Angioleiomyoma of the Uterus with Extensive Hyaline Degeneration- A Rare Case Report with Brief Review of Literature
Devi Subbarayan1, Vijayashree Raghavan2, Priyadharshini Kumar3, Vijayalakshmi Kandasamy4
1 Associate Professor, Department of Pathology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
2 Head, Department of Pathology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
3 Postgraduate Student, Department of Pathology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
4 Professor, Department of Obstetrics and Gynaecology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Devi Subbarayan, D Block, Department of Pathology, CHRI, Chennai, Tamil Nadu, India.
E-mail: sdevi2001@gmail.com
Angioleiomyoma (AL) or vascular leiomyoma is a distinct variant of leiomyoma with prominent vascular component, usually occurs in extremities and very rarely arise in internal organ. It has been documented in female genital tract including cervix, uterus, ovary and broad ligament. Uterine leiomyoma is very rare and is a distinct variant of conventional leiomyoma which has prominent vascular component. The diagnosis of this variant requires histopathological examination since it does not have specific clinical and radiological features unlike in soft tissues where it presents as subcutaneous painful swelling. Like conventional leiomyomyoma, AL can also undergo degenerative changes like hyalinisation, infarction, calcification and myxoid change. Here, a rare case of uterine AL with ovarian seromucinous cystadenoma is reported in a 38-year-old female who was diagnosed incidentally when she was evaluated for abnormal uterine bleeding. Magnetic Resonance Imaging (MRI) pelvis revealed a intramural fibroid of size 5×4.5 cm noted in anterolateral myometrium of uterus and a large multiloculated cystic lesion of size 12.5×12.5×8.8 cm seen arising from left ovary. Abdominal hysterectomy was done. Grossly, sectioning of myometrium showed well-circumscribed grey white to grey brown intramural fibroid measuring 4.5×3.5 cm. Histologically the lesion showed fascicles of spindle cells swirling around the thick walled blood vessels and immunohistochemically these cells were positive for Smooth Muscle Actin (SMA). Here, this rare case of uterine AL with brief review of literature is reported.
Histology, Leiomyoma, Smooth muscle actin, Uterine bleeding
Case Report
A 38-year-old P3L3A1 with known diabetes and HBsAg positive female presented to the Gynaecology Department with history of menorrhagia and lower abdominal pain for one month duration. On clinical examination, she was anaemic. Her uterus was enlarged 10-12 weeks size. Cervix and vagina were healthy on per speculum examination. Per vaginal examination, uterus was anteverted, mobile, bulky. MRI pelvis (contrast) revealed intramural fibroid of size 5×4.5 cm noted in anterolateral myometrium of uterus and a large multiloculated cystic lesion of size 12.5×12.5×8.8 cm seen arising from left ovary, no significant contrast enhancement or internal calcification noted.
