Introduction
In 2019, COVID-19 was first identified in Wuhan City in China, as a disease associated with the new Corona Virus Strain [1]. Globally, there are an estimated 73,575,202 confirmed cases and 1,656,317 confirmed deaths due to COVID-19 infection according to December 19th, 2020, WHO report. The disease was said to be transmitted through droplets from infected people and the route of transmission is by eyes, nose and mouth. Later, the virus gets lodged into the lungs through these entries [2]. Medical characteristics of COVID-19 vary from asymptomatic patients to Acute Respiratory Distress Syndrome (ARDS) and multiple organ failures. A cascade of inflammatory mediators is associated with symptoms like influenza. SARS-CoV2 was initially assumed to be primarily affecting the respiratory system, particularly the lower respiratory tract. The symptoms include fever, dry cough, nausea and diarrhoea which were reported initially in Wuhan, China [3]. But researchers reported that corona virus not only affects the respiratory system, but also the musculoskeletal and neurological systems as well. A systematic review conducted by Abdullahi A et al., suggested that SARS-CoV2 affects both neurological and musculoskeletal systems. This review reported that COVID-19 patients experienced symptoms such as myalgia, fatigue, injury to skeletal muscle and joint pain [4].
The mechanism of pain in people suffering from post-COVID-19 infection was suggested by Wu Y et al., that central pain can be caused through ACE2-positive cells in the human spinal cord by decreasing functional Angiotensin Converting Enzyme 2 (ACE2), resulting in Angiotensin II accumulation and decreasing Angiotensin 1-7. The effect of spinal ACE2 on pain sensation and the impact of direct or indirect tissue damage can result in the pain induced after infection with COVID-19, and the function of ACE2 in the transmission and management of pain in the infected patients needs to be further evaluated [5]. According to Stanford Hall Consensus statement for post-COVID-19 rehabilitation [6], potential rehabilitation needs are expressed at the individual level, particularly to cardiovascular, pulmonary, musculoskeletal, and neurological aspects. The rehabilitation is a patient-centred method and includes multiple components of biopsychosocial aspects of pain [6].
People with COVID-19 infection were managed in ICU by ventilator support. Prolonged periods of inactivity and steroids use have caused muscle atrophy, arthralgia, weakness in limbs and loss of balance in the affected population. There is a need for extensive physiotherapy sessions to reduce pain, improve muscle mass, and reduce balance issues in these populations [7]. But, COVID-19 survivors discharged from the hospital have high chances of getting infected again as the disease has no cure or vaccine till now. Halpin SJ et al., in his research conducted through telephone rehabilitation has found a beneficial effect of these sessions in bringing back the function of individuals who survived the infection [8]. As the pandemic seems like not going to end soon, recommendations have been suggested for musculoskeletal physiotherapists on how to rehabilitate COVID-19 survivors. This literature review aims to identify strategies to rehabilitate patients with post-COVID-19 infection.
Literature Search
This literature review was performed using PubMed and Google Scholar, with the following search words from January 2019 to September 2020: COVID-19 Corona Virus 2019, Sars-Cov2, Novel Corona virus, Musculoskeletal Physiotherapy and Recovery. Initially, the papers were screened by title and abstract in PubMed. The first 200 hits with appropriate title in Google Scholar and abstract were included in the analysis.
Inclusion criteria: Articles published in the last two years, intervention physiotherapy, and post-COVID-19 physiotherapy, Randomised control trials, Consensus Statements, Guidelines.
Exclusion criteria: Articles not concerning rehabilitation or Pulmonary or Cardiac Rehabilitation. The flowchart showing the selection of studies is given in [Table/Fig-1].
Flow diagram of articles reviewed.
