Induction can be considered as one of the most crucial events in anaesthesiology, as it is associated with number of alternations in haemodynamic and physiology of various body systems.
Propofol, is a preferred induction agent due to its properties of smooth and rapid induction, rapid awakening and orientation times, clear headed recovery, decreased incidence of postoperative nausea, vomiting, better intubating conditions and upper airway integrity. Inspite of all it’s advantages, an induction dose of propofol of 2-2.5 mg/kg can be hazardous because vasodilation and cardiovascular depressant action, can cause profound hypotension [1,2].
Therefore, using a smaller total dose of propofol could offset the hypotension that it causes. The application of priming principle is well-documented with regard to the use of non-depolarising muscle relaxants, where priming shortens the onset of neuromuscular blockade, provides better intubating conditions and reduces the total required dose of the drug.
However, studies using priming principle for propofol are few. Hence, this study was undertaken to observe whether priming with propofol reduced the actual induction dose of the drug and thereby, providing a stable haemodynamic state in ASA 1 and II patients in the set up.
Materials and Methods
After obtaining Ethical Committee Clearance, dated 15th October 2018, the randomised controlled study was conducted in ACS Medical College and Hospital, Chennai from December 2018 to February 2020. Sample size was calculated considering the mean reduction in dose requirement between the groups as (30±23.89) mg for Study Group (SG) and (30±20.28) mg for Control Group (CG). The power was 90%, alpha error was 5% with 95% confidence [Table/Fig-1].
Flowchart showing the patient distribution.
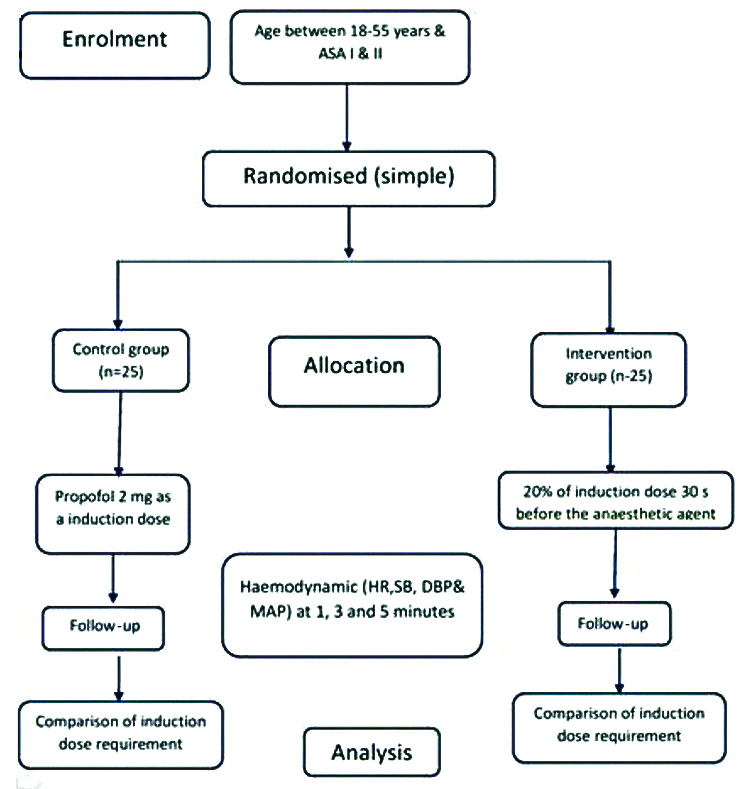
Inclusion criteria: Consent was taken from patients in study. Total 50 consenting patients age between 18-55 years, belonging to ASA-I or ASA-II category undergoing surgery under general anaesthesia.
Exclusion criteria: Patients with known allergy to propofol and its constituents (egg and eggproteins), pregnant and lactating women, BMI >35, patients premedicated with clonidine for induced hypotension were excluded from the study.
Procedure: During preanaesthetic assessment, a detailed history and clinical examination of each patient was carried out to optimise them before surgery. Relevant investigations appropriate to the patient age and co-morbidities were requested.