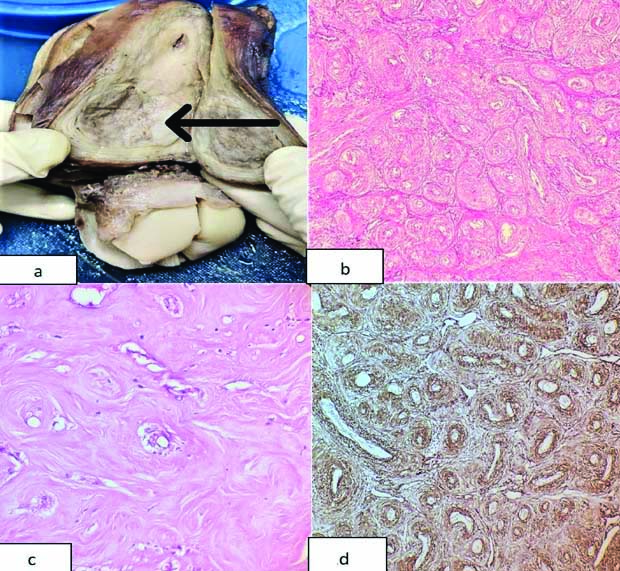
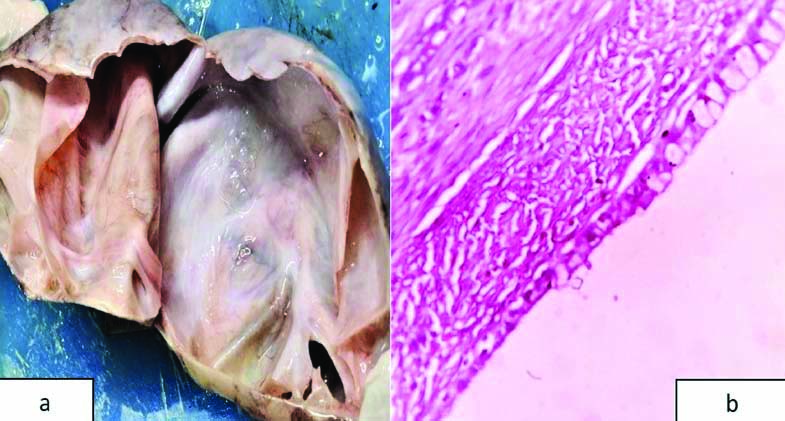
Based on clinical features and radiological findings, provisional diagnoses of leiomyoma with complex ovarian cyst was made, for which abdominal hysterectomy with left salpingo-oophorectomy was performed. The specimen was sent for histopathological examination. Grossly, uterus was asymmetrically enlarged, measuring 12×7×4.5 cm, left ovary measured 12×10×4 cm. On serial sectioning of myometrium showed well-circumscribed intramural fibroid measuring 4.5×3.5 cm and posterior wall fibroid measuring 2.5 cm in diameter. Cut section of intramural fibroid appeared grey white to grey brown with areas of whorling [Table/Fig-1a]. Cut section of the left ovarian cyst was multiloculated filled with viscous mucinous material. Microscopically, the intramural fibroid showed well-circumscribed fascicles of spindle cells swirling around the thick walled blood vessels with areas of hyalinisation [Table/Fig-1b,c]. No atypia, mitoses or necrosis noted. Based on the above histological features, possibilities of AL, Angiomyolipoma (AML) and uterine stromal tumours were considered in the differential diagnoses. On extensive sampling of tumour, lipomatous component was not found. Hence, AML was ruled out and immunohistochemically, it was proceeded with SMA and CD10. The tumour cells exhibited strong cytoplasmic positivity for SMA [Table/Fig-1d] and negative for CD10 which confirmed it as AL. Section from the ovarian cyst was lined by serous and tall columnar mucin secreting epithelium with an underlying fibrocollagenous stroma [Table/Fig-2a,b]. A final diagnosis of AL of uterus with seromucinous cystadenoma of left ovary was rendered.
a) Gross photomicrograph of uterus showing well-circumscribed grey brown tumour with focal grey white area (arrow); b) Microscopic image showing well-circumscribed fascicles of smooth muscle swirling around the thick walled blood vessels (Hematoxylin & Eosin, 10x); c) Showing hyalinisation (Hematoxylin & Eosin, 20x); d) Immunohistochemistry tumour cells show strong positivity for Smooth Muscle Actin (SMA) (20x).
a) Gross photomicrograph of ovary shows multiloculated cyst; b) Microscopic image of cyst is lined by tall columnar mucin secretion epithelium and ciliated cuboidal epithelium with underlying fibrocollagenous stroma. (Hematoxylin & Eosin, 40x).
Discussion
The AL is rare benign mesenchymal tumour which arises from smooth vessels with prominent vascular component. It usually occurs in extremities as a painful lesion in middle aged women. Its occurrence in the uterus is very rare and it represents 0.3-0.4% cases of uterine leiomyoma [1-3]. Apart from uterus, cervix, ovary and broad ligament, AL has been reported in the female genital tract [2]. Though, it has a prominent vascular component, no specific clinical or radiological findings that help to distinguish it from conventional leiomyoma is available. Hence, the diagnosis mainly relies on histopathological examination.
