Invasive Aspergillosis of Right Maxillary Sinus with Orbital Extension in an Immunocompetent Individual
Sachin Daigavane1, Madhumita Prasad2, Sana Beg3, Jigna Motwani4
1 Professor, Department of Ophthalmology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi (M), Wardha, Maharashtra, India.
2 Registrar, Department of Ophthalmology, Sankaraeye Centre, Indore, Madhya Pradesh, India.
3 Senior Resident, Department of Ophthalmology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi (M), Wardha, Maharashtra, India.
4 Junior Resident, Department of Ophthalmology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi (M), Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Jigna Motwani, B904, Fantasia, Raheja Gardens, LBS Marg, Thane, Maharashtra, India.
E-mail: jignamotwani04@gmail.com
Secondary involvement of orbit in aspergillosis following paranasal sinus fungal infection is rare. A case of invasive aspergillosis of right maxillary sinus in a 31-year-old immunocompetent male patient was referred to Ophthalmology OPD with unilateral proptosis. Patient developed proptosis in right eye since six months, which was insidious in onset, progressive, not associated with painful movements. It showed regression since last one month. On examination, best corrected visual acuity was 6/12 in right eye with light projection accurate in all quadrants on presentation, with progressive diminution of vision over 15 days, normal colour vision, pupil was normal in size, reacting to light. Extraocular movements were reduced on lateral side. Left eye examination was within normal limit. Magnetic resonance imaging showed involvement of intra and extraconal compartment upto apex of orbit of right eye, pushing optic nerve medially, with erosion of lamina papyrecea. Intravenous amphotericin B was started and functional endoscopic sinus surgery with maxillary sinus debridement was done. Regular follow-up was kept to prevent the optic nerve involvement.
Fungal infection, Neuroaspergillosis, Proptosis
Case Report
A 31-year-old male with ulcer in right upper jaw presented with unilateral proptosis. The patient was referred to Ophthalmology OPD with chief complaint of protrusion of right eyeball since six months, insidious in onset and gradually progressive. It was not associated with painful eye movements. There was relief in symptoms since the past one month with slight regression of the proptosis according to the patient. Diminution of vision was insidious in onset and gradually progressive in nature. There was no history of trauma in the recent past, no history of bilateral involvement, no history of throbbing sensation. Patient did not give any history of headache or diplopia. No history of weight loss, recurrent cough or fever, intake of thyroid medication, and jaundice was noted. There was no history of previous treatment taken by the patient. Patient did not give any history of surgery in the past.
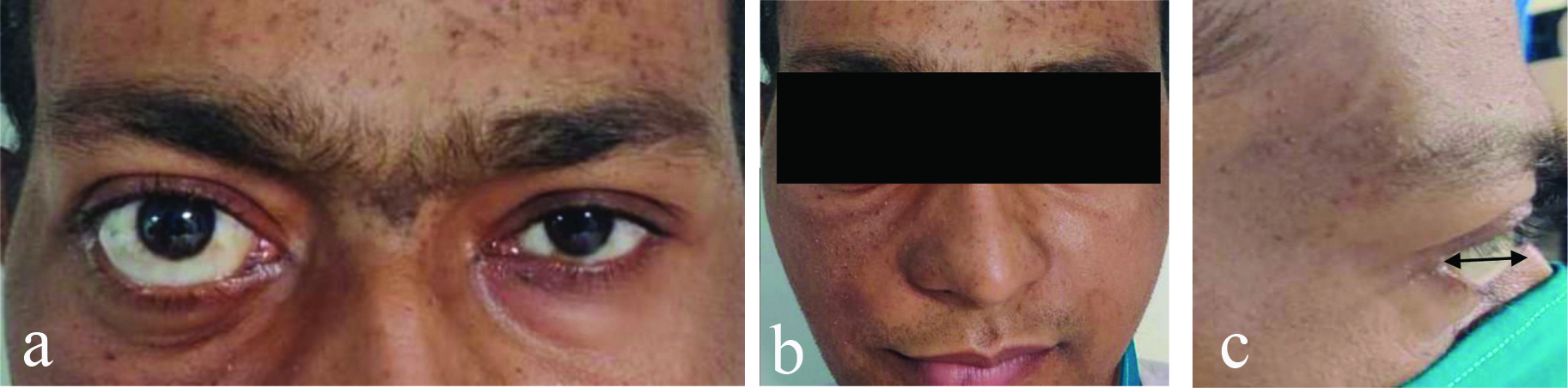