Patients were diveded into two equal groups randomly, based on closed envelope method. There was a fasting period of 8 hours and patients were premedicated on the previous night and morning of surgery with tab. diazepam 5 mg and tab. ranitidine 150 mg.
All patients were connected to standard multiparameter monitor (DASH 3000/4000 monitor by GE medical monitoring systems) to monitor the Electrocardiogram (ECG), non-invasive blood pressure and pulse oximetry. An 18G or 20G cannula was inserted in all patients with a free-flowing drip of lactated ringers’ solution. All patients were pre-oxygenated with 100% oxygen for 3 minutes.
Patients in both groups received an anti-sialagogue Inj. Glycopyrrolate 0.2 mg and Inj. Midazolam 2 mg 5 minutes before the procedure. All patients received Inj fentanyl 1 mcg/kg over 30 seconds.
Patients in CG were injected propofol at a speed of 30 mg/10 sec until the loss of eyelash reflex. Patients in SG received 20% of the total calculated dose of Inj. Propofol (2 mg/kg). After 30 seconds the remaining calculated dose of propofol was injected at a rate of 30 mg/10 seconds till the loss of eyelash reflex. Based on other studies, 20% of the total calculated dose was chosen as the priming dose and the time interval between priming and induction dose was decided as 30 seconds [1-4].
Intubation was accomplished with Inj. Suxamethonium 1.5 mg/kg intravenously and Vecuronium was used subsequently as a muscle relaxant intraoperatively. Anaesthesia was maintained with isoflurane, O2 and N2O (50:50). No surgical stimulus was allowed for the first 5 minutes.
Total dose of propofol required was calculated; while in the SG it included the priming dose too. Pulse rate and non invasive blood pressure (systolic, diastolic and mean blood pressure) were recorded at the following intervals-baseline, 1 minute, 3 minutes and 5 minutes after induction in both the groups. Baseline was an average of first 2 preoperative values recorded 3 minutes apart in the operating room. Any complications like apnea, vomiting, involuntary movements, laryngospasm and coughing at induction were also noted.
Statistical Analysis
The data was entered and analysed using Statistical Package for the Social Sciences (SPSS) version 17.0 statistical software. Student’s t-test and Pearson’s Chi-square test was the statistical test of significance. The p-value ≤0.05 was considered as significant.
Results
The demographic data were comparable for age, BMI and gender [Table/Fig-2]. The surgeries done under various specialities in the two groups are shown in [Table/Fig-3].
| Parameter | Study group | Control group | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Age (years) | 39.4±9.260 | 36.92±12.234 | 0.423 |
| BMI | 26.070±3.0579 | 26.530±3.9326 | 0.646 |
| Gender (n) (M/F) | 8/17 | 10/15 | 0.556 |
n: Number of patients; p-value<0.05 significant
| Parameter | Study group | Control group | Total |
|---|
| General surgery | 7 | 8 | 15 |
| Gynaecology | 14 | 9 | 23 |
| Orthopaedics | 1 | 3 | 4 |
| Dental | 0 | 1 | 1 |
| ENT | 3 | 3 | 6 |
| Urology | 0 | 1 | 1 |
The mean of total induction dose of propofol was 107.60±29.33 mg in the CG compared to 88.84±21.03 mg in SG which was statistically significant (p=0.012) as shown in [Table/Fig-4]. Also, the mean induction dose required in SG was 1.77 mg/kg against 2.15 mg/kg in CG.
