Complex Percutaneous Coronary Intervention Salvages a Patient with Recurrent Acute Coronary Syndrome and Ischaemic Heart Failure with Multiple Life Threatening Co-morbidities: A Case Report
Brajesh Kunwar1, Farah Ingle2, Atul Ingle3, Chandrasekhar Tulagseri4
1 Senior Interventional Cardiologist, Head and Director of Cath Lab, Department of Cardiology, Fortis Hospital, Navi Mumbai, Maharastra, India.
2 Senior Physician, Department of Cardiology, Fortis Hospital, Navi Mumbai, Maharastra, India.
3 Senior Nephrologist, Department of Cardiology, Fortis Hospital, Navi Mumbai, Maharastra, India.
4 Senior Intensivist, Head ICU, Department of Intensive Care, Fortis Hospital, Navi Mumbai, Maharastra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Brajesh Kunwar, Fortis Hospital, Navi Mumbai, Maharastra, India.
E-mail: Kunwar_brajesh@yahoo.com
More than 422 million people are suffering from Diabetes Mellitus (DM) worldwide. Majority of the affected population resides in lower and middle income countries. This chronic, metabolic disease gradually does serious damage to heart, blood vessels, eyes, kidneys and nerves; eventually causing cardiovascular diseases, peripheral vascular diseases, retinopathy, nephropathy and neuropathy. Here, a rare case of a 58-year-old male was present who had history of uncontrolled DM with dry gangrene in right forefoot, acute kidney injury and Coronary Artery Disease (CAD) involving Left Main (LM) bifurcation presented with recurrent acute coronary syndrome with heart failure. Patient in view of multiple co-morbidities was unfit for Coronary Artery Bypass Grafting (CABG) was managed successfully with complex coronary intervention involving LM bifurcation.
Bifurcation, Coronary artery disease, Dry gangrene, Left main, Nephropathy
Case Report
A 58-year-old male was admitted with dry gangrene and pain in 2nd to 5th right foot toes secondary to the 23 year long standing uncontrolled type 2 DM. HbA1c levels at the time of admission was 8.3%. The patient complaint recurrent ischaemic heart failure. The cardiac enzyme levels were elevated; creatinine kinase was 45 IU/L and Troponin T was 105 ng/mL. Electrocardiogram showed sinus tachycardia with T-inversion in anterolateral leads with ST-segment depression. The 2D echocardiography revealed inferior wall hypokinesia with left ventricular ejection fraction of 45%. The patient was put on maximum medical management including antianginals and unfractionated heparin. In view of rising creatinine, patient was put on urgent haemodialysis along with reno-protective medications. Patient continues to show signs of cardiac ischaemia and it was decided to perform angiography after nephrologist fitness. Patient also showed feature of wound infection and the swab from gangrene showed growth of Escherichia Coli. The patient underwent right forefoot amputation (trans-metatarsal amputation) along with debridement and vacuum-assisted closure.
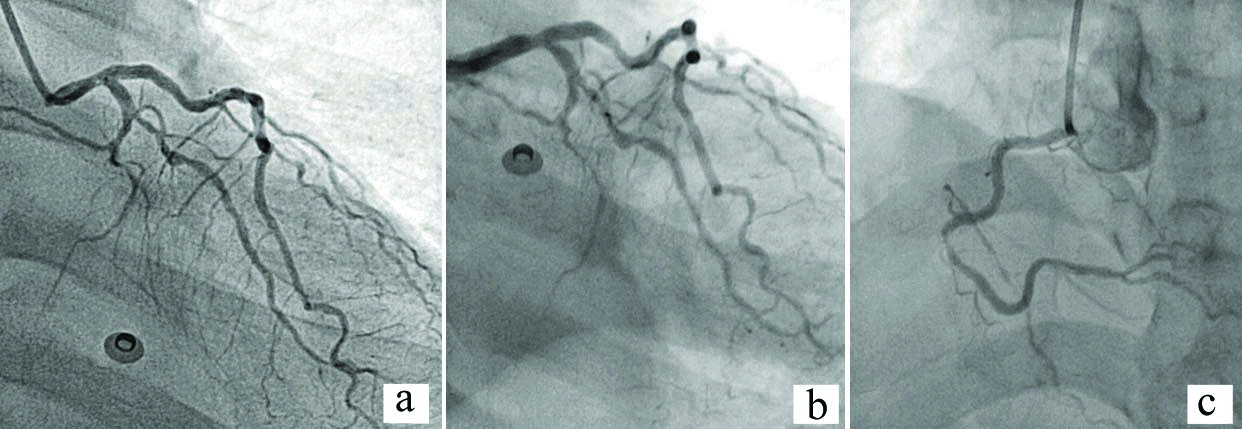