On examination of the face, it was grossly asymmetrical due to ulceration present on right side of palate extending from midline to 1 cm posterior to the line perpendicular to outer canthus of eye anteroposteriorly and from outer canthus of eye to ala tragus of right side superoinferiorly [Table/Fig-1a,b]. The ulcer was firm in consistency, tender, approximately 5×4 cm in size, associated with restricted mouth opening at the temporomandibular junction, palapable submandibular lymph nodes measuring 0.5 cm, on the right side were also present. On ophthalmic examination, Hirshberg test was orthophoric. The best corrected visual acuity was 6/12 by the snellen’s visual acuity chart, with N6 near vision, normal colour vision and normal confrontation test in the right eye. The patient had mild vertical orbital dystopia which was 12 mm when measured with a plastic ruler resting at the right lateral orbital margin parallel to the ground as seen in [Table/Fig-1c]. On anterior segment examination, scleral show was present inferiorly. Pupil was normal in size and reacting to light. No relative afferent pupillary defect was seen. The lens findings were normal. Extraocular movements in the right eye were restricted on lateral side, however they were full on the medial side. The intraocular pressures were within normal limit in the involved eye. Amsler grid test had no abnormality detected. Diplopia charting was normal. On posterior segment examination, a clear media, the optic disc with all margins well-defined, a cup disc ratio of 0.3:1, no hyperaemia of the disc, normal blood vessels and normal macula with bright foveal reflex were seen. Gross tessellations were a positive fundus finding. The left eye examination was within normal limit. Gradual and progressive diminution of vision in right eye was noted in due course of 15 days upto 6/36 on snellen’s chart.
(a) Shows unilateral proptosis on the right side; b) Right side disfigured face; c) The black arrow showing exophthalmos measuring 12 mm.
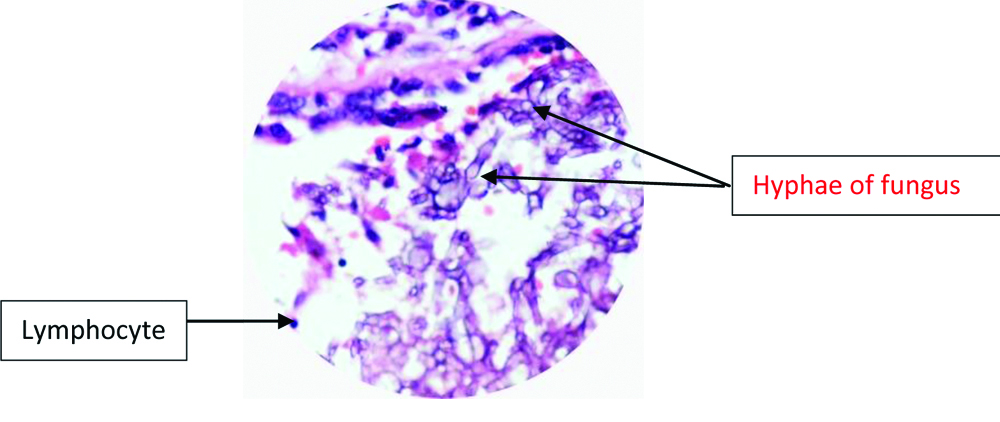
The patient was immunocompetent with no history of being on any drugs. His complete blood counts, liver and renal function tests, chest x-ray, blood glucose, and immunoglobulin levels were within normal limits. He was non-reactive to human immunodeficiency virus, hepatitis B and hepatitis C antigens. COVID antigen test was negative. His glycosylated haemoglobin value was normal. Thyroid function test was within normal limits. Magnetic resonance imaging [Table/Fig-2,3] showed an ill-defined non-enhancing soft tissue lesion arising from right maxillary sinus with extensive erosion and thinning of all walls of maxillary sinus. There was reported extension of the lesion into right nasal cavity, right masseter and temporalis muscles. In the orbit superiorly, the lesion involved intra and extraconal compartment of the right eye with complete encasement of the inferior and medial rectus muscles and partial encasement of lateral rectus muscle and optic nerve. It extended upto apex of the orbit, pushing the optic nerve medially. There was right sided proptosis and erosion of lamina papyraecea. There was also involvement of right frontal and ethmoid sinus. The lesion also had intracranial extension with abscess formation. Incisional biopsy was done from a right maxillary mass. Potassium hydroxide mount examination of biopsy taken from right maxillary mass showed septate, long, filamentous with acute angle branching fungal element suggestive of granulomatous lesion secondary to fungal infection, indicating of aspergillosis [Table/Fig-4].
a) The MRI image shows proptosis of right eye in the transverse section; b) T1 weighted MRI image shows medial displacement of optic nerve in the right eye.
