Syncephalastrum racemosum as a Rare Agent of Rhino-orbital Mucormycosis: A Case Report and Review
Neelam Gulati1, Poonam Gupta2, Charu Nayyar3, BL Sherwal4, Sunil Kumar5
1 Assistant Professor, Department of Microbiology, Government Medical College Hospital, Chandigarh, India.
2 Consultant, Department of Microbiology, Reliance Hospital, Mumbai, Maharashtra, India.
3 Consultant, Department of Microbiology, Medanta Superspeciality Hospital, Sri Ganganagar, Rajasthan, India.
4 Director, Department of Microbiology, Chacha Nehru Bal Chikatsalya, New Delhi, India.
5 Director and Professor, Department of Ear, Nose and Throat, Lady Hardinge Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neelam Gulati, Room No. 246, Block E, Government Medical College Hospital, Chandigarh, India.
E-mail: drneel222@gmail.com
Fungal infection of the paranasal sinuses is an increasingly recognised entity both in immunocompetent and immunocompromised individuals. Aspergillus species are the most common aetiologic agents of this disease. Zygomycete agents are the common culprits in the immunocompromised group. The most common agent causing human disease is Rhizopus species followed by Rhizomucor spp. The important risk factors are uncontrolled diabetes mellitus and immunsupression. Here, a rare case of pansinusitis with Syncephalastrum racemosum was reported in a 13-year-old male child with aplastic anaemia. Syncephalastrum racemosum has been debated for its role in human diseases and very few reports are documented. To the best of our knowledge this was the third report of rhino-orbital infection caused by this fungus. Syncephalastrum racemosum should be considered as one of the aetiologic agents of rhino-orbital infections especially in the immunocompromised group.
Aspergillus species, Fungal infection, Mortality, Zygomycete
Case Report
A 13-year-old male child, known case of aplastic anaemia of unknown aetiology presented to the Paediatric Emergency with petechial spots all over the body since two days. Child was afebrile with no respiratory distress. On examination he had oral ulcers, gingivitis for which chlorhexidine mouth wash and candid mouth paint was prescribed. Rest of clinical examination was essentially normal. Routine haematological investigations were normal except low platelet count i.e., 5000/mm3 for which child was transfused twice with platelet concentrate in emergency. Appropriate consents were taken wherever required.
Five days post admission the child developed fever. He was investigated for fever but the blood cultures were sterile and peripheral smear and immunochromatographic tests for malaria were negative. Meanwhile treatment with Tab. augmentin 375 mg TDS (three times a day) for seven days was started but there was no response so the drug was changed to inj. ceftriaxone. In-between, child also complained of abdominal pain for which ultrasonography was done which was non-significant. After 10 days of admission, the child developed a submandibular swelling and cervical lymphadenopathy. At the same time, the child noted nasal obstruction in his right nostril, facial swelling and proptosis. Hence, subsequently child was referred to otorhinolaryngologist for opinion.
Diagnostic nasal endoscopic examination revealed ulceration of nasal mucosa with presence of slough and crusting on right side. Rest of the Ear, Nose, Throat (ENT) examination was within normal limits. Cranial nerves were also normal including visual equity. All movements of the eye were normal. A specimen of the nasal crust was sent to the microbiology laboratory for testing. A Contrast Enhanced Computed Tomographic (CECT) scan of his brain and orbit showed bilateral opacification of the maxillary, sphenoid and ethmoid sinuses together with involvement of the cavernous sinus.