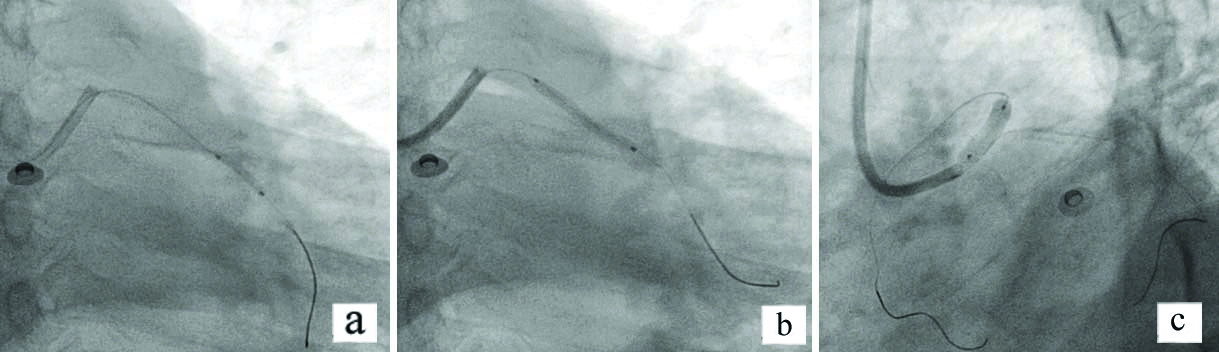
The condition suddenly deteriorated post amputation with dropping oxygen saturation requiring intensive care. The detailed timeline is presented in the [Table/Fig-1]. In view of recurrent episodes of cardiac ischaemia induced heart failure patient underwent coronary angiogram which revealed multivessel disease affecting 60-70% distal LM, 50% ostial Left Circumflex (LCx) 80% ostio-proximal Obtuse Marginal (OM) (Medina Classification 1,0,1) [1], 90% mid Right Coronary Artery (RCA) and minor disease in Left Anterior Descending (LAD) artery [Table/Fig-2a-c]. The SYNTAX score was 25. Heart team was approached and was advised for high risk Coronary Artery Bypass Graft (CABG) surgery in view of complex lesions (LM bifurcation and long standing DM). CABG surgery was outrightly refused by patient and relatives’ hence percutaneous coronary intervention was commenced. The LCx-OM lesion was crossed with Fielder FC 0.014” guide wire and pre dilated with Cosmos 2.0×10 mm balloon at 12 atm [Table/Fig-3a]. A 2.25×20 mm Tetrilimus (everolimus-eluting stent) was negotiated and deployed there at 14 atm [Table/Fig-3b]. Followed by this, a 3.50×16 mm Tetrilimus stent was negotiated from LM to ostial LAD and deployed at 14 atm [Table/Fig-3c].
Patients timeline of the events.
| Day | Intervention |
|---|
| Day 0 | Patient presented with dry gangrene and history of uncontrolled Diabetes Mellitus (DM), diagnosed with inferior wall hypokinesia, 45% left ventricle ejection fraction, acute kidney injury. Advised for haemodialysis. |
| Day 2 | Right forefoot wound swab was sent for diagnosis, reported positive for Escherichia Coli on day 5 |
| Day 7 | Right forefoot amputation was performed |
| Day 9 | Shifted toward from ICU |
| Day 12 | Underwent debridement and vacuum-assisted closure |
| Day 21 | Complained of breathlessness, Oxygen Saturation (SPO2) 93% on 5L Oxygen, shifted to ICU, cardiology and nephrology review taken |
| Day 24 | Shifted to ward |
| Day 25 | Again complained of breathlessness, SPO2 86% on room air, started with 3L of Oxygen SPO2 88% on 3L of Oxygen, 90% on 6L of Oxygen; advised to shift to ICU |
| Day 26-35 | Kept on complaining breathlessness and SPO2 levels were <90% |
| Day 36 | After nephrology clearance, advised for coronary angiography, multivessel disease diagnosed affecting Left Main (LM); percutaneous coronary intervention advised and performed |
| Day 48 | Discharged in stable condition |
Angiogram revealed LM, LCx-OM, LAD and RCA multi-vessel diseases.
LM: Left main; LCx-OM: Ostial left circumflex- ostio-proximal obtuse marginal; LAD: Left anterior descending; RCA: Right coronary artery
a) LCx-OM1 lesion crossed with Fielder FC 0.014” guide wire and pre dilated with Cosmos 2.0 mm×10 mm balloon at 12 atm; b) LCx-OM1 lesion deployed Tetrilimus stent 2.25 mm×20 mm at 14 atm pressure for 30 secs; c) Then LM to Ostial LAD stented with Tetrilimus stent 3.50 mm×16 mm at 14 atm pressure.
