Splenic Hydatid Cyst- A Case Report
Leena Kumar1, Harshavardhan Balaganesan2, Sanjay Ballari3, Pooja Varwatte4, Meenal Jain5
1 Junior Resident, Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Chennai, Tamil Nadu, India.
2 Senior Resident, Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Chennai, Tamil Nadu, India.
3 Junior Resident, Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Chennai, Tamil Nadu, India.
4 Junior Resident, Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Chennai, Tamil Nadu, India.
5 Junior Resident, Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Leena Kumar, Junior Resident, Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Ammapettai, Nellikuppam, Chennai-603108, Tamil Nadu, India.
E-mail: leenakandeeban@gmail.com
Although involvement of spleen is rare in cases of hydatid disease, it should always be considered as a differential diagnosis for a cystic lesion in any of the solid organs, abdomen, lung or brain. The current case report is of a 60-year-old female patient who presented to Emergency Department with complaints of left upper quadrant pain which was continuous and dull aching. Ultrasound abdomen revealed a well-defined multicystic lesion with septations in spleen. Computed tomographic examination and magnetic resonance imaging confirmed the same and the lesion showed the characteristic T2 hypointense rim, consistent with hydatid disease. Splenectomy was performed for the patient and proved to be splenic hydatid cyst.
Computed tomography, Magnetic resonance imaging, Spleen, Utrasonography
Case Report
A 60-year-old female patient presented to the Emergency Department with complaints of abdominal pain for six months. The pain was confined to the upper left quadrant of the abdomen and was continuous and dull aching in nature and was not radiating or shifting. She had no history of vomiting, jaundice, cough or respiratory distress, diarrhoea/constipation. No fever, loss of weight or appetite. No previous history of abdominal trauma. On examination she was pale and afebrile, not icteric or cyanotic. Her Pulse Rate (PR) was 78/min and Blood Pressure (BP) was 130/90 mmHg. On systemic examination, her cardiac and respiratory systems were normal. Per abdominal examination revealed a soft abdomen with mild tenderness in left hypochondrium and epigastric region. A regular soft palpable mass was felt in the left hypochondrium which was moving with respiration. The mass was confined to left hypochondrium about 7-8 cms from left costal margin with no extension to other quadrants. No signs of guarding or rigidity was noted. Investigations like complete blood count, liver function tests, renal function tests and serology was carried out. The patient was found to be Hepatitis B surface antigen (Hbsg) positive. The patient was referred to the Radiology Department for further evaluation.
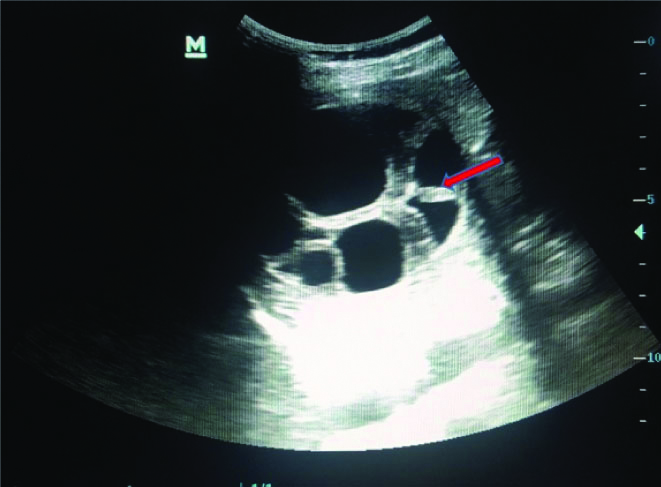
Ultrasonogram (USG) abdomen was done for the patient. USG abdomen revealed a well-defined multicystic lesion measuring 7.5×6.0 cms with thick internal septations in spleen [Table/Fig-1].
Transabdominal Ultrasonography (TAS) axial image showing a well-defined multiloculated anechoic cystic lesion with posterior acoustic enhancement and multiple thick internal septations (red arrow).
