inclusion requirements underwent ultrasound guided FNB under LA on the same gurney by the emergency physician after adequate consent. Patients were explained regarding procedure and informed written consent was obtained. Ultrasound guided FNB was given as described below: Patient was placed in supine position with the affected side in neutral position. Under aseptic precaution, a linear transducer (6-13 MHz, Sonosite Edge) was placed along the inguinal crease. Femoral artery was identified and nerve seen as hyperechoic oval or triangular structure just lateral to the artery [Table/Fig-1]. In case of poor visibility, transducer was tilted proximally or distally to identify the nerve. Ropivacaine 0.5% was used as LA. A skin wheal of LA was made 1 cm away from the lateral edge of the transducer. A 22 gauge spinal needle was inserted in plane in lateral to medial orientation, and advanced towards femoral nerve. Once needle tip was adjacent to nerve, 1-2 mL of drug was injected to confirm correct placement. A total 15 mL of drug was given in small aliquots and nerve was seen separating from the artery. VAS scoring was done postprocedure at 20 minutes before shifting the patient for radiology. The orthopaedic surgeon performed reduction and splintage in the procedure room after radiographs were obtained. VAS score and HAM-A scale was repeated 4 hours after block, when the patient was settled in the orthopaedic ward. Data of patients requiring additional doses of systemic analgesics within 4 hours of the block were not considered for evaluation.
Ultrasonographic visualisation of femoral nerve.
Statistical Analysis
All data was entered into excel sheets and tabulated. Statistical analysis of the data was done using Statistical Package For The Social Sciences (SPSS) version 21.0. The p≤0.05 considered with 95% Confidence Interval (CI) in the study. The difference in mean values, and chi-square test was utilised for categorical data. Paired t-test and independent student t-test was applied to compare the preoperative and postoperative VAS and HAM anxiety score. Significant difference was accepted at p≤0.05.
Results
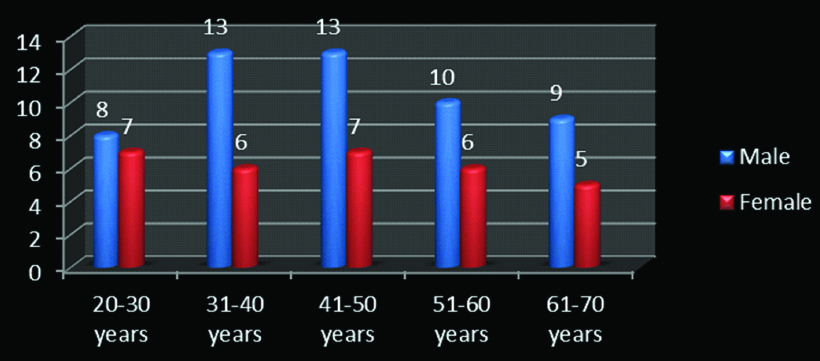
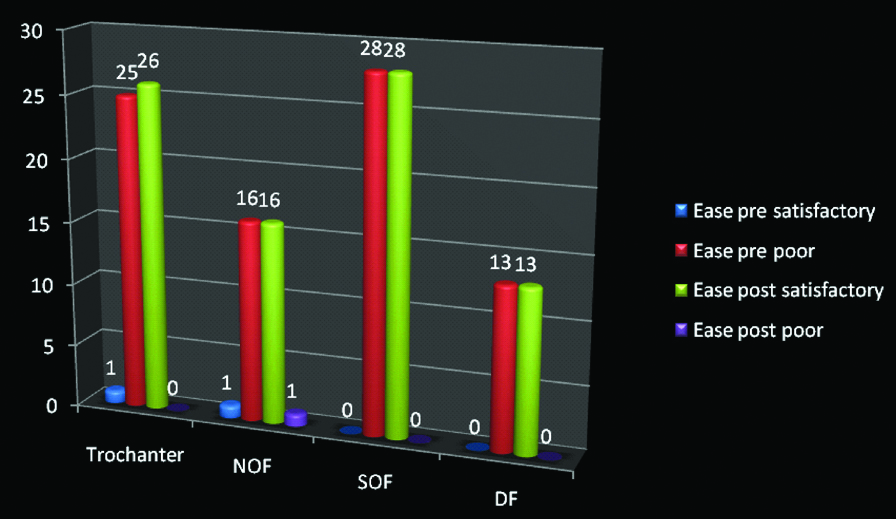
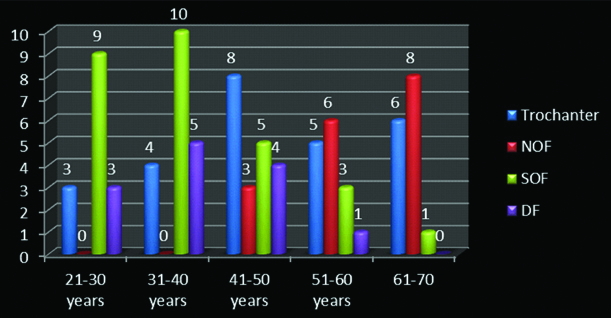
