Unique Case of Mediastinal Teratoma with Unusual Components
Anand Deodhar1, Dinesh Kulkarni2
1 Consultant Cardiovasular and Thoracic Surgeon, Department of CVTS, United CIIGMA Hospital, Aurangabad, Maharashtra, India.
2 Consultant Histopathologist, Department of Histopathology, Saurabh Eye Care and Histopathology Centre, Aurangabad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dinesh Kulkarni, Consultant Histopathologist, Department of Histopathology, Saurabh Eye Care and Histopathology Centre, Aurangabad, Maharashtra, India.
E-mail: drdineshkulkarni@gmail.com
Mature teratoma is a benign, slow growing tumour. It usually affect adults in 20-40 years of age. Teratomas with mature pancreatic tissue are extremely rare. There are only a few cases of teratoma containing mature pancreatic tissue that have been reported in literature. Authors report a case of a 25-year-old male having a large solid cystic anterior mediastinal mass, which on excision, histologically revealed large areas of mature pancreatic tissue along with squamous epithelium with sebaceous glands and keratin, pseudostratified columnar ciliated epithelium, mucin secreting glands, cartilage, pigment and other germ cell derived mature elements. This is a unique case with unusual microscopic findings in the form of predominant pancreatic and also brain tissue along with other elements.
Anterior mediastinum, Benign, Pancreatic tissue
Case Report
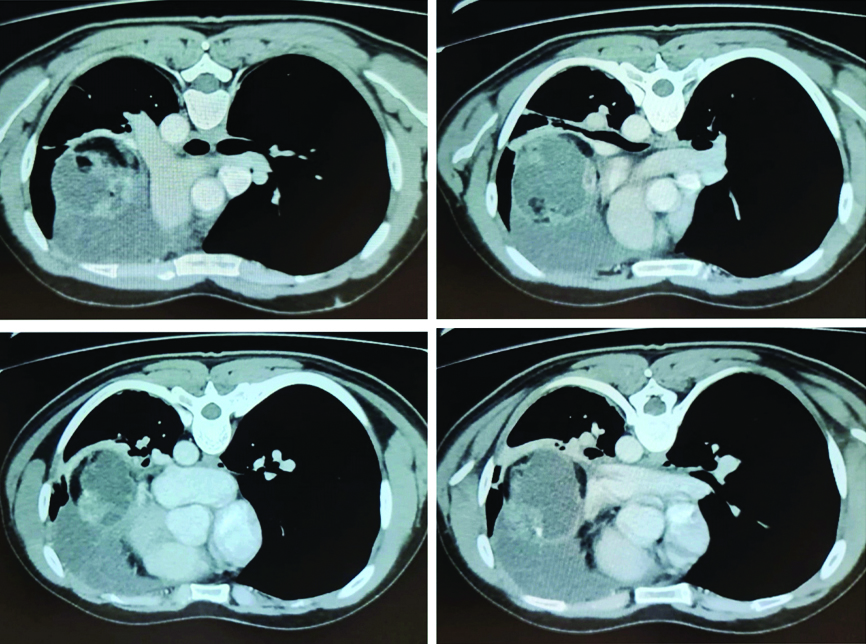
A 25-year-old male was referred from outside for excision of mediastinal mass. On examination he was a young man, averagely built with pulse, blood pressure within normal limits. His Contrast Enhanced Computed Tomography (CECT) Thorax revealed a large 11×8×12.5 cm well-demarcated anterior mediastinal mass showing heterogenous enhancing soft tissue component and peripherally enhancing cystic areas with foci of calcification and fat. Mediastinal vessels were normal. There was no evidence of mediastinal lymphadenopathy. Trachea and both bronchi were normal. Pleura, bony cage and soft tissue of chest wall were normal. A diagnosis of mediastinal teratoma was made [Table/Fig-1].
Laboratory reports in the form of Complete Blood Count (CBC), Liver Function Test (LFT), Kidney Function Test (KFT), urine were within normal limits. His blood group was O positive. He was tested negative for HBsAg, HCV and HIV. The Electrocardiogram (ECG) and 2D Echocardiography (2D ECHO) findings were also within normal limits.
