The RPTs are uncommon neoplasms representing 3.5 to 4% of germ cell tumours in paediatric age group [1,2]. Although, extragonadal germ cell tumours are more common in children than gonadal sites, sacrococcygeal teratomas account for majority of cases [3]. About 80% of childhood RPT present before five years of age, with maximum incidence during first year of life [4]. They usually present as distention of abdomen and a palpable lump [1]. A preoperative diagnosis can be made because of distinctive findings on imaging. But, imaging features often overestimate the tumour size and may be misleading [2,5].
Surgical exploration of RPT is a challenge because of enormous size and adherence to surrounding organs as well as major blood vessels [2]. Even benign tumours can be fatal in newborns and young infants [6]. One should be versed with the extent of tumour and relationship with vital structures before operating. In spite of their horrific intraoperative appearance, they are amenable for curative excision [5]. Lack of adequate exposure with these tumours is another factor, because of its rarity. The studies on RPT are limited and literatures are scanty to provide enough knowledge.
The present study was conducted to analyse the demographic pattern, clinical profile and outcome of RPTs managed in our tertiary care paediatric institute in last seven years.
Materials and Methods
This retrospective cohort study was carried out in the Paediatric Surgery Department located in the eastern part of India. The hospital records of children with RPT admitted between June 2013 and May 2020 were reviewed. It was conducted in accordance with ethical standards and Institutional Ethics Committee approval was obtained for the study (IEC/38/2020/289). The diagnosis of RPT was based on radiological and intraoperative findings and was confirmed by histopathology. Data were analysed for demographic pattern, clinical findings, pathological features and outcome.
Inclusion criteria: Patients who were operated and a confirmative diagnosis of RPT was made based on histopathological findings, patients up to the age of 14 years were included.
Exclusion criteria: Children in whom a provisional diagnosis of RPT was made but, surgery was not performed because of refusal by parents, patients who left against medical advice.
After hospitalisation, routine blood investigation, Serum Alpha-Fetoprotein (AFP), X-ray abdomen and ultrasonography were done in all cases. A preoperative Computed Tomography (CT) scan was also performed and laparotomy was planned. Details about the management approach was explained to parents and written consent obtained. Surgery was performed under general anaesthesia and the resected tumours were sent for histopathological study. Postoperative care with intravenous fluids antibiotics and supportive treatment was continued. Patients were allowed oral diet after the bowel function resumed. At discharge they were advised for follow-up with histopathology report. The patients were followed-up with ultrasonography as well as serum AFP every three months till one year and every six months thereafter.
Statistical Analysis
Data analysis was done using Microsoft Excel Q1 Macros software. Results were presented as percentages (%). Fisher’s-exact test was used for comparison between various groups such as: (i) RPT and other solid abdominal tumours; (ii) histological types of teratomas. The results were considered significant, when the value of p<0.05.
Results
A total of 88 cases of intra-abdominal solid tumours were operated during the study period (47 male and 41 female children). RPT was detected in 16 cases (18.18%) and it was the second most common following Wilm’s tumour [Table/Fig-1]. The median age at presentation was one year (range: one month to 12 years) and infants accounted for 56% of cases [Table/Fig-2]. There were 11 male and five female children in the study (M:F=2.2:1). A male preponderance was observed among RPT patients in comparison to other intra-abdominal solid tumours; n=72, 36 males and 36 females (p=0.26: Fisher’s-exact test). All 16 patients presented with abdominal distention and palpable abdominal mass. Although, a provisional diagnosis was made based on X-ray and ultrasonography, Contrast Enhancing Computed Tomography (CECT) scan was done in all cases to accurately delineate the tumour, its extension and relation to the surrounding structures. Serum AFP was elevated in five patients with a mean value of 258 ng/mL. Laparatomy was done through supraumbilical transverse incision in 15 cases and it was extended to the side of mass. In these cases, the tumours were in pararenal area and renal vessels were stretched over the tumour surface. Inferior vena cava was displaced by the tumour in eight cases. In one patient, who was preoperatively diagnosed as Wilm’s tumour, it was found that, the kidney was separate from tumour, atrophic and small in size [Table/Fig-3]. Renal vessels were encased within the teratoma, which was resected along with atrophic left kidney. The tumour was approached through midline incision above the umbilicus in one patient, as it was present in epigastrium. The tumour was adherent to stomach, pancreas and diaphragm. In all cases, the tumours were excised completely without any spillage or damage to surrounding structures.