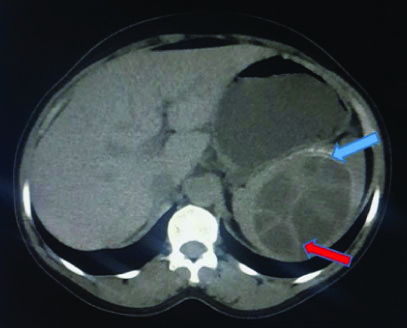
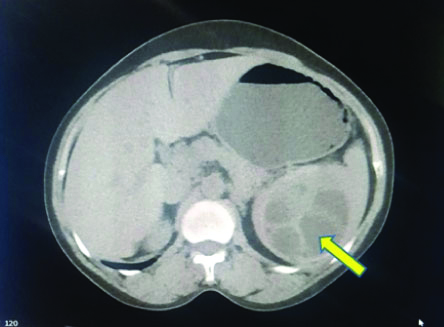
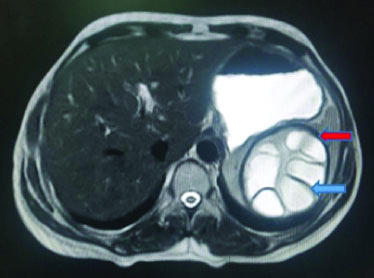
The patient was subjected for Computed Tomography (CT) examination. Non-enhanced CT (NECT) abdomen revealed a well-circumscribed oval hypodense multicystic lesion measuring 7.9×6.2 cms with internal septations showing the spoke wheel pattern in the substance of spleen. A thin focal rim of calcification was noted in the periphery of the lesion [Table/Fig-2,3]. Magnetic Resonance Imaging (MRI) was performed for the patient. T1 and T2 weighted MRI demonstrated a well-defined multicystic lesion with well-defined capsule and a hypointense rim on T2 which is characteristic of hydatid [Table/Fig-4,5]. Other abdominal organs were found to be normal. The differential diagnoses to be considered are as follows:
NECT abdomen (bone window) axial view showing a well-defined oval multicystic lesion with thick internal septations (red arrow) showing the spoke wheel pattern and eccentric peripheral rim calcification (blue arrow).
NECT: Non-enhanced computed tomography
NECT abdomen (soft tissue window) axial view on the right side showing the multicystic lesion with daughter cysts (yellow arrow).
Axial T2WI of abdomen showing a well-defined multilocular hyperintense cystic lesion with peripherally arranged cysts separated by hypointense septations (blue arrow) and a hypointense capsule (red arrow).
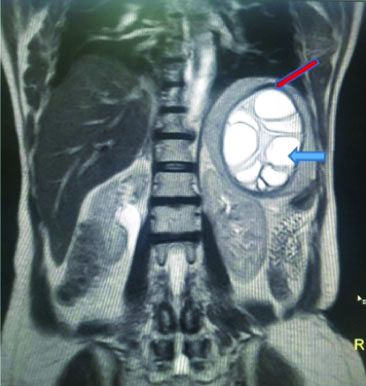
Coronal T2WI of abdomen showing a multilocular hyperintense cystic lesion (blue arrow) with hypointense septations and capsule (red arrow).
Epidermoid cyst of spleen: Cystic lesion with mobile echogenic debris.
Splenic abscess: Poorly demarcated with variable appearance ranging from hypoechoic to hyperechoic with internal septations.
Pseudocysts of spleen: Well-defined cystic lesion with heterogenous content due to internal echoes.
Haematoma: Sharply marginated with variable appearance.
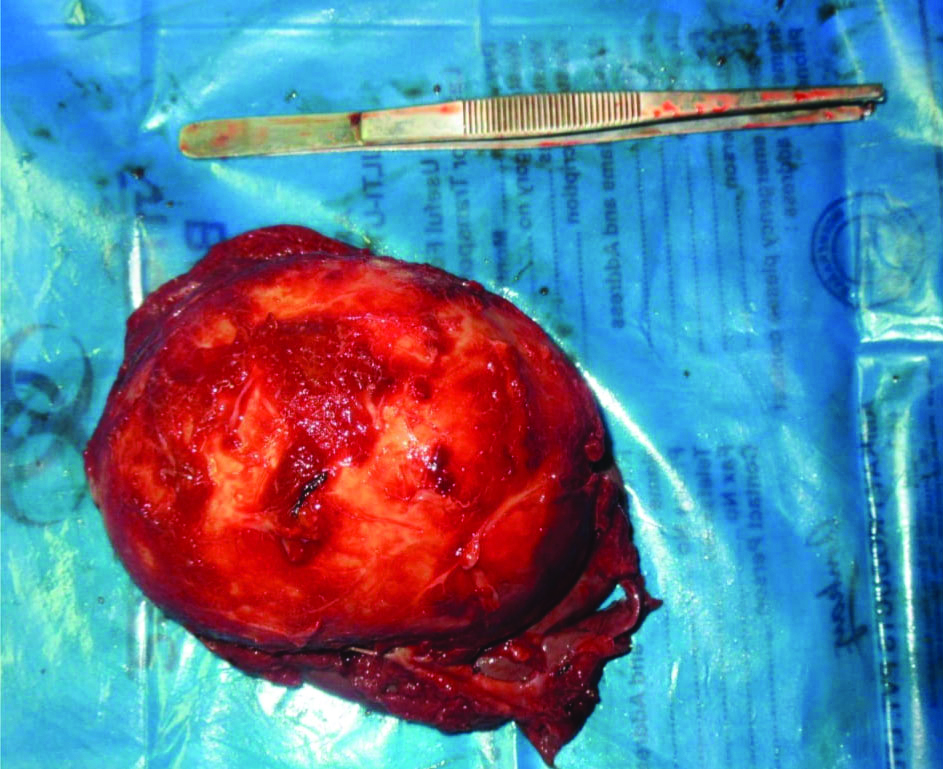
The provisional diagnosis of hydatid disease of spleen was given based on the above imaging findings. Open total splenectomy was performed for the patient with preoperative treatment with albendazole for 10 days. The postoperative period was uneventful. Gross splenectomy specimen [Table/Fig-6] measuring 10×7 cms and cut specimen of spleen showing multiple fluid-filled vesicles is shown in [Table/Fig-7]. It was proved to be hydatid cyst of spleen on histopathological examination.
Gross specimen of spleen.
Gross view of multiple fluid-filled vesicles on cut section of spleen.

Discussion
The word hydatid is of Greek origin and it means a drop of water. Hydatid disease is endemic in Middle East, India, Australia, South America, New Zealand [1]. Hydatid disease is a parasitic infestation by a tapeworm Echinococcus granulosus. Infestation with Echinococcus granulosus is prevalent especially in villages where sheep, dogs, and other cattles live in close contact with humans. Dogs and other members of canine family are the hosts of the parasite [2].