After proper preanaesthetic evaluation, (left) thoracotomy was planned for removal of mass. Under General Anaesthesia (GA) (left) lateral thoracotomy was done from 5th intercostal space. Intraoperatively a large mass was detected in anterolateral mediastinum which was adherent to lingular and upper lobe of (left) lung and also pericardium. Left phrenic nerve was pushed laterally and stretched by tumour mass. Left lung was separated from the mass. The partially solid and cystic mass was excised in totol and was sent for histopathological examination. No blood transfusion was required. The postoperative period was uneventful and was discharged on 7th postoperative day. The patient is under regular follow-up.
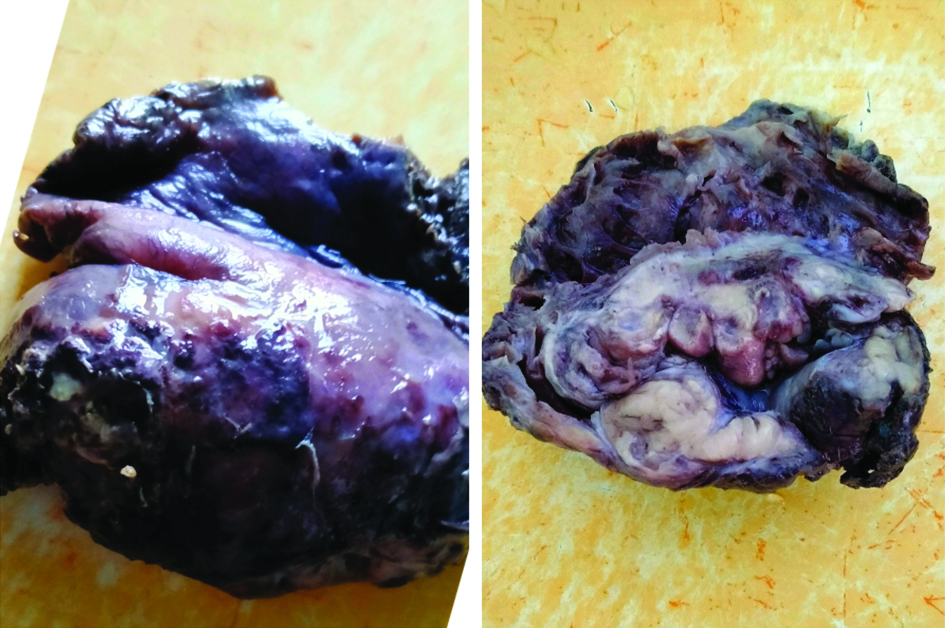
Histopathology findings: Gross examination of the specimen revealed a single oval mass measuring 13×12×8 cm, well-circumscribed, grayish, soft to firm at places. Cut surface was solid and cystic with thick wall and cystic portion showed small cystic spaces [Table/Fig-2].
Gross and cut surface of mediastinal mass.
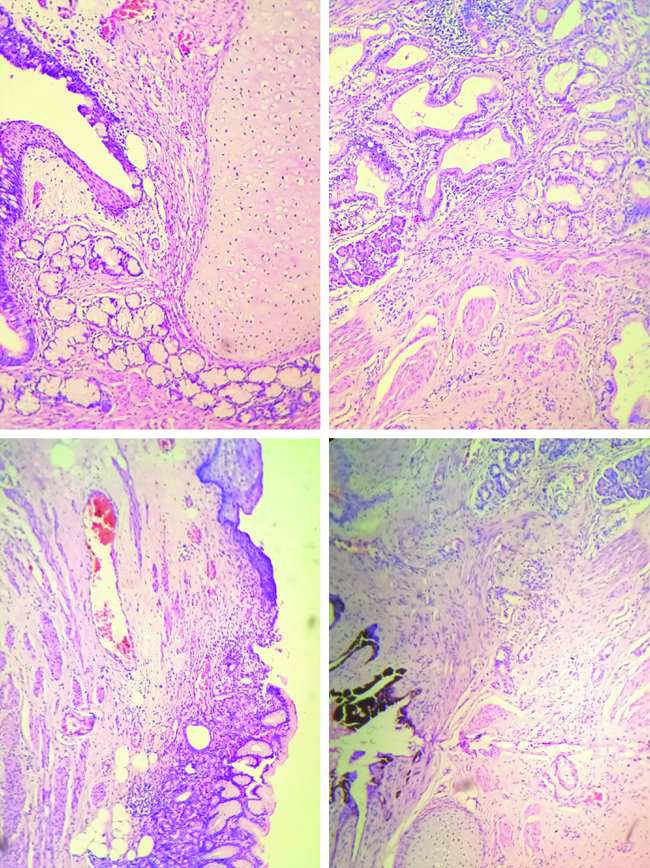