Usual presentation of uterine AL, like conventional leiomyoma depending on the location and size of the tumour, it can present as menorrhagia, dysmenorrhea and abdominal lump, sometimes anaemia may be initial presentation because of bleeding. Other rare clinical presentations include DIC, hyperfibrinogenemia, raised CA125 levels and pseudo Meigs syndrome [4-8]. Few researchers have stated that, expression of abnormal growth factors such as basic fibroblast growth factor and its receptor can lead to abnormal vascular morphology and regulate angiogenesis resulting in abnormal uterine bleeding and anaemia in these cases [2]. Very rarely, the tumours can undergo spontaneous rupture due to its high vascularity and present as emergency [8]. Size of these tumour usually ranges from 4-30 cm, Pierro A et al., reported a case of giant AL measuring 32 cm in dimension occupying entire abdomen [9]. Recently, a case of gaint superinfected uterine AL with distant septic metastasis has been reported by Sanchez-Iglesias JL et al., [10]. Histologically, AL is classified into capillary type, venous type and cavernous channels based on the vascular caliber and amount of smooth muscle present in the tumour. The present case is of venous type wherein smooth muscle cells swirls around thick walled blood vessels, compared to conventional leiomyoma where blood vessels are predominantly of capillary type sometimes small arterioles are seen. AL is usually benign in nature and do not show any pleomorphism, mitosis or necrosis. Thomas S et al., have reported atypia and giant cells in their AL cases [4]. Like conventional leiomyomyoma, AL can also undergo degenerative changes such as infarction, hyalinisation, calcification and myxoid change [1]. This case showed extensive hyalinisation. Few studies have reported mucoid areas and fibrin deposits. Epithelioid variant sometimes mimic like glomangiomyoma or glomus tumour. Immunohistochemically, the tumour cells usually expresses SMA, desmin and h-caldesmon [Table/Fig-3] [1-10].
Cases of uterine Angioleiomyoma (AL) reported so far in the literature [1-10].
| Author name and year | Clinical features | Differential diagnosis | Final diagnosis based on histopathological and immunohistochemistry |
|---|
| Garg G and Mohanty SK, 2014 [1] | Middle aged women, complaints of menorrhagia, abdominal pain, abdominal mass | Intramural or sub serosal nodules,Endometrial stromal nodule,Angiomyo-fibroblastoma,Perivascular epithelial cell tumour | Angioleiomyoma |
| Sikora-Szczesniak DL, 2016 [2] | 9 patients, mean age 47.1±5 years | Fibroid uterus,Fibroma, Angiofibroma,Angiolipoma, andAngiomyofi-broblastoma | Six were intramural angioleiomyoma (66.7%) and three were subserosal angioleiomyoma (33.3%). |
| Gorginzadeh M et al., 2020 [3] | 41 years female, G4P3A1, Persistent vaginal bleeding following abortion, ultrasound shows a 3×3 cm mass in uterine cavity | Retained products of conception | Angioleiomyoma |
| Thomas S et al., 2012 [4] | 47 years female complains of abdominal distention for 1 year accompanied by pain, menorrhagia, dyspepsia and weight loss. Examination revealed a massive ascitis | Ovarian tumour,Uterine sarcoma | Angioleiomyoma |
| Hong JA et al., 2003 [5] | 33-year-old unmarried woman, complaints of vaginal bleeding, headache, vertigo, and vomiting. USG and CT revealed a huge uterine leiomyoma about 14.2 cm in its longest length | Leiomyoma | Angioleiomyoma |
| Hsieh CH et al., [6]. | 50-year-old, nulligravid,complains of menorrhagia for 3 years and progressively palpable lower abdominal mass for a half year. (CT showed that a huge 30-cm heterogeneously multilobulate mass with solid and laminated configuration, with cystic and multiseptal contents was found in left lower abdomen and pelvic cavity. | Leiomyoma | Multiple Angioleiomyoma |
| Handler M et al., 2012 [7] | 38-year-old nulligravida, complaints of abdominal swelling, menorrhagia for 10 years, which was aggravated for the past 4 months with clots and cramping pain | Malignant tumour with consumptive coagulopathy | Angioleiomyoma |
| Culhaci N et al., 2006 [8] | 45-year-old multigravida complains of lower abdominal pain, nausea, vomiting. | Leiomyoma like ruptured mass with vascular structures originating from uterine fundus | Angioleiomyoma |
| Pierro A et al., 2018 [9] | 37-year-old female, complains of abdominal distention, menorrhagis and dyspepsia for a period of 1 year | Giant uterine angioleiomyoma | Angioleiomyoma |
| Sánchez-Iglesias JL et al., 2019 [10] | Perimenopausal women, complaints of fever, abdominal pain and distention. | Endometrial stromal sarcoma | Giant angioleiomyoma superinfected by S. agalactiae with development of distant specific metastasis |
| Present case (2021) | 38-year-old P3L3A1 with known daibetes and HBsAg positive female, menorrhagia and lower abdominal pain for one month duration | Angioleiomyoma, Angiomyolipoma (AML) and uterine stromal tumours | Angioleiomyoma of uterus with seromucinous cystadenoma |
The histologic differential diagnoses included endometrial stromal tumours, perivascular epithelioid cell tumours and angiomyofibroblastoma. Though each of these has characteristic histologic findings at times overlapping microscopic features or epithelioid variant may warrant panel of IHC markers to confirm the diagnosis. Endometrial stromal tumours will be positive for CD10, perivascular epithelioid cell tumours will show HMB45, MART-1 positivity. Since it’s benign nature, complete excision of the tumour is the mainstay of treatment especially in women who want to retain their fertility or hysterectomy may be warranted for those who have completed family or in postmenopausal women.