The definitive hosts are cattles and dogs whereas the humans are the accidental hosts because they are usually a dead end for the parasitic infection cycle. Humans may contract infection either by direct contact with dog or by ingestion of fluid or food contaminated with the faeces of dogs [3]. The most common organ affected by the parasite is the liver and the lungs followed by the other organs like kidney, brain and bones. The least common organs to be affected are the spleen, pancreas and the muscles. The splenic involvement represents 5% of cases [4].
The clinical presentation of the hydatid disease depends upon the position and the size of the hydatid cyst and also upon the accessibility of the organ for clinical examination. Radiography demonstrates the presence of calcification which is usually ring like or curvilinear representing peripheral pericyst calcification [5]. The other features seen are elevated left hemidiaphragm, displaced stomach bubble and left colon and reactive left pleural effusion. Ultrasonographic appearance of the hydatid cyst usually varies ranging from purely unilocular cystic lesion to solid appearing lesion. The detachment of endocyst membrane results in floating membranes within the pericyst that gives the water lily sign. Computed tomography is the investigation of choice and demonstrates the presence of unilocular to multilocular hypodense cystic lesion with peripheral calcification and contrast is not needed unless some complications like biliary communication or infection are suspected [6]. The hydatid cysts appears as a unilocular or multilocular T1 hypointense and T2 hyperintense lesion with hypointense septations. The characteristic appearance of hydatid disease in MRI is the presence of a hypointense rim on T2 weighted images due to presence of high amount of collagen in pericyst [7]. The differential diagnosis to be considered are in [Table/Fig-8] [8]. The ideal treatment of choice for splenic hydatid cyst is surgery because of the increased chances of rupture of cyst causing disseminated hydatidosis. The surgery of choice is either partial or total splenectomy depending on the extent of splenic parenchyma involved by the cystic disease [9]. The other treatment options available includes Percutaneous Aspiration Irrigation and Reaspiration (PAIR) where the cystic fluid is aspirated in order to decrease the pressure within the cyst [10]. Postoperative period should be followed-up with albendazole therapy. Albendazole is the mainstay of treatment in the postoperative follow-up period. Complication of hydatid cyst includes calcification, secondary infection, rupture of cyst with peritoneal seedling, systemic dissemination of the cysts.