Frequency of solid abdominal tumours.
| Pathology | Number of cases (%) |
|---|
| Wilm’s tumour | 52 (59.09) |
| Retroperitoneal teratoma | 16 (18.18) |
| Neuroblastoma and other adrenal tumours | 15 (17.04) |
| Rhabdomyosarcoma bladder | 3 (3.41) |
| Ovarian tumour | 2 (2.27) |
| Total | 88 |
Demographic pattern, pathology and outcome of 16 children with Retroperitoneal Teratoma (RPT).
| Age | Sex | Weight (Kg) | Site | Treatment | Histopathology | Outcome |
|---|
| 3 months | F | 4.9 | Left pararenal | Excision | Mature teratoma | Cured |
| 12 years | M | 22.2 | Left pararenal | Excision | Mature | Cured |
| 1 month | F | 3 | Left pararenal | Excision | Mature | Cured |
| 4 years | M | 11.3 | Right pararenal | Excision | Mature | Cured |
| 1 month | M | 3.6 | Left pararenal | Excision | Immature teratoma | Cured |
| 8 years | M | 18 | Right pararenal | Excision | Mature | Cured |
| 3 months | M | 4.7 | Left pararenal | Excision | Mature | Cured |
| 8 years | M | 17 | Right pararenal | Excision | Mature | Cured |
| 4½ years | M | 13 | Right pararenal | Excision | Mature | Cured |
| 4½ years | F | 15 | Left pararenal | Excision | Mature | Cured |
| 1 year | M | 7.6 | Right pararenal | Excision | Mature | Cured |
| 3 months | M | 4.3 | Left pararenal | Excision | Mature | Cured |
| 5 months | M | 7 | Right pararenal | Excision | Mature | Cured |
| 1 year | F | 8.5 | Left pararenal | Excision | Immature teratoma | No tumour recurrence |
| 9½ years | M | 29.5 | Bilateral supraumbilical | Excision and chemotherapy | Malignant | No tumour recurrence |
| 6 months | F | 8 | Left pararenal | Excision | Mature | Cured |
M: Male; F: Female
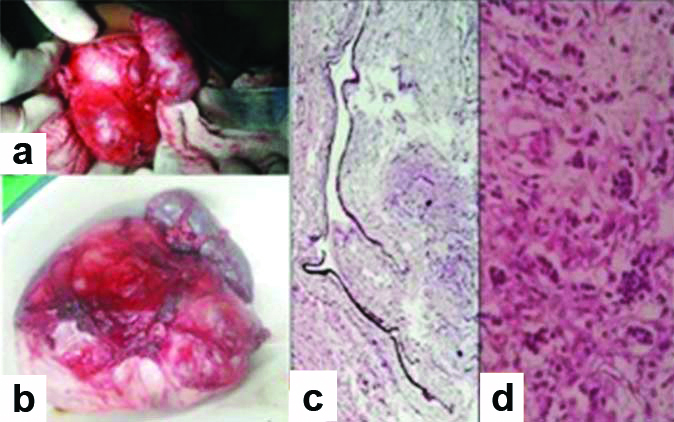
Immature teratoma in a one-year-old female child: (a) Intraoperative picture with atrophic left kidney; (b) Excised specimen; (c) Focus of teratoma with melanotic neuroectodermal elements-Pigmented epithelial cells with surrounding immature glial and mesenchymal elements (40X, H&E); (d) Clusters of small round cells (40X, H&E).
On gross examination, the tumours were loculated mass and cut section revealed cysts of various sizes containing pultaceous material with hairs. Bones and teeth were detected in some cases. Anaesthesia recovery and postoperative periods were uneventful. Although, two patients were shifted to intensive care unit, they did not need ventilator support. All the patients were discharged on oral diet and medications. Histopathology suggested benign mature teratoma [Table/Fig-4] in 13 cases (81.25%) and immature teratoma was found in two cases (13%). Although, statistically not significant, immature teratomas were more commonly detected among infants as compared to older children in the present study (p-value=0.48: Fisher’s-exact test). In one patient (6%) with bilateral tumour, the histopathology revealed teratoma with secondary malignant transformation to papillary carcinoma of thyroid and he was advised for chemotherapy [Table/Fig-5]. Serum AFP was returned to normal postoperatively in all cases. Follow-up was continued with ultrasonography and AFP. The period of follow-up ranged from six months to five years and there was no tumour recurrence.
