Poststreptococcal Glomerulonephritis (PSGN) is an acute inflammation of renal glomerular parenchyma and is sequelae of pharyngitis or skin infection caused by nephritogenic strains of group A beta-Haemolytic Streptococcus. PSGN is conventionally diagnosed based upon clinical findings and demonstration of recent streptococcal infection by a positive skin/throat culture or serologic tests. Hereby, authors present a case of PSGN in an 18-year-old normotensive male is reported who presented with anasarca. On evaluation, the patient had subnephrotic range proteinuria without haematuria and normal serum creatinine. Concealed healing skin lesions in the gluteal region, suggestive of impetigo were noted and hence, arrived at the diagnosis of PSGN. He was treated with intravenous antibiotics, following which symptoms improved. Young patients with acute presentation of oedema or proteinuria with possible renal cause warrants thorough head to foot examination for unseen skin lesions in otherwise overlooked areas. PSGN responds promptly with early antibiotic therapy.
Group A beta-Haemolytic Streptococcus, Impetigo, Pharyngitis, Proteinuria
Case Report
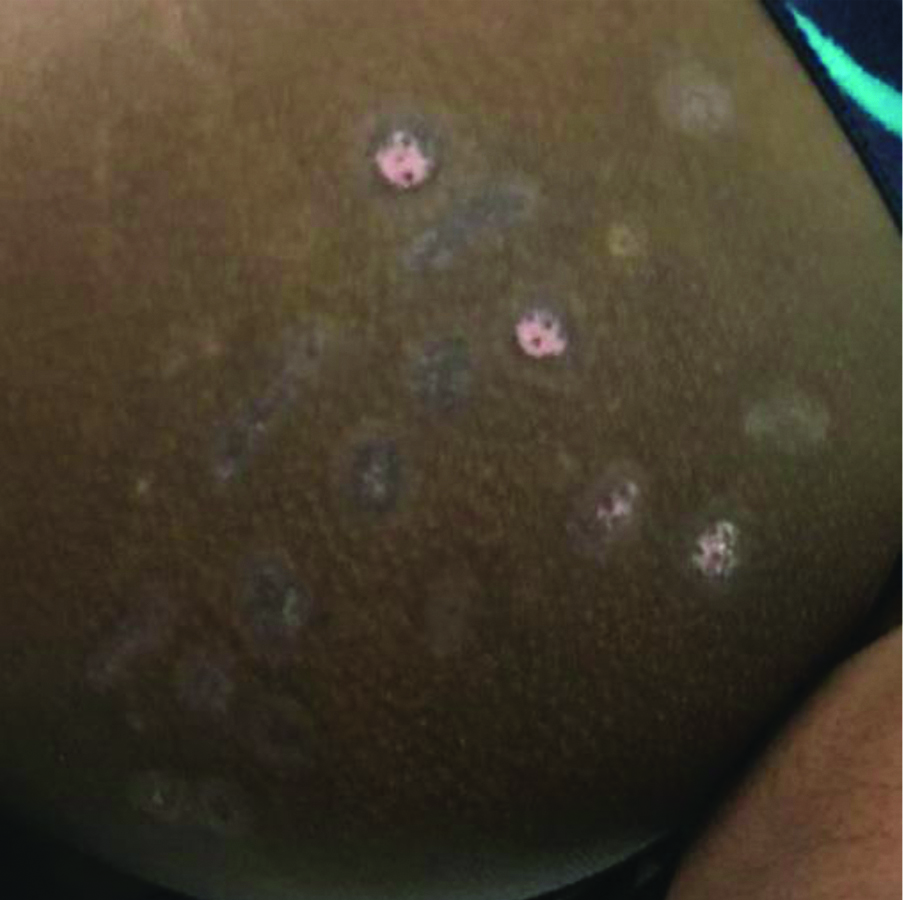
An 18-year-old male patient presented with complaints of early morning facial puffiness followed by swelling of upper limbs, lower limbs and abdomen for four days. He had no history of sore throat, fever, haematuria, or oliguria. Patient had no history of anti-inflammatory drugs, steroids, tobacco, or alcohol abuse. He had no medical co-morbidities. He had no history of any surgeries in the past. On examination, generalised anasarca was present along with bilateral pitting pedal oedema. Head to foot examination revealed concealed skin lesions in the bilateral gluteal region, suggestive of impetigo [Table/Fig-1].
Shows multiple erythaematous macular rashes in the bilateral gluteal region.