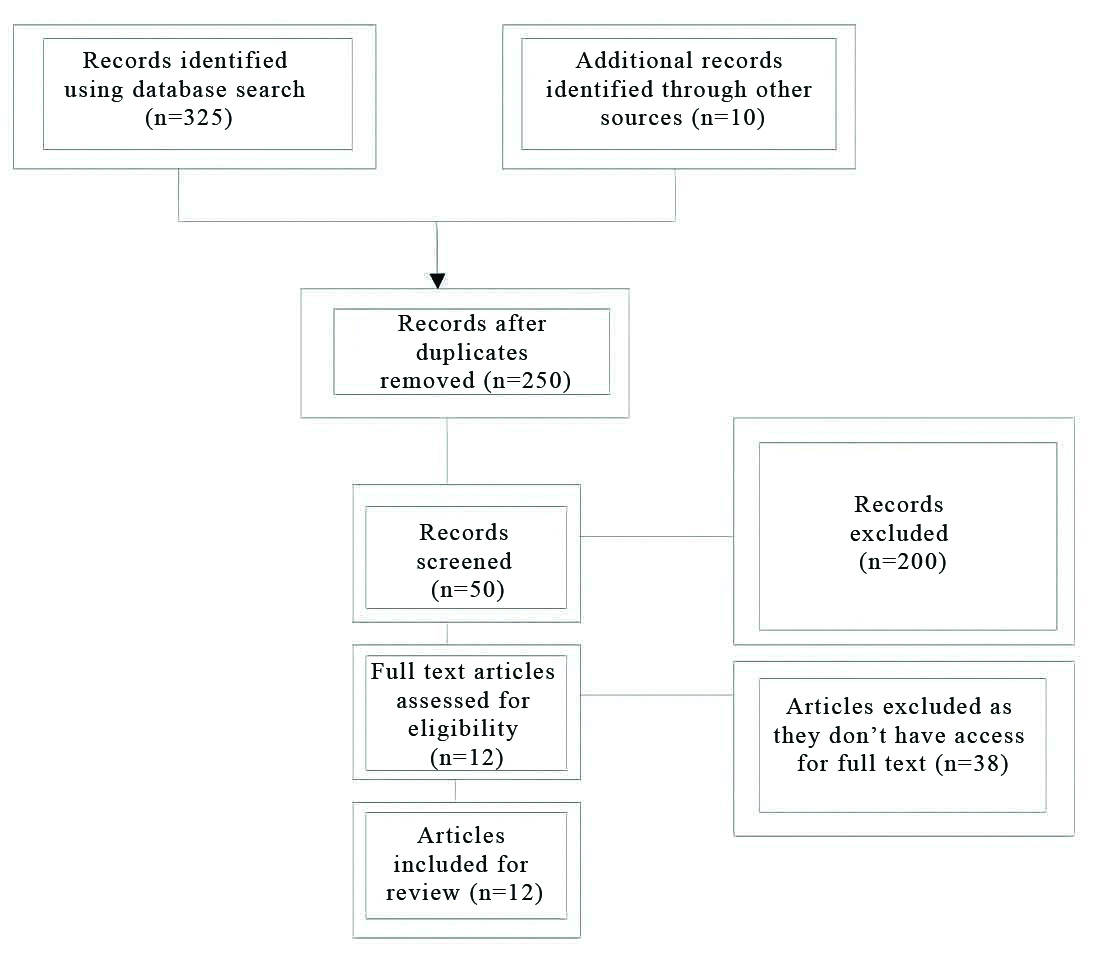
A total of 12 research papers satisfying the inclusion criteria were considered for literature review. After reviewing the papers, four themes, Telerehabilitation, Patient education, Pain management, and Self management were extracted from the articles. These articles stated the delivery of physiotherapy sessions for post-COVID-19 population.
Discussion
In order to help patients with musculoskeletal discomfort and postorthopaedic surgery recovery, physiotherapists use a combination of hands-off and hands on abilities. Manual therapy is a prime example of functional skills intended to minimise pain and enhance self- efficacy among individuals with pain. The hands-off practise has been recommended with the outbreak of COVID-19 and with social distancing requirements, manual therapy techniques cannot be delivered. Thus, these methods are highly useful to improve the quality of treatment and quality of life. So, in this unusual situation and high rehabilitation demands researchers have suggested few strategies in delivering physiotherapy sessions to maintain or improve physical function in individuals suffering with pain. These simple and effective strategies were recommended for rehabilitating individuals with post-COVID-19 infection to reduce the risk of re-infection and measures to improve the quality of treatment and health of post-COVID-19 infected individuals [Table/Fig-2] [4-15].