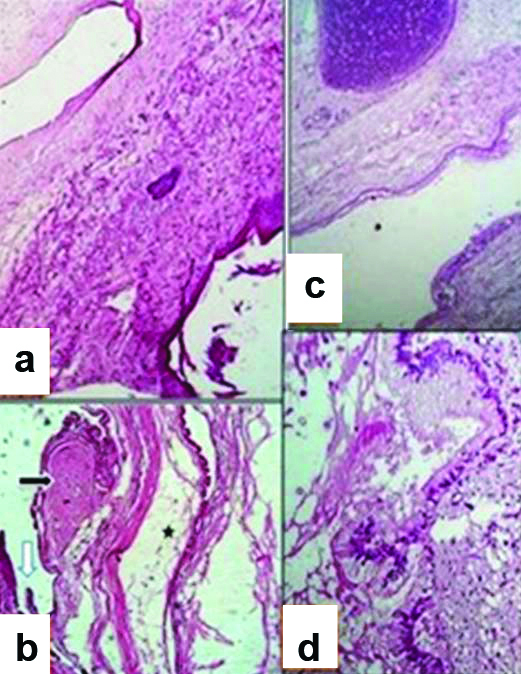
Mature (Benign) cystic teratoma; photomicrograph in a six month female infant [40X H&E]. (a) Mature keratinised stratified epithelial lining with hair follicles. (b) Respiratory mucosal lining (white arrow), smooth muscle bundles (black arrow) and adipose tissue (asterisk). (c) Organised respiratory conductive system units. (d) Gastric foveolar lining epithelium.
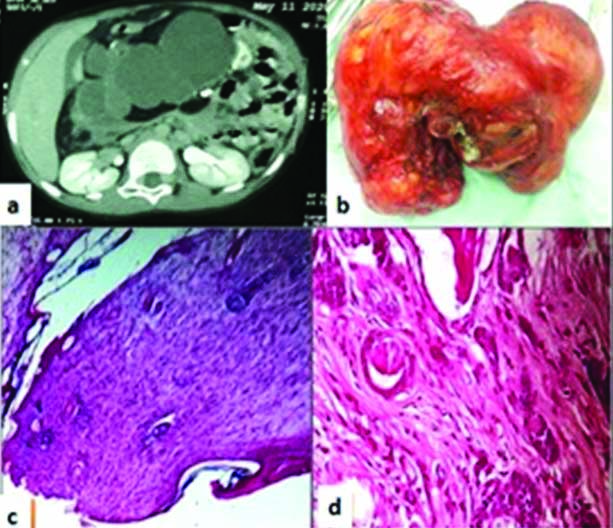
Somatic-type malignancy in a nine and a half-year-old male child with retroperitoneal teratoma: (a) CT scan showing bilateral teratoma anterior to pancreatic body and displacing transverse colon inferiorly; (b) Excised specimen; (c) Keratinised stratified squamous epithelium lining the cystic mass (40X, H&E); (d) Focal area of Papillary carcinoma of thyroid (100X, H&E).
Discussion
The RPTs are rare and comprise only 1-11% of primary retroperitoneal neoplasms in paediatric age group [7,8]. However, a higher incidence was observed in this study and teratomas constituted 18% of the neoplasms. Teratomas have been described as third common retroperitoneal tumour following neuroblastoma and Wilm’s tumour in childhood [9]. However, it was detected as second common neoplasm, only after Wilm’s tumour in this study. Majority of the cases present during infancy and 80% present before five years of age [4]. Similar observation was made in the present study, as 75% of cases were below five years of age with maximum incidence during first year of life. We also observed that, boys were more commonly affected than girls in RPT in comparison to other abdominal solid tumours (p-value=0.26: Fisher’s-exact test). The male preponderance found in this study was also marked by Rattan KN et al., [2]. However, a female predominance is reported by previous studies [1,6]. The presenting feature such as abdominal distention and palpation of a solid mass, were also marked in most of the series [1,2,5,6].