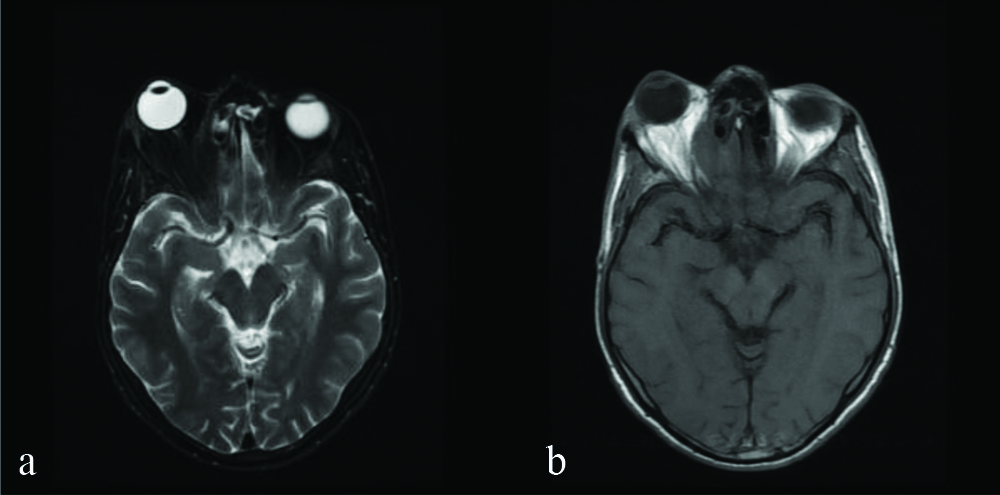
The T1 weighted MRI image shows destruction of the right maxillary sinus along with involvement of the floor of orbit and its extension into the orbital compartment.

A PAS stained histology specimen of 40×10 power (x) showing Aspergillus in the buccal mucosa.
PAS: Periodic acid-schiff
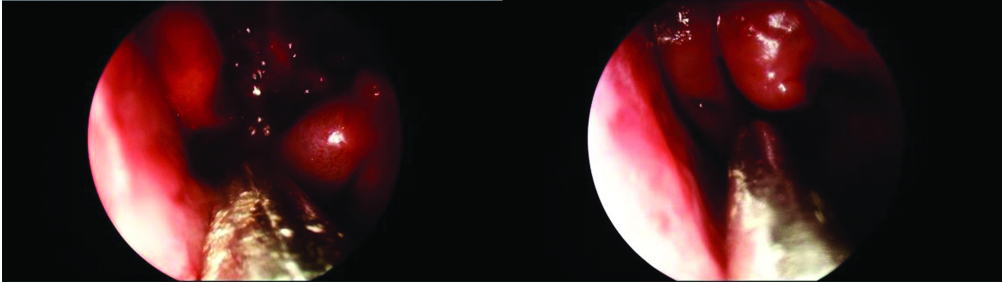
Therapeutic intervention: The patient was started on intravenous amphotericin B with the dose of 1 mg/kg and ocular follow-up was done. There was deterioration of vision during this course. A functional endoscopic sinus surgery was planned with the help of otorhinolaryngologists after one week of systemic antifungal treatment [Table/Fig-5]. Maxillary sinus debridement was done under all aseptic precautions under general anaesthesia. Postoperatively, patient was kept on antifungal and antibiotic cover to prevent further infection.
Debridement of fungal mass was done during endoscopic sinus surgery.
Follow-up: Patient was being followed for monitoring the severity of proptosis. On postoperative day one of follow-up, the proptosis was measured to be 10 mm, 2 mm lesser than the preoperative stage [Table/Fig-6]. On third follow-up, reduction in proptosis was further noted. The patient was continued on intravenous amphotericin B therapy along with a combination of piperacillin and tazobactam. Patient showed slight improvement in vision of upto 6/18 by snellen’s visual acuity chart over a longer follow-up of two months.
Shows the severity of proptosis to be reduced to 10 mm in the postoperative stage.

Discussion
There should always be a high suspicion for grave sino-fungal infections of the orbit to ensure early diagnosis and prompt management. The most common ones are mucormycosis and aspergillosis which frequently involve the sinuses as primary site of inoculation but may present with ocular symptoms [1]. The incidence of invasive sinus aspergillosis is 3.5 cases per 1000 person in immunocompromised individuals, however the disease is very rare in the immunocompetent [2]. Invasive aspergillosis of the orbit has very few reported cases in the past [3,4]. In healthy individuals, cases tend to occur in countries like India, Sudan and tropical areas which see a hot and humid temperature, favourable for fungal growth [5,6]. Orbital involvement in infection due to Aspergillus species has a poor prognosis. They are rapidly progressive and fatal opportunistic infections.