His Pulse Rate (PR) was 76/min and Blood Pressure (BP) recorded in the right upper limb in sitting posture was 110/80 mmHg. Abdomen was soft, distended, no tenderness, free fluid was present. Complete blood count was within normal limits. Renal function tests showed normal levels of blood urea nitrogen (14 mg/dL) and serum creatinine (0.9 mg/dL). Serum electrolytes were normal (sodium 134 mmol/L, potassium 3.8 mmol/L, chloride 104 mmol/L, bicarbonate 22 mmol/L). Serum albumin was decreased (3.3 g/dL). Other liver function test parameters were normal. Thyroid function tests within normal limits. Urine tests showed Red Blood Cells (RBC) 1-2 cells/hpf, no cast, and urine proteins was 3+. Urine protein/creatinine ratio was increased (0.8). A 24-hour urine protein was 1432 mg/day, which is in the subnephrotic range. Antistreptolysin O (ASO) titer was 234 IU/mL, C-reactive protein was 11 mg/L. Antinuclear Antibody (ANA) by immunofluorescence was negative. Viral markers for hepatitis B, C, and Human Immunodeficiency Virus (HIV) were negative. Lipid profile was normal. Complement levels were low, C3 was 25.3 mg/dL (normal 90-180 mg/dL), C4 was 7.2 mg/dL (normal 10-40 mg/dL).
Electrocardiogram (ECG) showed normal sinus rhythm. Chest x-ray was normal. Ultrasound abdomen showed thickened gallbladder likely to be reactive, mild splenomegaly and mild ascites. Ultrasound venous doppler of the lower limbs was negative of deep vein thrombosis. Anasarca in a young male with healing, crusted skin lesions suggestive of impetigo, which on further evaluation revealed subnephrotic range proteinuria and low C3/C4 level narrowed the diagnosis to atypical presentation of post-infective glomerulonephritis. Other differentials include IgA nephropathy where the classical presentation is synchronous upper respiratory tract infection with recurrent episodes of gross haematuria and proteinuria; minimal change disease and vasculitis. Since the patient had an antecedent skin lesion in a concealed site followed by proteinuria, most likely diagnosis is postinfectious glomerulonephritis (atypical presentation). The patient was treated with Intravenous (IV) antibiotics (Inj. amoxicillin 1000 mg + clavulanic acid 200 mg) for seven days. Daily weight monitoring with target weight reduction of 0.5-1 kg/day, strict input-output chart, restricted salt <6 g/day was done. Intravenous diuretics Inj. furosemide 20 mg once daily was given. Patient weight gradually reduced from baseline 68 kg to 64 kg on discharge.
Hence, the patient was discharged with oral antibiotics. On follow-up after four weeks, the skin lesions over the gluteal region healed, oedema reduced and the patient’s weight gradually reduced from baseline 68 kg to 52 kg after four weeks [Table/Fig-2]. Urine routine showed no evidence of protein or cast.
Shows the resolution of size lesions after four weeks of treatment.
Discussion
Following the infection, there is rapid deterioration of kidney function due to deposition of immune complexes. It is more common in children. PSGN presents with haematuria, hypertension, oedema, proteinuria, and oliguria. Rarely, it can present as nephrotic syndrome with nephrotic range proteinuria. In children, the prognosis is very favourable, but residual renal impairment may cause poor prognosis in adults [1]. The yearly incidence of new cases of PSGN range from 8.5 to 28.5 per 100000 individuals [2] and it is important to note that around 97% of such patients live in underprivileged countries [1,2].
Classic triad of PSGN includes oedema, haematuria, and hypertension. However, patients with PSGN occasionally present with unusual clinical symptoms that often lead to delayed or misdiagnosis of the disease and increased morbidity. The usual presenting symptom being gross haematuria occurs in 30-50% of cases with acute PSGN [2]. Subclinical cases of PSGN are primarily characterised by microscopic haematuria. PSGN is usually associated with hypertension. Berry S et al., observed association of hypertension in 69.1% of cases [3]. Puri RK et al., found hypertension in 74.6% of cases [4]. Hypertension was found in 82% of cases by Rajajee S, and 18% of PSGN patients were non-hypertensive [5]. Proteinuria is usually in the mild subnephrotic range however, nephrotic range proteinuria (>3.5 g/24 hours) is rare and seen only in 5% of cases [2]. Proteinuria generally resolves within 6 to 8 weeks. PSGN is usually characterised by low C3 levels and normal C4 levels [2]. In the study by Moroni G et al., C3 was low in 71% of the 48 patients tested, whereas C4 was low in 15% [6].
The patient had unusual and interesting presentation: 1) anasarca without hypertension; 2) absence of haematuria; 3) occurrence of renal insult (postinfectious glomerulonephritis) when skin lesions didn’t resolve completely, highlighting the short latency observed in this patient; 4) subnephrotic range proteinuria resolved completely within a short span of four weeks; 5) complement levels C3 and C4 both on the lower side is quite rare in PSGN. This report also emphasises complete search for skin lesions in hidden areas like the gluteal region.