The total number of participants in present study was 84 with mean age of 44.98±13.82 years and 63.1% (n=53) were males and 36.9 % (n=31) were females. Maximum age was 69 years and minimum was 22 years. The p=0.532 showed statistically non-significant difference in age and gender distribution which means that the study population was homogeneous [Table/Fig-2,3]. Ease of handling and shifting as subjectively expressed by the patient was found to be poor preblock in almost all cases and satisfactory in all patients postblock [Table/Fig-4]. Shaft of femur and distal femur fractures were mainly seen in the younger age group while fractures around the hip were commonly seen in the elderly [Table/Fig-5]. The mean±SD VAS score preoperatively was 72.93±10.91. At 30 minutes and 4 hours postblock, the mean±SD VAS scores were 18.65±5.25 and 13.88±6.05, respectively. There was statistically significant difference in VAS score at 30 minutes (p=0.004) and 4 hours (p=0.015). Thus, there was a marked relief in pain postblock [Table/Fig-6]. On comparison of VAS scores among the two major fracture groups (fractures around the hip and fractures of the shaft) there was statistically significant difference (p=0.0031) in the pre-operative period with more pain in femur shaft fracture group as compared to fractures around the hip. There was statistically non-significant difference between the two groups at 30 minutes (p=0.126) and 4 hours (p=0.214) postblock. This signifies that the femoral block was equally effective in pain relief in both the groups [Table/Fig-6].
Demographic details of the study population.
| Demographic | N | Mean±SD | Maximum | Minimum |
|---|
| Age (Years) | 84 | 44.98±13.82 | 69 | 22 |
| Sex | Males (%) 53 (63.1%) | Females (%) 31 (36.9%) |
SD: Standard deviation
Distribution of study population according to age and gender.
Ease of patient handling and shifting (Subjectively answered by Patient) preblock and postblock according to site of fracture.
Comparison of fracture site with age.
SOF cases are more in age groups 21-30 and 31-40 years. There are no NOF cases in age groups 21-30 and 31-40 years. NOF cases are more in age group 61-70 and 51-60 years age groups. Trochanter fracture cases are more in age group 41-50 years age group; NOF: Neck of femur; SOF: Shaft of femur; DF: Distal femur
Clinical outcomes for VAS scores overall and intergroup comparison preoperative and postoperative.