The age of presentation is generally younger age group. Decreased vision, proptosis, periorbital oedema, and complete external ophthalmoplegia are the most common ophthalmic features. Orbital involvement in a sinus fungal infection is through the spread from paranasal sinuses and thus, further risking contiguous spread through superior orbital fissure and optic canal into the middle cranial fossa. There has been documented risk of cerebrovascular disease as a complication of CNS aspergillosis [7]. These are more often fatal due to their intracranial extension. Early diagnosis and surgical intervention are required to improve vision and survival. Studies prove the effectiveness of combined approach of debulking with prolonged antifungal treatment [8]. The mechanism of action of antifungal agents is damaging the fungal cell wall membranes by acting on or inhibiting the synthesis of ergosterol. These include polyenes, azoles, echinocandins, pyrimidines, the most commonly used being intravenous or other forms of amphotericin B [9]. Surgical treatment involves radical extirpation of all involved paranasal sinuses. Orbital debridement depends on the extent of spread, the functional status of the eye and the response to medical therapy. The procedure is almost always adopted, but has no definitive reports of increased survival. Surgical debridement may not always be required though it has the benefit of reducing the fungal load and improving the delivery of antifungals. In the present case, the patient showed resolution of proptosis on immediate follow-up.
Conclusion(s)
This was a rapid progressive case of invasive fungal infection caused by Aspergillus involving the eye where early diagnosis followed by endoscopic sinus surgery was done and strict antifungal monitoring gave good results.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 10, 2020
Manual Googling: Feb 19, 2021
iThenticate Software: Mar 17, 2021 (11%)
[1]. Mukherjee B, Raichura ND, Alam MS, Fungal infections of the orbitIndian J Ophthalmol 2016 64:337-45.10.4103/0301-4738.18558827380972 [Google Scholar] [CrossRef] [PubMed]
[2]. Gupta V, Gupta A, Prevalence and clinical profile of patients with chronic fungal maxillary sinusitisInt J Otorhinolaryngol Head Neck Surg 2019 5:280-84.10.18203/issn.2454-5929.ijohns20190758 [Google Scholar] [CrossRef]
[3]. Dhiwakar M, Thakar A, Bahadur S, Invasive sino-orbital aspergillosis: Surgical decisions and dilemmasJ Laryngol Otol 2003 117(4):280-85.10.1258/0022215036060088712816217 [Google Scholar] [CrossRef] [PubMed]
[4]. Pushker N, Meel R, Kashyap S, Bajaj MS, Sen S, Invasive aspergillosis of orbit in immunocompetent patients: Treatment and outcomeOphthalmology 2011 118(9):1886-91.10.1016/j.ophtha.2011.01.05921665281 [Google Scholar] [CrossRef] [PubMed]
[5]. Hedges TR, Leung LS, Parasellar and orbital apex syndrome caused by aspergillosisNeurology 1976 26(2):117-20.10.1212/WNL.26.2.117943065 [Google Scholar] [CrossRef] [PubMed]
[6]. Green WR, Font RL, Zimmerman LE, Hayashi M, Tanaka K, Mizutani T, Aspergillosis of the orbit: Report of ten cases and review of the literatureArch Ophthalmol 1969 82(3):302-13.10.1001/archopht.1969.009900203040025806054 [Google Scholar] [CrossRef] [PubMed]
[7]. Ueki Y, Kazuta T, Naitou E, Hayashi M, Tanaka K, Mizutani T, A case of CNS aspergillosis developing orbital apex syndrome and causing mycotic aneurysm and the subsequent cerebral infarctionRinsho Shinkeigaku 2002 42(8):761-65. [Google Scholar]
[8]. Adulkar NG, Radhakrishnan S, Vidhya N, Kim U, Invasive sino-orbital fungal infections in immunocompetent patients: A clinico-pathological studyEye (Lond) 2019 33(6):988-94.10.1038/s41433-019-0358-630765886 [Google Scholar] [CrossRef] [PubMed]
[9]. Ghannoum MA, Rice LB, Antifungal agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistanceClin Microbiol Rev 1999 12(4):501-17.10.1128/CMR.12.4.50110515900 [Google Scholar] [CrossRef] [PubMed]