Outcome of included studies [4-15].
| Authors | Population | Intervention/Suggestions | Outcome/Conclusion |
|---|
| Abdullahi A et al., 2020 [4] | COVID-19 patients | Systematic review of clinical manifestations post-COVID-19 infection | The authors in their review summarised all the neural and musculoskeletal complications experienced by individuals in post-COVID-19 infection. |
| Wu Y et al., 2020 [5] | COVID-19 infection | COVID-19 infection and the pathology involved in the infection was explored by the authors | The authors concluded the Neuro and musculoskeletal systems involved in COVID-19 infection. |
| Barker-Davies RM et al., 2020 [6] | COVID-19 | The authors suggested rehabilitation guidelines in treating people with COVID-19 infection | The consensus statement have suggested guidelines in both assessing and treating musculoskeletal pain in post-COVID-19 infection. |
| Drozdzal S et al., 2020 [7] | COVID-19 | Pain management strategies in post-COVID-19 infection | The authors have suggested guidelines in managing pain among post-COVID-19 infected population. |
| Halpin SJ et al., 2021 [8] | Post-COVID-19 infection | The authors conducted a cross-sectional survey on individuals postdischarge | The authors concluded that individuals have reoccurrence of infection post discharge and rehabilitation strategies must be online based. |
| Turolla A et al., 2020 [9] | Review | The authors reviewed telerehabilitation methods and strategies involved in it. | The authors conclude that healthcare workers must be trained in telerehabilitation prior implementing. |
| Cottrell MA and Russell TG 2020 [10] | Patients with musculo-skeletal pain | The authors suggested telerehabilitation as a mode of rehabilitation of individuals in pain | The author concluded that telerehabilitation is effective in rehabilitating people with pain. |
| Mallari B et al., 2019 [11] | Chronic pain | The authors conducted a systematic review of virtual reality and its analgesic effect of people with chronic pain | The authors concluded that virtual reality is effective on acute pain than in chronic pain. |
| Laskowski ER et al., 2020 [12] | NA | Standardisation of telerehabilitation assessment of patients and testing methods. | The authors have standardised the methods of online examination of patients and testing criteria which can be utilised as easy methods of telerehabilitation. |
| Pugliese M and Wolff A, 2020 [13] | Post-COVID-19 infection | Patient education was recommended as one of the rehabilitative strategies for patients with post-COVID-19 infection | The authors recommended that, to have effective rehabilitation strategies and adherence to rehab protocol, patient education is mandatory. |
| Wang CC and Wolff A, 2020 [14] | Post-COVID-19 infection | Rehabilitative suggestions on musculoskeletal pain and recommendations of exercises in pain rehabilitation online | The authors concluded that telerehabilitation is one of the reliable method in rehabilitating patients with musculoskeletal pain during pandemic. |
| Demeco A et al., 2020 [15] | Post-COVID-19 infection | Rehabilitation strategies have been explained by the authors for COVID-19 infection, they focussed primarily on respiratory and cardiac functions | They concluded that rehabilitative strategies must include active exercises and cardiac and pulmonary rehabilitation. |
Telerehabilitation
The word ‘Telehealth’ is an umbrella term used by healthcare providers to identify the provision of healthcare at a distance, using Information and Communication Technology (ICT). The word telerehabilitation is often characterised in the field of physiotherapy as the provision of rehabilitation services through information and communication technologies [10]. Healthcare interaction is characterised by the option of incorporation of ICT, either synchronously or in real time. Asynchronous telehealth causes temporary delay between message sent and received by the person watching, including other ICT styles, smart watches, trackers, virtual reality, and telehealth operation [11].