LCx-OM 1: Left circumflex- ostio-proximal obtuse marginal 1; LM: Left main; LAD: Left anterior descending
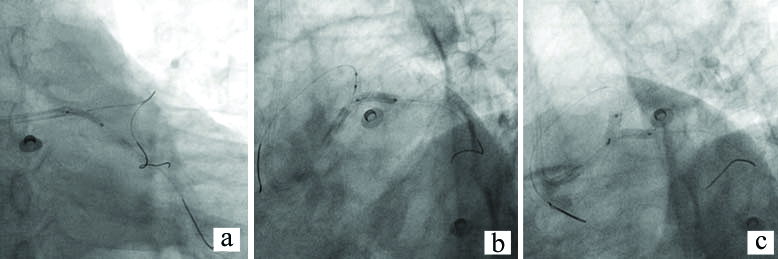
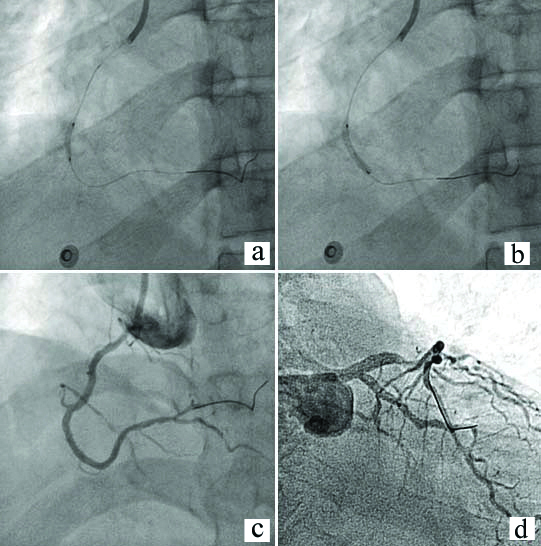
Angiogram showed pinching of LCx ostium, hence aggravating the ostial LCx stenosis further. Hence, it was decided to balloon dilate and consider bifurcation stenting of ostial LCx. Another Fielder FC guide wire was crossed into LCx through struts of stent implanted in LM and opened the struts with Cosmos 2.0×10 mm balloon [Table/Fig-4a]. A 2.50×12 mm Tetrilimus stent was negotiated through the created orifice and deployed at 14 atm [Table/Fig-4b]. The protruding struts of LCx stent was crushed by 3.5×8 mm NC balloon inflated in LM stent. The postdilatation was done at 16 atm. Followed by this, simultaneous kissing balloon in LM and LCx was done with 3.5×8 mm Cosmos NC balloon at 18 atm [Table/Fig-4c]. This is a modification of T stenting known as TAP (T and small Protrusion) technique. Proximal Optimisation Technique (POT) of LM coronary artery stent was done using 4×8 mm NC balloon at 10 atm. The RCA lesion was crossed with Fielder FC 0.014” guide wire and pre dilated with Cosmos 2.0×10 mm balloon at 12 atm pressure [Table/Fig-5a], followed by stenting with 2.25×16 mm Tetrilimus at 14 atm [Table/Fig-5b]. Post-stenting Thrombolysis in Myocardial Infarction (TIMI) III flow was achieved in all affected vessels [Table/Fig-5c,d]. Whole of the procedure was uneventful and patient tolerated the procedure well. Patient improved dramatically with de-escalation of heart failure and antianginal medications. Patient was under observation for a week and was stable during the hospitalisation. The patient was discharged in stable condition. Upon discharge, he was advised strict medication including dual antiplatelet, statins, beta blocker and Angiotensin-converting Enzyme (ACE) inhibitors. At 14 months follow-up, the patient is living a normal life.
a) Fielder FC guide wire crossed to LCx through the struts of the LM stent and opened the struts with Cosmos 2.0 mm×10 mm balloon; b) stented with Tetrilimus stent 2.50 mm×12 mm at 14 atm pressure; c) post dilated with stent balloon at ostial of LCx at 16 atm and simultaneous kissing balloon done with Cosmos NC 3.5 mm×8 mm balloon in LM at 18 atm.
LCx: Left circumflex; LM: Left main
a) RCA lesion was pre dilated with Comos 2.0 mm×10 mm balloon at 12 atm; b) RCA lesion stented with Tetrilimus 2.25 mm×16 mm at 14 atm; c) Post stent TIMI III flow RCA; d) Post stent TIMI III flow left circulatory system.