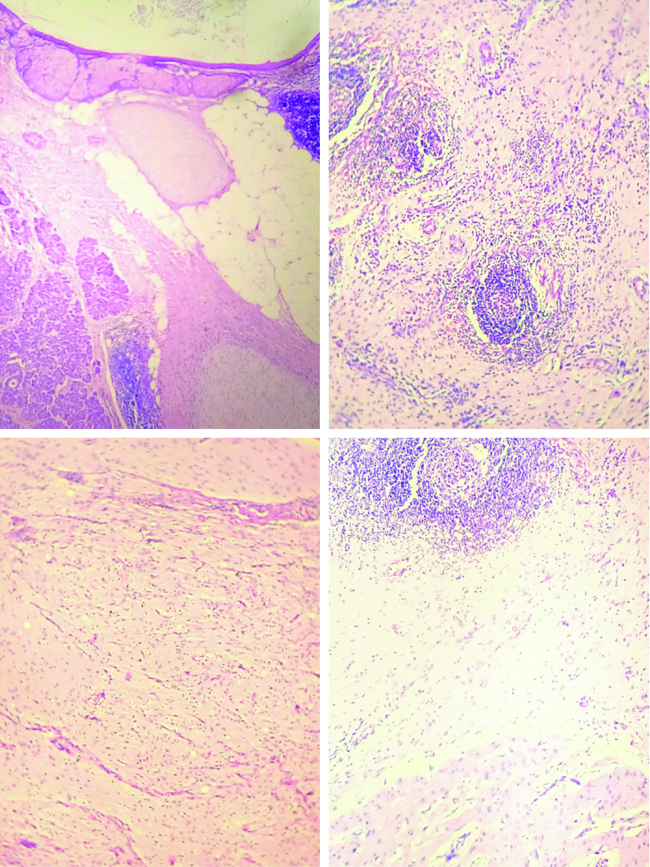
Sections from solid areas, microscopically revealed pseudostratified columnar ciliated respiratory epithelium and squamous metaplasia at places and mucin secreting glands, pigment and cartilage [Table/Fig-3]. Pancreatic acini and ducts, fat, smooth muscles, glands and cartilage were seen with abundance of pancreatic tissue [Table/Fig-4]. Squamous epithelium with adnexal tissue, fat, cartilage, lymphoid follicles, thymic tissue and brain tissue were identified [Table/Fig-5]. The stroma was fibrocollagenous with dense collection of lymphocytes and histiocytes. No nuclear atypia seen. No capsular invasion seen. The sections from cystic area showed fibrous tissue.
Reveals pseudostratified columnar ciliated respiratory epithelium and squamous metaplasia at places and mucin secreting glands, pigment and cartilage (H&E 100X).
Pancreatic acini and ducts, fat, smooth muscles, glands and cartilage (H&E, 100X).
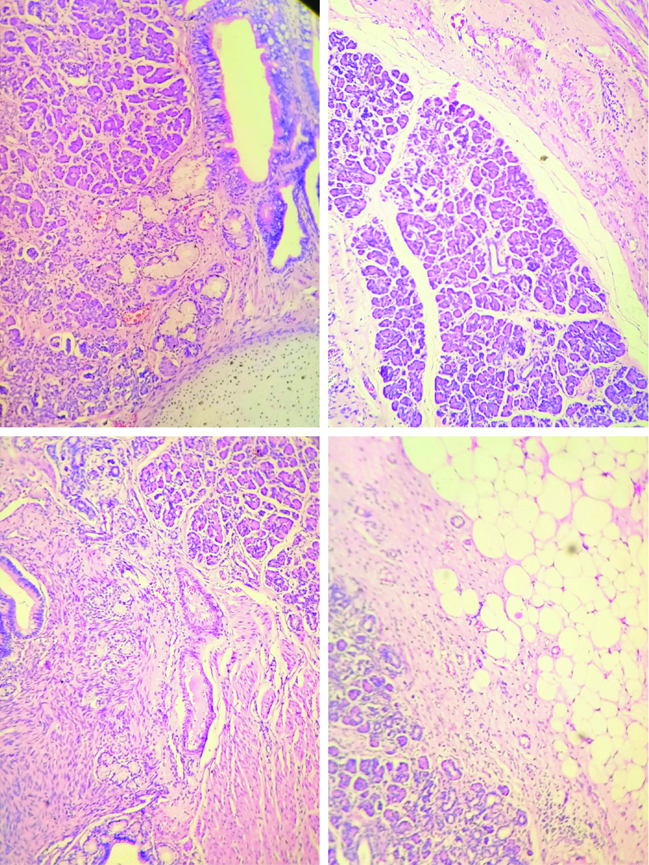
Squamous epithelium with adnexal tissue, fat, cartilage, lymphoid follicles, thymic tissue and brain tissue (H&E, 100X).