| Clinical outcomes for VAS scores overall preoperative and postoperative |
|---|
| VAS score | Mean±SD | SEM | t | df | p-value |
|---|
| VAS preoperative | 72.93±10.91 | 1.19 | 61.21 | 83 | 0.004 |
| VAS 30 min | 18.65±5.25 | 0.574 | 32.42 |
| VAS 4 hour | 13.88±6.05 | 0.661 | 20.92 | 0.015 |
| Intergroup comparison of VAS scores with Trochanter+NOF (hip) and SOF+DF (shaft) fracture |
| VAS Score | N | Mean±SD | SEM | t | df | p-value |
| VAS preoperative hip | 43 | 66.95±11.52 | 1.75 | 38.08 | 42 | 0.0031 |
| VAS preoperative shaft | 41 | 79.19±5.39 | 0.84 | 94.07 |
| VAS 30 min Hip | 43 | 19.67±5.28 | 0.805 | 20.64 | 0.126 |
| VAS 30 min Shaft | 41 | 20.73±4.4 | 0.689 | 30.02 |
| VAS 4 hour Hip | 43 | 14.02±6.85 | 1.045 | 11.46 | 40 | 0.214 |
| VAS 4 hour Shaft | 41 | 15.83±4.39 | 0.686 | 23.01 |
SD: Standard deviation; SEM: Standard error of mean; df: Degree of freedom; t: Independent t test; NOF: Neck of femur; SOF: Shaft of femur; DF: Distal femur; VAS: Visual analog scale; Significant difference p<0.05
The mean Hamilton Anxiety score at preblock and 4 hour postblock was 27.05±5.94 and 8.07±3.7, respectively. The overall HAM-A score comparison showed that there was statistically significant change after 4 hours postblock (p=0.013) meaning that there was significant reduction in patients anxiety level. Comparison of intergroup HAM-A scores showed a statistically non-significant difference, indicating that FNB was equally effective in decreasing patient anxiety in both groups [Table/Fig-7].
Clinical outcomes for HAM scores on overall and intergroup comparison.
| Clinical outcomes for HAM scores on overall comparison with preoperative and postoperative |
|---|
| HAM score | Mean±SD | SEM | r | t | df | p-value |
|---|
| HAM preoperative | 27.05±5.94 | 0.649 | 0.442 | - | 83 | 0.353 |
| HAM 4 hour | 8.07±3.7 | 0.404 | - | 19.84 | 0.013 |
| Intergroup comparison of HAM scores with Trochanter+NOF (fractures around hip) and SOF+DF (fractures of femur shaft) preoperative and postoperative |
| HAM score | N | Mean±SD | SEM | t | df | p-value |
| HAM preoperative hip | 43 | 27.07±7.64 | 1.16 | 23.17 | 42 | 0.345 |
| HAM preoperative shaft | 41 | 27.02±3.46 | 0.54 | 49.91 |
| HAM 4 hour hip | 43 | 8.35±4.45 | 0.674 | 12.214 | 40 | 0.654 |
| HAM 4 hour shaft | 41 | 7.78±2.73 | 0.427 | 18.101 |
r: Karl Pearson correlation coefficient; NOF: Neck of femur; SOF: Shaft of femur; DF: Distal femur; VAS: Visual analog scale; HAM: Hamilton anxiety score; Significant difference p<0.05
Discussion
Ultrasound-guided FNB is a relatively new concept for pain management of fractures in the ED. This was traditionally done by anaesthetists in the operation theatre for procedural and postprocedural analgesia [2]. There are multiple advantages of this technique when used in ED, like avoidance of procedural sedation, reducing length of stay, avoiding the need for patient monitoring and decreasing the side-effects of systemic analgesics and sedatives. This procedure is extremely effective and provides adequate and prompt pain relief and has no lag period like systemic analgesics. Procedural analgesia and sedation involves long term fasting, a monitored bed in the ED, time for preparation of drugs, and risks of deep sedation like aspiration and airway compromise. In addition, co-existing traumatic conditions such as head injury and shock and co-morbid conditions make the use of procedural sedation unacceptable [15]. Ultrasound guided nerve blocks are very accurate with rate of block success being almost 95% [16].