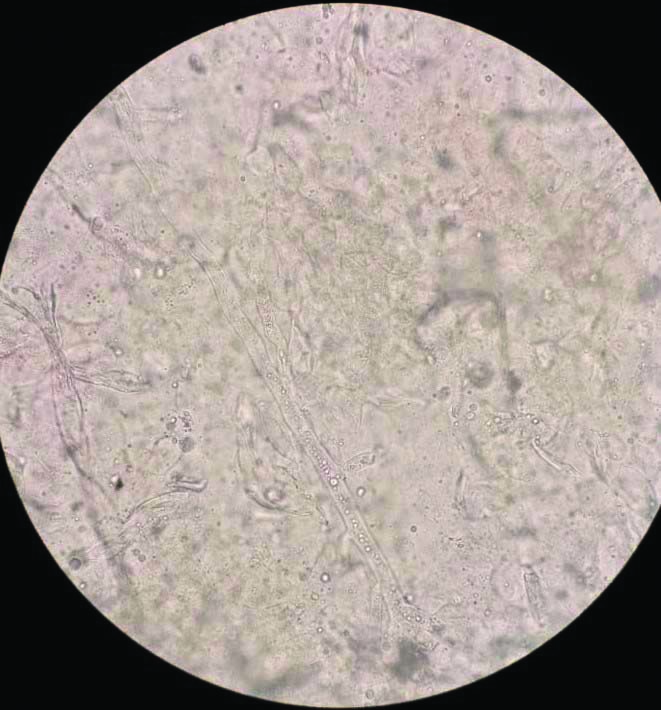
Direct examination of a portion of the nasal crust in a Potassium Hydroxide (KOH) mount using light microscopy showed hyaline, broad, coenocytic hyphae [Table/Fig-1].
KOH mount showing broad aseptate coenocytic hyphae.
A portion of the nasal crust was cultured on Sabouraud dextrose agar with and without chloramphenicol at 25°C and 37°C. After 48 hours of incubation, only white, wooly colonies producing aerial hyphae were observed on slant cultures at each temperature. Over the next 2-3 days, the colonies turned from white to gray brown and filled the culture tubes. The aetiology was also confirmed by demonstration of broad hyphae with right angled branching on histopathology.
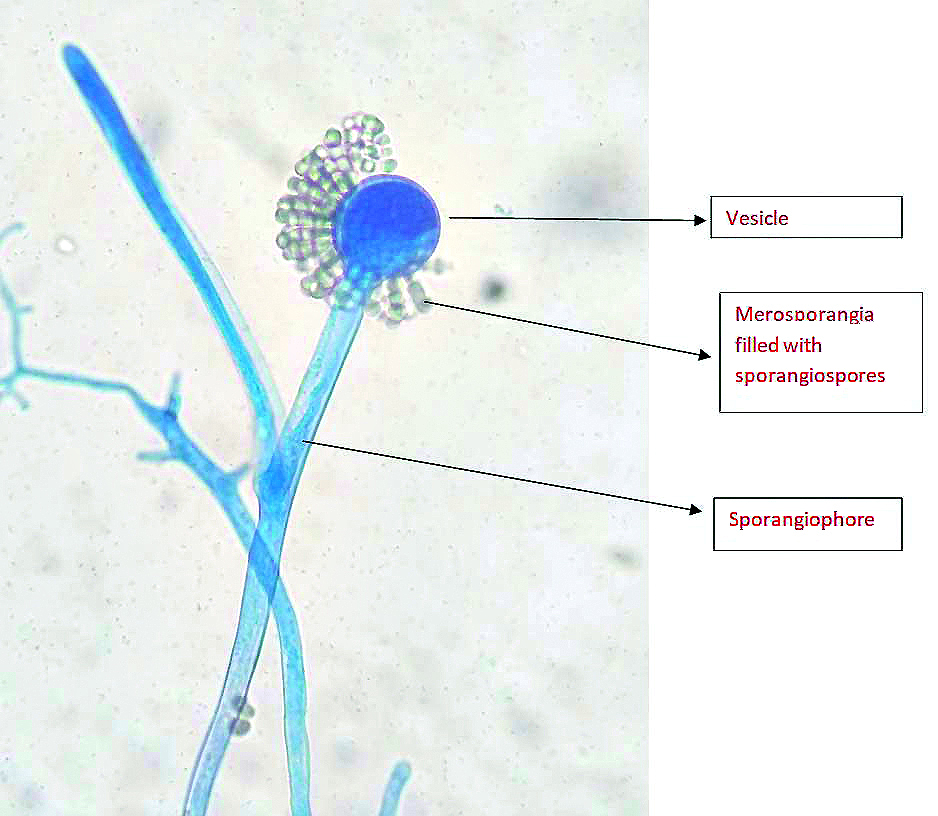
Fungal identification: Microscopic examination done with Lactophenol Cotton Blue (LPCB) revealed broad, sparsely septate hyphae branching at right angles, branched sporangiophores ending in round or oval terminal vesicles. The vesicles were surrounded by club shaped merosporangias which contained rows of round to oval sporangiospores. This arrangement gives the appearance of a daisy head. Based on the findings, the isolate was identified as Syncephalastrum racemosum [Table/Fig-2].