Differential diagnosis to be considered.
| Diseases | Ultrasonogram | Computed tomography | Magnetic resonance imaging |
|---|
| Splenic hydatid | A smooth walled unilocular anechoic cyst or a complex cyst with multiple septations if daughter cysts are present. | Multiple vesicular cystic lesion with daughter cysts attached to the membrane of mother cyst with peripheral calcification of cyst wall. | The cyst appears T1 hpointense and T2 hyperintense with a T2 hypointense rim due to collagen rich pericyst. |
| Epidermoid cyst | Well-defined anechoic or hypoechoic lesion with internal echoes if debris is present. The cyst wall may show calcification and appears echogenic. | Well-defined hypoattenuating lesion with lack of enhancement on post contrast. Wall calcification may be present. | Appears hypointense on T1 and hyperintense on T2. |
| Splenic abscess | Poorly demarcated hypoechoic lesions with low level internal echoes. It contains multiple internal septations of variable thickness. The presence of gas bubbles may show reverberation artifacts. | A fairly defined centrally hypoattenuating lesion with average of 20-40 HU.It shows peripheral rim enhancement of capsule on contrast. | Appears hypointense on T1 and hyperintense on T2 with peripheral enhancement of capsule. |
| Pseudocyst of spleen | A well-defined cystic lesion with heterogenous content due to the presence of debris. | A well-defined hypoattenuating lesion with thin wall and lack of enhancement on post contrast. | Variable T1 signal intensity due to presence of haemorrhage or proteinaceous material and high T2 signal intensity. |
| Splenic haematoma | A well-defined hypoechoic region with defined borders. | A well-defined hypoattenuating lesion with lack of enhancement on post contrast. | Variable depending on the stage of evolution. |
Similar case has been reported in the literature by Garg M et al., [11] where they found a large heterogenous solid cystic lesion in the left supra renal region measuring 15×12 cms on ultrasonograhic examination. Two calcified cystic lesion were found on computed tomographic examination and it was proven to be splenic hydatid on histopathological examination.
Similarly Dilli A et al., has reported a case of splenic hydatid which presented with a multilocular cystic lesion measuring 12×11 cms in the splenic hilum displacing the left kidney to inferolateral in position [12]. On CT, it was found to be a hypoenhancing hypo attenuating cystic lesion and had T2 hypointense rim on T2 weighted MRI images for which total splenectomy was done and it was pathologically proven to be splenic hydatid.
Pukar MM and Pukar SM, has reported a case of splenic hydatid where they found a large homogenous cystic lesion measuring 20×22 cms with multiple septa in the spleen almost occupying the whole of the parenchyma and displacing the bowels to the right [13]. On exploration it was found that the cystic lesion was attached to the left hemidiaphragm for which en block splenectomy with resection of diaphragm and subcutaneous tissue was performed which is not found in this case. Serologically it was proven to be hydatid.
Acharya S et al., has reported an unusual case of hydatid cyst with complication [14]. In this report it was stated that a middle-aged women came with complaints of pain and abdominal distension. CECT revealed a large cystic lesion in the splenic parenchyma with internal floating membranes and the lesion was seen extending to perisplenic region. The patient also had ascites, hepatomegaly and features of portal hypertension which were all complications of the cystic lesion. He has also quoted a study saying that rupture of splenic hydatid into peritoneal cavity was reported in only 1.7% of cases where the patient presents with acute abdomen and abdominal distension. It was stated that during surgery dense adhesions were found over stomach, diaphragm, transverse colon and omentum.
Kar JK and Kar M, has reported a case of splenic hydatid where the blood investigations were found unremarkable [15]. On ultra sonographic examination, splenomegaly was found with a unilocular cystic lesion with no evidence of any daughter cysts. This case differs from present case by the absence of daughter cysts which is the most common presentation of a hydatid disease. At the time of laparotomy clear fluid was aspirated and cyst was excised. He also stated that splenic cystectomy was performed for the patient, whereas splenectomy is the ideal procedure for hydatid disease. However, postoperative period was uneventful and no recurrence was found till two-year follow-up period.
Kumar V et al., has reported a similar case of splenic hydatid where it presented as a loculated cystic lesion in the splenic parenchyma without any complications for which splenectomy was performed for the patient and the postoperative period was uneventful [16].
Though spleen is least commonly affected when compared to liver, similar case reports have been published emphasising the fact that it should be kept as a differential in cases of cystic lesions of spleen.