In present study population, age and sex distribution was homogenous. The impact of factors such as age and gender on pain reduction score and anxiety was not found to be statistically significant. The present study also analysed the subjective comfort (Answered by the patient) of the patient pre and postnerve block and found that all patients were satisfied by the pain relief. This subjective assessment of patient comfort, ease of handling and shifting has not been done in recent literature. The present study used the VAS pain score in analysis of pain pre and postblock. The analyses revealed that patients with fractures around the hip had less pain than fractures of the shaft femur and distal femur after trauma. This may be explained by the fact that muscle forces acting in the shaft femur after a fracture are extremely high causing migration of fragments and severe spasm leading to intense pain. However, in fractures around the hip especially in neck of femur fractures muscle forces are less and being peri-capsular, the capsule also provided some sort of stability which leads to lesser pain. In the postblock period VAS score both at 30 minutes and 4 hours was significantly reduced showing appreciable pain relief in all subjects. However, on doing an intergroup analysis for postblock VAS scores at 30 minutes and 4 hours between fractures around the hip and fractures of the shaft femur did not reveal significant difference thus pointing to the fact that FNB was equally effective in pain relief in all fractures of the femur, including fractures around the hip, fractures of the shaft and fractures of the distal femur. In general, the periosteum of deep bones like femur derives its nerve supply from the nerves of the motor branches to nearby muscle [17]. Femoral nerve supplies the quadriceps muscle and also the periosteum of the femoral shaft [8]. Hence, FNB may also reduce the periosteal pain in fractures of the shaft femur apart from fractures around the hip where it has direct supply. Decrease in pain scores after FNB is similar to studies by Schiferer A et al., and Capdevila X et al., who reported decrease in pain scores, blood pressure and heart rate after administration of block [18,19]. However, none of the previous studies have done a comparative analysis of pain relief between various sites of fractures in the femur after block. This is unique to this study and shows a very important observation regarding comparable benefit of this nerve block at all fracture femur sites. The present study have considered an anxiety component after trauma. The Hamilton Anxiety score was used preblock and 4 hours postblock to assess the patient’s mental status. This correlation of trauma and pain with anxiety and effect of block in reducing this, is unique to present study. Three results were identified by search [20-22]; however amongst these no studies about anxiety level in fracture patients undergoing FNB was identified in the accompanying abstract or full-text publication. There was significant decrease in anxiety levels after block in both the fracture groups. This can be explained by the fact that block reduces pain and hence makes the orthopaedic surgeons job of reduction and splinting easier. Also, the patient is transported to radiology and to ward comfortably. Usually by 4 hours, a final treatment plan is made and communicated to the patient. This also adds significantly to the decrease in anxiety.
Limitation(s)
The present study has few limitations like small sample size and lack of control group. Randomised controlled trials (RCTs) with large number of participants are necessary in future to prove the exact efficacy of this procedure.
Conclusion(s)
In present study, FNB provided rapid and prolonged analgesia with comfort in patients with fracture around the hip, shaft femur and distal femur fractures. The analgesic effect and the quadriceps palsy allow muscle relaxation and hence pain-free radiology and orthopaedic tractions and splinting. Also, decreasing the pain immediately on arrival and performing transport, radiology and orthopaedic procedures with minimal pain has positive impact on the patient’s anxiety. Thus, the present study can safely conclude that FNB is a safe approach in providing rapid and effective analgesia in fractures around the hip and fractures of the shaft femur while decreasing the side effects of PSA. The present study also recommend that FNB should be included as the part of primary treatment for patients suffering from fracture shaft femur or fractures around the hip in an emergency ward.
Contribution of Authors: Review concept, Review design, Literature search and article writing by SST, SA and SM. Supervision by SST, AA and SM; Materials by SM, AA and SA; Critical review by SST, SM, SA and SA; Article editing by SST, SM, AA and SA and Final approval by SST, SA and SM.
SD: Standard deviation
SD: Standard deviation; SEM: Standard error of mean; df: Degree of freedom; t: Independent t test; NOF: Neck of femur; SOF: Shaft of femur; DF: Distal femur; VAS: Visual analog scale; Significant difference p<0.05
r: Karl Pearson correlation coefficient; NOF: Neck of femur; SOF: Shaft of femur; DF: Distal femur; VAS: Visual analog scale; HAM: Hamilton anxiety score; Significant difference p<0.05