LPCB tease mount showing the round vesicle with tubular merosporangia filled with sporangiospores.
A clinical diagnosis of acute rhino-orbital mucormycosis was made on the basis of symptoms, signs as well as CECT pictures and normal baseline kidney functions were checked, the patient was treated with an intravenous infusion of amphotericin B deoxycholate at 50 mg/day. Meanwhile, the child had also developed difficulty in breathing and chest pain due to bilateral pleural effusion. The aetiology of this could not be ascertained by the laboratory investigation. Although, surgical debridement and biopsy for histopathological study was planned under general anaesthesia, it could not be undertaken in view of the deteriorating condition of the patient. The patient developed features of renal failure within a week, with urea and creatinine levels increasing to 28.6 mmol/L and 194.5 mmol/L, respectively. The dose of amphotericin B was reduced to 25 mg/day. On the 18th day of hospitalisation, the general condition of the patient deteriorated and he died due to multi-organ failure.
Discussion
Mucormycosis is the term used for mycological infections by the fungi of Mucorales group and rhino-orbito-cerebral mucormycosis is the most common type of mucormycosis. Factors which predispose to this type of infection are diabetes mellitus usually with ketoacidosis, leukaemia, lymphoma and other haematological disorders, corticosteroid therapy and anticancer drugs which usually lead to immunosuppression [1]. The fungi most commonly associated are Rhizopus, Rhizomucor, Absidia and Mucor. Here, authors report a case of rhino-orbital mucormycosis by a rare agent, Syncephalastrum racemosum in a child with aplastic anaemia. Unlike other agents of Zygomycetes which are known to cause mainly invasive infections, Syncephalastrum has low pathogenic potential [2].
Syncephalastrum racemosum is widely distributed in the environment especially in decaying matter, isolated from indoor and outdoor samples. Fungal air contamination may be an important risk factor in immunocompromised patients [3]. In present case, the child was suffering from aplastic anaemia which was compromising his immune status. There are 12 cases of Syncephalastrum racemosum reported in literature to the best of our knowledge. These cases have been elaborated in [Table/Fig-3] [2-12]. Five of the cases were responsible for cutaneous and subcutaneous infections, one case of fungal ball and four cases showed evidence of invasive infections. Rhino-orbital mucormycosis by Syncephalastrum racemosum has been reported previously by Mathuram AJ et al., [10] and another unpublished case has been mentioned by Gomes MZR et al., [3].
Reported cases of mycoses caused by Syncephalastrum racemosum [2-12].