Mean total induction dose.
| Propofol | Study group (Mean±SD) | Control group (Mean±SD) | p-value |
|---|
| Induction dose (in mg) | 88.84±21.03 | 107.60±29.33 | 0.012* |
*p-value <0.05 significant
The haemodynamic parameters were compared before induction, 1 minute, 3 minutes, and 5 minutes after induction. The baseline HR, SBP, DBP, MAP, which were an average of two recordings 3 minutes apart, were comparable between the two groups. It was observed that the mean heart rate was significantly high in CG at 1 minute after induction (p=0.017) and 3 minutes after induction (p=0.099) as shown in [Table/Fig-5]. However, the heart rate at 5 minutes after induction was comparable between the two groups (p=0.231). Change in systolic blood pressure was seen ax depicted in [Table/Fig-6].
| Heart rate | Study group | Control group | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 86.16±12.91 | 89.04±16.63 | 0.497 |
| 1 min | 87.04±14.07 | 95.48±9.70 | 0.017* |
| 3 min | 90.68±14.18 | 97.0±12.34 | 0.099* |
| 5 min | 90.72±14.69 | 95.68±14.18 | 0.231 |
*p-value <0.05 significant
Changes in Systolic Blood Pressure (SBP).
| SBP | Study group | Control group | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 128.68±12.69 | 132.72±17.62 | 0.357 |
| 1 min | 118.48±17.81 | 105.20±22.14 | 0.024* |
| 3 min | 120.12±21.81 | 108.2±10.16 | 0.017* |
| 5 min | 112.56±20.68 | 107.36±9.72 | 0.48 |
*p-value <0.05 significant
The mean diastolic blood pressure was higher in SG, at 1 minute after induction (p=0.044) and 3 minutes after induction (p=0.028), compared to CG and were statistically significant as shown in [Table/Fig-7].
| DBP | Study group | Control group | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 76.52±8.71 | 76.88±9.64 | 0.890 |
| 1 min | 74.20±12.14 | 68.20±7.96 | 0.044* |
| 3 min | 74.48±17.53 | 66.0±6.41 | 0.028* |
| 5 min | 72.84±14.28 | 69.56±11.14 | 0.370 |
*p-value <0.05 significant
The mean blood pressure values at 1 minute after induction (p= 0.003), 3 minutes after induction (p=0.015) were higher in SG compared to CG and significant statistically as shown in and [Table/Fig-8]. It was also observed that 6 patients (24%) in CG and 13 patients (68%) in SG had developed various complications as shown in [Table/Fig-9].
Mean arterial pressure changes.
| MAP | Study group | Control group | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 93.91±8.73 | 95.49±11.36 | 0.583 |
| 1 min | 88.96±10.57 | 80.53±8.69 | 0.003* |
| 3 min | 89.69±18.04 | 80.07±6.11 | 0.015* |
| 5 min | 86.08±14.04 | 82.16±8.17 | 0.234 |
*p-value ≤0.01
| Complications | Control group | Study group | p-value |
|---|
| Apnea | 0 | 3 | 0.074 |
| Involuntary movements | 1 | 1 | 1.0 |
| Coughing | 1 | 2 | 0.552 |
| Fasciculations | 4 | 11 | 0.031* |
| Total | 6 | 17 | |
Other complications like vomiting and laryngospasm were not observed in either groups.
Discussion
The authors conducted this study to evaluate the effect of the priming principle on the induction dose of propofol. They looked for a reduction in the total dose of propofol which would produce a stable haemodynamic state. It was observed that there was 17.43% reduction in the induction dose requirement of propofol by applying priming principle. Kumar A et al., found a 27.48% reduction, Kataria R et al., reported 31.88% reduction [1,2], Baliarsing LA and Mhamane RA reported 33% reduction [5], Karlo R et al., found 10.23% reduction [3] and Prathapadas U et al., reported 40% reduction in the induction doses of propofol in their respective studies [6].
The mean induction dose required in SG was 1.77 mg/kg against 2.15 mg/kg in CG. The reduction in the induction dose could be attributed to the anxiolytic effect of propofol at sub hypnotic doses. This significant reduction in the dosage may be attributed to the unique pharmacokinetic and pharmacodynamic mechanisms of propofol. Cardiac output plays a small, yet significant predictive role in determining the hypnotic dose of propofol. It is noted that for a given dose of propofol, the effective plasma concentration is higher in a patient with low cardiac output than the one with a high cardiac output. Patient anxiety and pain are the main contributors to increased cardiac output state during the induction phase of anaesthesia [7]. The initial priming dose of propofol produces anxiolytic and amnestic effects. This results in reduced cardiac output during induction, and thus, an increased effective plasma-site concentration is achieved with a significantly lower dose of propofol.