Clinical Evidence on Telerehabilitation
The efficacy of telerehabilitation has been assessed by many researchers through their systematic reviews and Meta-analysis. Agostini M et al., have conducted systematic review and meta-analysis on the efficacy of telerehabilitation on various musculoskeletal and arthroplasty surgeries and they have concluded that telerehabilitation had positive benefits on rehabilitation methods [16]. Practical telerehabilitation has a beneficial effect on pain relief, enhancing joint range of motion, muscle strength, functional tasks, and impairment in the sense of physiotherapy. Telerehabilitation has either similar or higher importance in comparison with face to face usual care in physiotherapy [9].
Moreover, the effects of telerehabilitation as standalone care have been investigated in people with chronic musculoskeletal pain. Thus, evidence suggests that telerehabilitation can be used as a substitute to face-to-face intervention for reducing disabilities caused due to pain [10]. The feasibility of telerehabilitation based consultation for MSK pain has been reported. It has validity, good interrater and intrarater reliability in the assessment and management of various conditions leading to pain. Lower validity and reliability have been identified in the assessment of shoulder, elbow joints, scar assessment of knee and evaluation of lumbar spine postures. Due to the absence of a standard error of measurement and coefficient of variation, these findings cannot be generalised [16].
Opportunities in Telerehabilitation during and post-COVID-19
Despite its wide benefits, the utility of telerehabilitation was slow until COVID-19. The surge of telerehabilitation has taken place; most clinics and hospitals adopted this method. Significant efforts have been made to understand the usage of telerehabilitation services, which included infrastructure changes, obtaining new ICT enabled consultations. The advancement of technology for consumers both in software and hardware was supported by numerous funding bodies. Thus, telerehabilitation changed the way in offering services during the pandemic in 2019 [10]. The majority of literature published on telehealth has been focused on the perspective of the clinician regarding the success and failure of telerehabilitation services. Factors like patient efficacy towards technology, patient privacy, and safety concerns have been cited. Telehealth requires both the clinician and the patient to be reliant on each other in delivering and adhering to appropriate care [10].
These adaptive strategies of healthcare providers towards telehealth were challenged by online communication skills, patient environment, and the platform used [10]. Recent studies have demonstrated strategies to overcome the challenges faced by health providers by specific training towards the assessment and treatment of people with MSK pain [10]. Strict social distancing norms adhered by the organisations led to a rapid increase in uptake of telehealth and cut through many traditional barriers. This rapid shift is the only option to treat people with adequate distancing and home-based rehabilitation. Many healthcare professionals started treating people with pain and post-COVID-19 infection.
Assessment and Rehabilitation of Individuals using Telehealth Post-COVID-19
Geriatric population people must be advised to continue or take upon a physical activity that reflects the current guidelines. Programs must include a mix of strength, balance, and aerobics. According to the Mayo clinic’s report, they have recommended the assessment procedures in Physiotherapy. The physiotherapist’s assessment contains Range of motion examination, muscle strength, flexibility, balance and others as examination components. These simple observation procedures have been recommended for telerehabilitation as people with post-COVID-19 infection have to be treated online and face to face physiotherapy sessions are not indicated. These virtual guidelines in examination help physiotherapists and other clinical practitioner’s to examine musculoskeletal components [12].
Patient Education
Patient-centric care in Physiotherapy is essential in delivering effective care. These include effective communication, education, and self-management strategies taught to the patients to make them an active member of the rehabilitation team than receiving passive care. Telerehabilitation is a patient-centric method, emphasising on active strategies [13]. Without patient education, rehabilitation is incomplete. Education of an individual is intended to improve understanding and builds confidence which is an important factor for home rehabilitation, built on effective communication, a thorough explanation of symptoms, mechanism, and management plan and includes teaching and counselling to modify behaviour. Proper education is a first line intervention that empowers knowledge, reduces fear and assures the patients for a speedy recovery [13].