TIMI: Thrombolysis in myocardial infarction; RCA: Right coronary artery
Discussion
Worldwide a vast majority is affected by Diabetes Mellitus which is a chronic, metabolic disease. The number of population with DM have quadrupled in three decades [2]. India has the second highest number of population affected with DM. The complications of DM include nephropathy, neuropathy, retinopathy, stroke and coronary heart diseases. Individual with DM has two times more risk of developing cardiovascular diseases than a healthy person [3]. It is associated with other life threatening conditions like chronic kidney disease and gangrene. CAD involvement in diabetes is usually multivessel with diffuse disease. Associated co-morbidities makes the management of CAD in DM even more difficult. Critical coronary lesion involving bifurcation becomes frequent state of affairs requiring major surgical interventions. However, in emergency in a critical unstable patient with multiple co-morbidities, CABG may not be possible all the time [3].
The case presented here is a very rare presentation of several co-morbid conditions in a single subject due to patient’s long history of uncontrolled type 2 DM. Diabetes is associated with many life threatening complications and reduces the quality of life. The most common responsible or aggravating factor for gangrene is poor glycaemic condition of the individual [4]. The reports claim that diabetic patients have 15 times more chances of undergoing amputation than the non-diabetic population [5,6]. Diabetic nephropathy leading to chronic kidney disease is also very common [7]. The most common cause of death in patients with long standing uncontrolled diabetes is cardiac cause. CAD almost always accompanies the long standing diabetes. The coronary involvement in diabetes is usually diffuse and complicated with difficult anatomic subsets often requiring CABG. However, Percutaneous Coronary Intervention (PCI) do have a role in patients with simpler anatomy, patient refusal to surgical treatment, associated multiple co-morbid conditions making patient unfit for surgery and in emergency situation where doing CABG is not possible due to logistic approach [7].
Patient in this case had a long standing diabetes with chronic kidney disease and was already on dialysis. The patient also had infected gangrene of foot requiring amputation. Multiple co-morbid conditions along with recurrent ischaemic heart failure made him subset for a complex PCI against CABG. There were many considerations while performing the procedure including possibility of aggravation of contrast-induced nephropathy, technical expertise including selecting the right quality hardware and correct bifurcation technique. Post procedure care is also important as patient needed tight control of diabetes and dialysis [7].
Patient was initially taken for provisional bifurcation stenting. TAP technique as bifurcation procedure was selected as it is a simple technique requiring small quantity of contrast and less likelihood of intraoperative destabilisation of patient as reserves were on borderline. The TAP technique also ensures complete coverage of side branch ostium and also minimises stent overlapping. A total of four drug-eluting stents were implanted for treatment of CAD [7].
Conclusion(s)
Long standing uncontrolled diabetes causes multisystem diseases. Complex diffuse CAD is life threatening association. CABG is often preferred as revascularisation procedure, however it is always not possible due associated severe co-morbid conditions and in emergency. Complex PCI involving bifurcation stenting can be offered to these subject provided there are facilities of good hardware and technical expertise.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 14, 2020
Manual Googling: Jan 28, 2021
iThenticate Software: Feb 03, 2021 (7%)
[1]. Medina A, Suárez de Lezo J, Pan M, A new classification of coronary bifurcation lesionsRevista Española de Cardiología (English Edition) 2006 59(2):18310.1016/S1885-5857(06)60130-8 [Google Scholar] [CrossRef]
[2]. Unnikrishnan R, Anjana RM, Mohan V, Diabetes mellitus and its complications in IndiaNature Reviews Endocrinology 2016 12(6):357-70.10.1038/nrendo.2016.5327080137 [Google Scholar] [CrossRef] [PubMed]
[3]. Collaboration ERF, Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studiesThe Lancet 2010 375(9733):2215-22.10.1016/S0140-6736(10)60484-9 [Google Scholar] [CrossRef]
[4]. Tuttolomondo A, Maida C, Pinto A, Diabetic foot syndrome as a possible cardiovascular marker in diabetic patientsJournal of Diabetes Research 2015 2015:26839010.1155/2015/26839025883983 [Google Scholar] [CrossRef] [PubMed]
[5]. Salahuddin O, Azhar M, Imtiaz A, Latif M, A developing world experience with distal foot amputations for diabetic limb salvageDiabetic Foot & Ankle 2013 4(1):2247710.3402/dfa.v4i0.2247724155996 [Google Scholar] [CrossRef] [PubMed]
[6]. Al Wahbi A, Autoamputation of diabetic toe with dry gangrene: A myth or a fact?Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 2018 11:25510.2147/DMSO.S16419929910628 [Google Scholar] [CrossRef] [PubMed]
[7]. Nasri H, Rafieian-Kopaei M, Diabetes mellitus and renal failure: Prevention and managementJournal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences 2015 20(11):111210.4103/1735-1995.17284526941817 [Google Scholar] [CrossRef] [PubMed]