Conclusion(s)
Unilocular or a multilocular cystic lesion should raise the suspicion of hydatid cyst, pariticularly in places where it is endemic and hydatid cysts can occur in unusual locations as well. Splenic hydatid cysts are usually solitary and occurs as a result of either systemic dissemination or intraperitoneal spread from a ruptured hepatic hydatid cyst.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 02, 2020
Manual Googling: Feb 23, 2021
iThenticate Software: Mar 22, 2021 (8%)
[1]. Pumarola A, Rodriguez-Torres A, García-Rodriguez JA, Piédrola-Angulo G, Microbiología y parasitología médica 1990 2nd edBarcelona, SpainSalvat [Google Scholar]
[2]. King CH, Cestodes (tapeworms) In: Mandell GL, Bennett JE, Dolin RPrinciples and practice of infectious diseases 1995 4th edNew York, NYChurchill Livingstone:2544-53. [Google Scholar]
[3]. Moro P, Schantz PM, Echinococcosis: A reviewInt J Infect Dis 2009 13(2):125-33.10.1016/j.ijid.2008.03.03718938096 [Google Scholar] [CrossRef] [PubMed]
[4]. Moguillanski SJ, Gimenez CR, Villavicencio RL, Radiología de la hidatidosis abdominal. In: Stoopen ME, Kimura K, Ros PR, edsRadiología e imagen diagnóstica y terapeútica: Abdomen. Vol 2 1999 Philadelphia, PALippincott Williams & Wilkins:47-72. [Google Scholar]
[5]. Beggs I, The radiology of hydatid diseaseAJR Am J Roentgenol 1985 145:639-48.10.2214/ajr.145.3.6393895873 [Google Scholar] [CrossRef] [PubMed]
[6]. de Diego J, Lecumberri FJ, Franquet T, Ostiz S, Computed tomography in hepatic echinococcosisAJR Am J Roentgenol 1982 139:699-702.10.2214/ajr.139.4.6996981931 [Google Scholar] [CrossRef] [PubMed]
[7]. Marani SA, Canossi GC, Nicoli FA, Alberti GP, Monni SG, Casolo PM, Hydatid disease: MR imaging studyRadiology 1990 175(3):701-06.10.1148/radiology.175.3.23431172343117 [Google Scholar] [CrossRef] [PubMed]
[8]. Franquet T, Montes M, Lecumberri FJ, Esparza J, Bescos JM, Hydatid disease of the spleen: Imaging findings in nine patientsAJR 1990 154:525-28.10.2214/ajr.154.3.21062142106214 [Google Scholar] [CrossRef] [PubMed]
[9]. Durgun V, Kapan S, Kapan M, Karabiçak I, Aydogan F, Goksoy E, Primary splenic hydatidosisDig Surg 2003 20(1):38-41.10.1159/00006886412637803 [Google Scholar] [CrossRef] [PubMed]
[10]. Dontigny L, Mercier C, Pagé A, Lévy R, Cossette R, Pelletier C, An unusual case of hydatid cystCan J Surg 1976 19:23-25. [Google Scholar]
[11]. Garg M, Mangal A, Tak H, Singh DP, Soni A, Isolated large primary splenic hydatid cyst: A case reportAsian Pac J Trop Dis 2015 5(Suppl 1):S178-180.10.1016/S2222-1808(15)60884-2 [Google Scholar] [CrossRef]
[12]. Dilli A, Idil Güneş Tatar, Umit Yasar Ayaz, Baki Hekimoglu, “Isolated Splenic Hydatid Disease”Case Reports in Medicine 2011 2011Article ID 763895, 3 pages. https://doi.org/10.1155/2011/76389510.1155/2011/76389521317988 [Google Scholar] [CrossRef] [PubMed]
[13]. Pukar MM, Pukar SM, Giant solitary hydatid cyst of spleen- A case reportInt J Surg Case Rep 2013 4(4):435-37.10.1016/j.ijscr.2012.12.01923500751 [Google Scholar] [CrossRef] [PubMed]
[14]. Acharya S, Ghimire B, Khanal N, Spontaneous rupture of isolated splenic hydatid cyst without acute abdomen: A case reportClin Case Rep 2019 7(11):2064-67.10.1002/ccr3.242431788252 [Google Scholar] [CrossRef] [PubMed]
[15]. Kar JK, Kar M, An unusual presentation of primary splenic hydatid cystTrop Parasitol 2011 1:126-28.10.4103/2229-5070.8696423508297 [Google Scholar] [CrossRef] [PubMed]
[16]. Kumar V, Mittal DD, Rastogi GP, Splenic Hydatid Cyst: A Case ReportAnn Int Med Den Res 2017 3(5):SG13-14.10.21276/aimdr.2017.3.5.SG4 [Google Scholar] [CrossRef]