Hence, a final diagnosis of mature teratoma with predominant pancreatic tissue was made.
Discussion
The mediastinum contains a range of variable tissue in the body and hence tumours in this area therefore, can represent many different clinical entities and pathologic processes. An understanding of embryology and anatomic relations to the structures around, is essential in proper determination of the exact nature of tumour [1].
Teratomas create an interest in pathologists with their varying features and puzzling pathogenesis [1]. Primary Germ Cell Tumours (GCT) of mediastinum are rare tumours (10-15%) and usually present in third to fourth decade. GCTs are predominantly found in gonads and most common extragonadal site is anterior mediastinum [2]. Most of teratomas in mediastinum are well-demarcated, grow slowly and are benign histologically. Less than 1% are malignant. Benign cystic teratomas may contain pancreatic tissue in larger amount and is a particularly common finding in mediastinal and sacrococcygeal region. The tissues found in benign teratomas are well-formed and usually considered to be mature by conventional microscopy, although may be arranged haphazardly [3].
Mature teratomas are the tumours of young adults in their third decade with no gender predilection. There is no definite pathogenesis for the development of teratomas. These tumours consist of primordial germ cells which drift into the extragonadal midline structures during migration while undergoing embryonic development. Most of the mediastinal teratomas are accidentally detected during chest X-ray examination. Many of them are clinically asymptomatic, but some may present with chest, back or shoulder pain, dyspnea, fever, pleural effusion and bulging of chest wall. Less commonly they may become infected or rupture into surrounding tissue like lung, bronchial tree or pleural and pericardial cavity. Symptoms can also be because of pressure causing vena caval syndrome. Surgical excision is the treatment of choice and complete recovery is the outcome [4].
It was found that squamous epithelium with adnexae, mucin secreting glands, respiratory epithelium and cartilage were detected in almost all cases. Lymphoid tissue was also detected in few of the cases. Pancreas and brain tissue were very rarely encountered. All these elements were seen in present case.
Conclusion(s)
Mediastinal teratomas are usually solid cystic, detected in young patients by CT scans. For pure mature teratomas, surgical excision is the treatment of choice. Histologically, with usual components, unusual components can be expected.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 23, 2020
Manual Googling: Feb 02, 2021
iThenticate Software: Mar 02, 2021 (8%)
[1]. Mueller DK, Teratomas and other germ cell tumours of mediastinumMedscape 2019 [Google Scholar]
[2]. Dunn PJ, Pancreatic endocrine tissue in benign mediastinalteratomaJ Clin Path 1984 37(10):1105-09.10.1136/jcp.37.10.11056149236 [Google Scholar] [CrossRef] [PubMed]
[3]. Stella F, Davoli F, Giant mediastinal mature teratoma with increased exocrinepancreatic activity presenting in a young woman: A case reportJ Med Case Reports 2011 5:23810.1186/1752-1947-5-23821703035 [Google Scholar] [CrossRef] [PubMed]
[4]. Agrawal T, Blau AJ, Chwals WJ, Tischler AS, A unique case of mediastinalteratoma with mature pancreatic tissue, nesidioblastosis and aberrant islet celldifferentiation: A case report and literature reviewEndocr Pathol 2016 27(1):21-24.10.1007/s12022-015-9393-426318442 [Google Scholar] [CrossRef] [PubMed]