PSGN is a renal disease that develops 10 to 14 days after a skin or throat infection, it is not caused by the bacteria itself, but by the body’s immune system. Popovic-Rolovic M, found preceding infection of respiratory tract in 82%, skin infection in 10%, and no infection in 8% of cases [7]. PSGN is conventionally diagnosed based upon clinical findings and demonstration of a recent group A beta-haemolytic streptococcal infection by either a positive skin or throat culture/serologic tests. However, a low C3 and total complement level are consistent with a diagnosis of PSGN, it can also be decreased in other forms of glomerulonephritis [2].
A renal biopsy may be required to differentiate PSGN from Membranoproliferative Glomerulonephritis (MPGN), IgA vasculitis, IgA nephropathy and lupus nephritis [5]. Patients with MPGN continue to have continual elevation in serum creatinine, hypocomplementemia and urinary abnormalities beyond four to six weeks [2]. Secondary causes of glomerulonephritis such as lupus nephritis and IgA vasculitis present similar features to PSGN. However, extrarenal manifestations of these underlying systemic diseases should be useful to exclude the possibility of PSGN. Indications of renal biopsy in PSGN are nephrotic range proteinuria in acute stage, normal serum complement, prolonged hypocomplementemia and long-lasting proteinuria [2]. The patient responded to IV antibiotics, hence renal biopsy was deferred.
Treatment is conservative. Well-documented PSGN should be treated with penicillin, or erythromycin if the patient is allergic to penicillin, usually for a period of 10 days to resolve streptococcal infection and prevent the spread of the nephritogenic streptococcus among contacts. Acute PSGN is prevented by early antibiotic treatment, and the spread of streptococcal infection is controlled by prophylactic antibiotic treatment to individuals at risk [8].
Poststreptococcal Glomerulonephritis (PSGN) is usually self-limiting. However, in few patients, it might lead to chronic renal failure. Other complications of PSGN include acute renal failure, chronic glomerulonephritis, hyperkalaemia, hypertension, pulmonary oedema, nephrotic syndrome, posterior reversible leukoencephalopathy and immune-mediated pneumonitis. Patients with an acute nephritic syndrome are advised to restrict sodium and fluid intake. The role of intravenous steroids, immunosuppression and anticoagulation in treatment of PSGN remains unproven [8].
Follow-up of PSGN patients includes monitoring BP and renal function tests; to check serum complement levels at 6-8 weeks to confirm that they have returned to normal; to check urine for haematuria and proteinuria every 3-6 months [2]. On follow-up, four weeks later the index patient had complete resolution of proteinuria, normal complement (C3, C4) levels, BP was within normal range.
Conclusion(s)
PSGN is an immune-mediated disease with a favourable prognosis. Thorough search for antecedent infection elsewhere in the body, if not obvious helps in arriving at the diagnosis in younger patients with either proteinuria or haematuria. Early diagnosis and appropriate antibiotics helps in reducing long term renal complications.
[1]. Rodriguez-Iturbe B, Musser JM, The current state of poststreptococcal glomerulonephritisJ Am Soc Nephrol 2008 19(10):1855-64.10.1681/ASN.200801009218667731 [Google Scholar] [CrossRef] [PubMed]
[2]. Rawla P, Padala SA, Ludhwani D, Poststreptococcal GlomerulonephritisIn: StatPearls [Internet] 2020 Treasure Island (FL)StatPearls Publishing [Google Scholar]
[3]. Berry S, Prakash K, Srivastava G, Gupta S, Acute glomerulonephritis in childrenIndian Pediatr 1971 8(5):198-200. [Google Scholar]
[4]. Puri RK, Khanna KK, Raghu MB, Acute glomerulonephritis in childrenIndian Pediatr 1976 13(9):707-11. [Google Scholar]
[5]. Rajajee S, Poststreptococcal acute glomerulonephritis: A clinical, bacteriological and serological studyIndian J Pediatr 1990 57(6):775-80.10.1007/BF027222752131308 [Google Scholar] [CrossRef] [PubMed]
[6]. Moroni G, Pozzi C, Quaglini S, Segagni S, Banfi G, Baroli A, Long-term prognosis of diffuse proliferative glomerulonephritis associated with infection in adultsNephrol Dial Transplant 2002 17(7):1204-11.10.1093/ndt/17.7.120412105242 [Google Scholar] [CrossRef] [PubMed]
[7]. Popovic-Rolovic M, Serum C3 levels in acute glomerulonephritis and postnephritic childrenArch Dis Child 1973 48(8):622-26.10.1136/adc.48.8.6224205832 [Google Scholar] [CrossRef] [PubMed]
[8]. Rodriguez-Iturbe B, Haas M, Poststreptococcal Glomerulonephritis. In: Ferretti JJ, Stevens DL, Fischetti VA (eds)Streptococcus pyogenes: Basic Biology to Clinical Manifestations [Internet] 2016 Oklahoma CityUniversity of Oklahoma Health Sciences Center [Google Scholar]