The telehealth model is used in delivering these components of education to the patient and to prepare the individual for the further rehabilitation process. The remote sessions offers a concentrated, distraction free care and allow the patient to acquire good communication and proper education. An increased ability to focus leads to greater comfort between the clinician and the patient, which can lead to higher satisfaction and a better outcome. Knowledge empowers patients to maximise compliance as this is very crucial in treating musculoskeletal pain, as beliefs regarding the condition may restrict the adherence to rehabilitation measures [10]. Therapists while using telerehabilitation to educate a patient must follow vocal instructions, hand written and physical demonstration during sessions and must explain anatomy, physiology and exercise positions; metaphors and analogies are encouraged to help a patient in understanding the contexts better. Hand written material should have clear letters and avoid technical texts, graphs and cluster. Effective techniques include repetition, spacing and multiple sessions to deliver the contexts to people and make them aware of the self-care methods [10,13].
Self-Management
Self-management includes a treatment framework that is patient-driven, with tools of self-management and a patient’s home as a therapy setting. Each of these tasks will contribute to a greater sense of responsibility and provides patients direction to reach their individuals’ goals actively. Providing advice on self-management can increase self-efficacy, coping strategies and instil belief in an individual that they have control over their symptoms [13,16].
Pain-related self-efficacy and locus of control are critical factors associated with outcomes in individuals with musculoskeletal pain. Patients with chronic pain must understand that short term solutions are a sustainable approach; they have to be educated and taught long term self-management strategies. The therapists must address active lifestyle strategies to manage musculoskeletal pain [13]. Instead of relying on physical examination, patients must be taught on active management approaches like exercises, functional activity training, and behavioural changes. This approach shifts the control of treatment to the patient, thus, making them a part of the treatment plan and by achieving self-monitoring and self-management [13].
Pain Management
Recommendations of pain management in post-COVID-19 infections have been given and they help in reducing acute pain and improve self-care in people with pain.
RICE (Rest, Icing, Compression and Elevation)
During the initial injury stage, tissue damage causes inflammatory reactions. People with post-COVID-19 pain are recommended to use RICE (Rest, Icing, Compression and Elevation), although cold can be replaced by heat as it improves vascularisation. However, the cold therapy is more suitable in reducing pain [14,15].
Exercise
Exercise in the phase of post-COVID-19 recoveries will reduce the severity in pain. The effects of immobilisation in ICU is not long-lasting. Individuals post-COVID-19 recovery must be instructed to stay active and activities like free exercises resisted training must be encouraged to counter the negative effects of atrophy and bring the muscle mass back to normal [8,15].
Conclusion(s)
Considering the high number of cases and people affected with COVID-19 infection, post-COVID-19 infection rehabilitation is very important to counter the negative effects of the disease and to improve the quality of life in individuals. But, people recovering or who have recovered from this disease are susceptible to re-infection. Recommending those vulnerable patients to undergo a face to face physiotherapy session is not advisable. So, that vulnerable population must be rehabilitated with offline strategies to improve function and quality of life. To reduce the burden of the disease, both Physiotherapists and patients have to adapt to the technologies faster to counter the negative effects of this unfrequented pandemic situation.