Traditionally, ultrasonography is considered as first imaging modality for evaluation of paediatric abdominal mass [2,5]. But, Schey WL et al., recommended only plain X-ray abdomen and suggested resection of tumour, if characteristic calcification is detected [10]. Abdominal radiography showing bones or teeth is considered to be most helpful for preoperative diagnosis [6]. CT scan has been suggested to accurately delineate the extent of tumour and its relationship to surrounding structures including major blood vessels. CT scan was done in all our cases before laparotomy. But, in many cases it was found that, the extent of tumour observed on imaging is more than actually detected during surgical exploration. This observation was also made by other studies [1,5,11]. Therefore, CT scan report regarding tumour size should not prevent exploration.
Although, we found a left-sided predilection similar to Chaudhary A et al., no specific side predilection was marked in other studies [1,2,5]. Complete surgical excision is curative for benign teratomas and even bilateral tumours are amenable for complete excision [2,5]. Various degree of adherence to surrounding structures was encountered during exploration but, complete resection was successful in all the cases, including the bilateral tumour. It is described that, even benign teratomas can encase vessels causing injury to involved organ or intestine [4]. In one case, renal vessels were sacrificed to allow complete removal of the tumour. Until now, only one case of RPT with atrophic kidney is reported in English literature [7]. We report herewith the second such case, where excision of teratoma along with nephrectomy was performed in childhood.
Majority of RPT reported are of mature (benign) variety [1,2,5,11]. These tumours are usually cystic in nature and contained elements derived from embryonic germ layers; ectoderm, mesoderm and endoderm. The most frequent components are ectodermal derivatives like keratinised stratified squamous epithelium, hairs and dental structures. The common mesodermal derivatives are adipose tissue, bones, cartilage and smooth or striated muscles. The endodermal derivatives such as intestinal mucosa, respiratory mucosa, thyroid and renal tissues can also be encountered. Immature teratomas are rare and are mostly reported as individual case reports [3,12,13]. They are composed of undifferentiated immature tissues such as neuroglia, neural tubes and are associated with malignant potential along with risk of tumour recurrence [13,14].
Jones NM and Kiely EM, found intimate adhesion of the tumour to retroperitoneal vessels as well as surrounding structures in all their six patients and partial gastrectomy was needed in one of their cases [15]. Our epigastric tumour was grossly adherent to stomach and adjacent organs. It was excised with difficulty and later on this tumour was found to be having malignant component. Some teratomas may differentiate with time along with malignant change, especially the immature teratomas [3]. Malignant components may be detected in 0 to 24% cases, out of which Yolk sac tumours are reported as most frequent histology (63%) [4,6]. Nephroblastic components are also reported in seven cases of RPT [13]. But, to the best of author’s knowledge, papillary thyroid carcinoma has not been reported as malignant component in paediatric RPTs. Postoperative chemotherapy is required for malignant cases, tumours with incomplete resection and recurrences [3,5]. Although, rarely encountered, the prognosis is poor in malignant lesions [2,3]. However, the overall prognosis is good in RPT, as most cases are benign and complete excision is curative [2,5]. We also agree with this, as there was no mortality during postoperative period and recurrence on follow-up. Serum AFP is a good tumour marker to monitor recurrences [1]. There is gross improvement in survival in RPT over the years, especially during last three decades [6]. This is largely attributable to increased recognition about these rare germ cell tumours in children and advances in operative techniques.
Limitation(s)
The major limitation of the present study is limited number of cases, due to rarity of these childhood neoplasms. Further, this unicentric study has its inherent problems such as selection bias. Because of the paucity of information, individual experiences will provide further insight and promote research on these germ cell tumours.
Conclusion(s)
The RPTs are uncommon childhood tumours, which usually present before five years of age. A preoperative diagnosis can be made because of distinctive imaging features. But, imaging can overestimate the tumour size as well as the extent and should not prevent surgical exploration. The two rare findings: (i) papillary thyroid carcinoma as a malignant component in childhood RPT; and (ii) renal atrophy secondary to RPT were important observations made in the present study. Since malignancy is not common in RPTs, complete excision should be attempted, even in bilateral lesions. But, early diagnosis is essential for curative surgery and recurrence should be assessed by serum AFP. However, multicentric studies on these neoplasms, especially focusing on genetic anomalies, tumour biology and environmental factors are future requirements.
M: Male; F: Female