Conclusion(s)
The AL is a distinct variant of uterine leiomyoma, with characteristic morphology and immunohistochemistry findings. Due to its vascular nature, clinically it can present as abnormal uterine bleeding, anaemia and sometimes it can undergo spontaneous uterine rupture with life-threatening bleeding. Due to increasing incidence of this entity and clinical relevance, it should be included as a distinct variant of leiomyoma in the WHO classification.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 19, 2020
Manual Googling: Jan 29, 2021
iThenticate Software: Mar 19, 2021 (11%)
[1]. Garg G, Mohanty SK, Uterine angioleiomyoma: A rare variant of uterine leiomyomaArch Pathol Lab Med 2014 138(8):1115-18.10.5858/arpa.2013-0315-RS25076303 [Google Scholar] [CrossRef] [PubMed]
[2]. Sikora-Szczesniak DL, Uterine angioleiomyoma- A rare variant of uterine leiomyoma: Review of literature and case reportsPrz Menopauzalny 2016 15(3):165-69.10.5114/pm.2016.6349627980528 [Google Scholar] [CrossRef] [PubMed]
[3]. Gorginzadeh M, Tahermanesh K, Hanjani S, Khorshidizadeh A, Allahqoli L, Sadeghipour A, Uterine intracavitary angioleiomyomaJournal of Obstetrics and Gynaecology 2020 40(8):1186-88.10.1080/01443615.2019.170577532068451 [Google Scholar] [CrossRef] [PubMed]
[4]. Thomas S, Radhakrishnan L, Abraham L, Matthai A, Uterine angioleiomyoma with atypia, raised CA-125 levels, and Pseudo-Meigs syndrome: An alarming presentationCase Rep Pathol 2012 2012:51947310.1155/2012/51947322953135 [Google Scholar] [CrossRef] [PubMed]
[5]. Hong JA, Heo GE, Kwak JJ, Chung SH, A case report of angioleiomyoma of uterusObstet Gynecol Sci 2017 60(5):494-97.10.5468/ogs.2017.60.5.49428989930 [Google Scholar] [CrossRef] [PubMed]
[6]. Hsieh CH, Lui CC, Huang SC, Ou YC, ChangChien CC, Lan KC, Multiple uterine angioleiomyomas in a woman presenting with severe menorrhagiaGynecol Oncol 2003 90(2):348-52.10.1016/S0090-8258(03)00263-4 [Google Scholar] [CrossRef]
[7]. Handler M, Rezai F, Fless KG, Litinski M, Yodice PC, Uterine angioleiomyoma complicated by consumptive coagulopathyGynecol Oncol Case Rep 2012 2(3):89-91.10.1016/j.gynor.2012.03.00524371629 [Google Scholar] [CrossRef] [PubMed]
[8]. Culhaci N, Ozkara E, Yüksel H, Ozsunar Y, Unal E, Spontaneously ruptured uterine angioleiomyomaPathol Oncol Res 2006 12:50-51.10.1007/BF0289343216554917 [Google Scholar] [CrossRef] [PubMed]
[9]. Pierro A, Rotondi F, Cilla S, Ninno MD, Mattoni M, Berardi S, Giant angioleiomyoma of uterus: A case report with focus on CT imagingRadiol Case Rep 2018 13(2):371-75.10.1016/j.radcr.2018.01.01529904475 [Google Scholar] [CrossRef] [PubMed]
[10]. Sánchez-Iglesias JL, Capote S, Cubo-Abert M, Carbonell-Socias M, Cabrera S, Illán-Hernández L, A giant superinfected uterine angioleiomyoma with distant septic metastases: An extremely rare presentation of a benign process and a systematic review of the literatureArch Gynaecol Obstet 2019 300(4):841-47.10.1007/s00404-019-05267-w31435775 [Google Scholar] [CrossRef] [PubMed]