[1]. Xu T, Chen C, Zhu Z, Cui M, Chen C, Dai H, Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19Int J Infect Dis 2020 94:68-71.10.1016/j.ijid.2020.03.02232179140 [Google Scholar] [CrossRef] [PubMed]
[2]. Hu Z, Yang Z, Li Q, Zhang A, Huang Y, Infodemiological study on COVID-19 epidemic and COVID-19 InfodemicPreprints 2020 2020:202002038010.2196/preprints.19135 [Google Scholar] [CrossRef]
[3]. Yuki K, Fujiogi M, Koutsogiannaki S, COVID-19 pathophysiology: A reviewClin Immunol 2020 215:10842710.1016/j.clim.2020.10842732325252 [Google Scholar] [CrossRef] [PubMed]
[4]. Abdullahi A, Candan SA, Abba MA, Bello AH, Alshehri MA, Afamefuna Victor E, Neurological and musculoskeletal features of COVID-19: A systematic review and meta-analysisFrontiers in Neurology 2020 11:68710.3389/fneur.2020.0068732676052 [Google Scholar] [CrossRef] [PubMed]
[5]. Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Nervous system involvement after infection with COVID-19 and other coronavirusesBrain Behav Immun 2020 87:18-22.10.1016/j.bbi.2020.03.03132240762 [Google Scholar] [CrossRef] [PubMed]
[6]. Barker-Davies RM, Sullivan OO, Pumi K, Senaratne P, Baker P, Cranley M, The Stanford Hall consensus statement for post COVID-19 rehabilitationBritish Journal of Sports Medicine 2020 54:949-59.10.1136/bjsports-2020-10259632475821 [Google Scholar] [CrossRef] [PubMed]
[7]. Drozdzal S, Rosik J, Lechowicz K, Machaj F, Szostak B, Majewski P, COVID-19: Pain management in patients with SARS-CoV-2 infection-molecular mechanisms, challenges, and perspectivesBrain Sci 2020 10(7):46510.3390/brainsci1007046532698378 [Google Scholar] [CrossRef] [PubMed]
[8]. Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluationJ Med Virol 2021 93(2):1013-22.Epub ahead of print10.1002/jmv.2636832729939 [Google Scholar] [CrossRef] [PubMed]
[9]. Turolla A, Rossettini G, Viceconti A, Palese A, Geri T, Musculoskeletal physical therapy during the COVID-19 pandemic: Is telerehabilitation the answer?Phys Ther 2020 100(8):1260-64.10.1093/ptj/pzaa09332386218 [Google Scholar] [CrossRef] [PubMed]
[10]. Cottrell MA, Russell TG, Telehealth for musculoskeletal physiotherapyMusculoskelet Sci Pract 2020 48:10219310.1016/j.msksp.2020.10219332560876 [Google Scholar] [CrossRef] [PubMed]
[11]. Mallari B, Spaeth EK, Goh H, Boyd BS, Virtual reality as an analgesic for acute and chronic pain in adults: A systematic review and meta-analysisJ Pain Res 2019 12:2053-85.10.2147/JPR.S20049831308733 [Google Scholar] [CrossRef] [PubMed]
[12]. Laskowski ER, Johnson SE, Shelerud RA, Lee JA, Rabatin AE, Driscoll SW, The telemedicine musculoskeletal examinationMayo Clinic Proc [Internet] 2020 95(8):1715-31.Available from: https://doi.org/10.1016/j.mayocp.2020.05.02610.1016/j.mayocp.2020.05.02632753146 [Google Scholar] [CrossRef] [PubMed]
[13]. Pugliese M, Wolff A, The value of communication, education, and self-management in providing guideline-based care: Lessons learned from musculoskeletal telerehabilitation during the COVID-19 CrisisHSS J 2020 16(1):160-63.10.1007/s11420-020-09784-232837411 [Google Scholar] [CrossRef] [PubMed]
[14]. Wang CC, Chao JK, Chang YH, Chou CL, Kao CL, Care for patients with musculoskeletal pain during the COVID-19 pandemic: Physical therapy and rehabilitation suggestions for pain managementJ Chin Med Assoc 2020 83(9):822-24.10.1097/JCMA.000000000000037632618600 [Google Scholar] [CrossRef] [PubMed]
[15]. Demeco A, Marotta N, Barletta M, Pino I, Marinaro C, Petraroli A, Rehabilitation of patients post-COVID-19 infection: A literature reviewJ Int Med Res 2020 48(8):01-10.10.1177/030006052094838232840156 [Google Scholar] [CrossRef] [PubMed]
[16]. Agostini M, Moja L, Banzi R, Pistotti V, Tonin P, Venneri A, Telerehabilitation and recovery of motor function: A systematic review and meta-analysisJ Telmed 2015 21(4):202-13.10.1177/1357633X1557220125712109 [Google Scholar] [CrossRef] [PubMed]