Administration of sub-hypnotic doses of propofol produces anxiolysis. Hence, the induction dosage is reduced. The amnestic and sedative action of propofol at sub-hypnotic doses may facilitate induction of propofol at lower doses [7].
The increase in the mean heart rate [Table/Fig-5] at 1 minute and 3 minutes after induction in CG, is similar to the increase in the heart rate observed by Kumar A et al., and Kataria R et al., [1,2]. A greater reduction in systemic vascular resistance in the CG could have triggered off an increased sympathetic activity causing tachycardia.
The mean SBP was significantly higher in the SG at 1 minute and 3 minutes after induction. In the study by Gvalani S and Bhodane S with an increase in the induction dose of propofol, the mean arterial pressure dropped, confirming that haemodynamic side effects of propofol are dose-dependent [4]. The fall in the SBP compared to baseline at 1 minute after induction was 20.73% in CG compared to 7.92% fall in SG (p=0.024). At 5 minutes after induction, the fall in SBP was comparable in both the groups (p=0.017). The decrease in the SBP in CG compared to SG could be attributed to the higher induction dose requirements in the CG.
The mean diastolic blood pressures were also lower in the CG at 1 minute (p=0.044) and 3 minute after induction (p=0.028), compared to SG [Table/Fig-7]. However, the mean DBP at 5 minutes after induction was comparable between the two groups.
The mean blood pressure values at 1 minute (p=0.003) and at 3 minutes (p=0.015), were significantly lower in the CG [Table/Fig-7]. There was 5.27% fall in MAP in SG compared to 15.6% in the CG at 1 minute after induction. The mean blood pressure at 5 minutes after induction was comparable between the two groups. Kumar A et al., also showed a 6.41% reduction in MAP in the primed group as against a 11.45% reduction in the non-primed group at 1 minute [1].
Propofol reduces blood pressure by decreasing vascular smooth muscle tone and total peripheral resistance. The vasodilatation and reduction in cardiac output are postulated to be the causes of reduction in the MAP by 22-33%. The mechanism that could account for the decrease in cardiac output may be its action on sympathetic drive to the heart and negative ionotropic effect [8]. Thus, it was observed that there were minimal haemodynamic alterations during induction with use of priming principle in the SG.
The overall incidence of various complications was 68% in SG compared to 24% in CG. Clinically, observed apnea (>30 secs) was seen in 3 patients of the SG. Though it was not statistically significant (0.074), this was only seen in the SG. Involuntary movements and coughing were comparable between the two groups. Another significant observation noticed in the study was the occurrence of fasciculations following administration of suxamethonium, 11/25 (56%) patients in the SG compared to 4/25 (16%) patients in the CG (p-value=0.031) exact mechanism by which fasciculations occur is not known. but most of the hypothesis proposed, attributed them to a prejunctional depolarising action of nerve terminals and antidromic discharges that manifest as uncoordinated muscle contractions [8]. The reduced incidence of fasciculations in the CG could probably be attributed to the deeper plane achieved by the bolus dose of propofol. Patients in SG received only 82% of the bolus dose of propofol compared to the CG, which was probably insufficient to prevent fasciculations.
Limitation(s)
The small sample might have been insufficient for exploring statistical significance. Accurate rates of infusion could have been ensure with the syringe pump rather than manually stopwatch. The study was done only on endo tracheal tube placements. Hence, the results cannot be extrapolated to supraglottic airway device placement.
Conclusion(s)
Based on the results obtained from the study it can be concluded that, application of priming principle for induction dose of propofol reduces the induction dose requirements, associated with favourable peri-intubation haemodynamic alterations. However, further studies with larger samples and varying priming doses are required before considering these observations as generalised.
n: Number of patients; p-value<0.05 significant
*p-value <0.05 significant
*p-value <0.05 significant
*p-value <0.05 significant
*p-value <0.05 significant
*p-value ≤0.01