| Reference | Year/Place | Age/Sex | Clinical presentation | Associated disorder | Medical management | Surgical management | Outcome |
|---|
| Kirkpatrick MB et al., [4] | 1979/USA | 61 years/M | Intracavitary fungal ball in left upper lobe | Previous history of lung abscess of bacterial origin | No specific therapy | Left upper lobectomy | Responded to treatment |
| Kamalam A and Thambiah AS, [5] | 1980/Chennai, India | 50 years/M | Cutaneous infection of the thumb with draining sinuses which progressed to arteritis and osteomyelitis | Diabetic ketosis | No specific therapy | Not performed | Died a few months later because of diabetes |
| Schlebusch S and Looke DFM [6] | 2005/Brisae, Australia | 23 years/M | Infection of the anterior abdominal wall, omentum and retroperitoneal tissues | Postoperative after splenectomy and surgical repair of lacerations following a deep trauma to the abdomen | Liposomal amphotericin B (total of 8.6g) | Surgical debridement | Wound healed, Patient survived |
| Pavlovic MD and Bulajic N, [7] | 2006/Belgrade, Serbia | 45 years/M | Right great toe nail onychomycosis | Nail injury seven months before | Nystatin ointment on nail bed postsurgery for two weeks | Extirpation of nail plate | Responded to treatment |
| Baradkar VP et al., [8] | 2008/Mumbai, India | 45 years/M | Sino-orbital infection | Chronic Hepatitis B infection and hepatic cirrhosis | Liposomal amphotericin B | Surgical debridement | Responded to treatment symptomatically |
| Amatya R et al., [2] | 2010/Nepal | 30 years/F | Multiple discharging lesions over the dorsum of left foot | Immunocompetent, following an injury to left foot with bamboo stick in fields | Could not be followed-up for treatment | Could not be followed-up for treatment | Not known |
| Ramesh V et al., [9] | 2010/Delhi, India | 4 years/M | Erythematous, raised and painless plaque encircling left thigh, extending to buttock and inguinal fold on same side | Could be following trauma while playing in garden | Potassium iodide five drops, three times daily increased to 20 drops for three months | Not performed | Complete regression of lesion |
| Ramesh V et al., [9] | 2010/Delhi, India | 8 years/M | Firm subcutaneous swelling on left buttock | Could be following trauma while playing in garden | Itraconazole 100 mg/d for two months. Slow progress so started on Potassium iodide | Not performed | Regression of lesion. Under treatment at the time of case documentation |
| Gomez MZR et al., -Unpublished case [3] | 2011/Texas, United States | 64 years/F | Rhino-orbital infection | Relapsed ALL after allogenic hematopoietic stem cell transplantation | Liposomal amphotericin B, granulocyte transfusions and G-CSF | Extensive debridement | Recovered |
| Mathuram AJ et al., [10] | 2013/Vellore, India | 63 years/M | Rhino-orbital cerebral | Diabetes Mellitus | Amphotericin B | NA | NA |
| Mangaraj S et al., [11] | 2014/Odisha, India | 45 years/M | Solitary subcutaneous swelling on anterior chest wall | Diabetes mellitus | Liposomal Amphotericin B | Surgical debridement | Recovered |
| Baby S et al., [12] | 2015/Kerala, India | 50 years/F | Injury to left great toe nail | Diabetic | Topical Nystatin | Surgical excision | Recovered |
NA: Not available; ALL: Acute lymphoblastic leukemia; G-CSF: Granulocyte colony stimulating factor
It has been a topic of debate for long that if Syncephalastrum is a true pathogen or merely a transient coloniser or contaminant [3]. Even though it was considered commonly as a contaminant earlier these reported cases are evidence of the pathogenicity of this fungus. The pathogenicity has been better established by the demonstration of the broad hypahae with right angled branching on histopathology and growth of Syncephalastrum racemosum on culture along with clinical correlation. This fungus cannot always be regarded as contaminant. Unlike other agents of Mucorales who are notorious for their fatal outcomes, Syncephalastrum racemosum is a pathogen with low virulence [13]. Treatment of zygomycete infection includes an aggressive surgical debridement, systemic antifungal therapy and correction of underlying treatment [2]. Amphotericn B and posaconazole are the most effective agents against Mucorales [14]. Syncephalastrum racemosum has been shown to be susceptible to itraconazole, terbenafine and nystatin also [13,14].
Present study stresses on the value of microbiological diagnosis in the management of a patient with zygomycete infection. Demonstration of fungal elements on histopathology as evidence of invasiveness is stressed upon to rule out colonisation. Most clinicians probably for the same reason send the samples for histopathology and miss out on microbiological investigation. A histopathology report usually takes days while a simple KOH examination can provide the report in an hour. A KOH report along with clinical correlation can help the patient in early institution of antifungal therapy. Furthermore, histopathology gives evidence of infection by a zygomycete agent with broad hyphae and right angled branching which are usually known to be resistant to azoles and are only left with the option of amphotericin B antifungal therapy and posaconazole in resistant cases [14]. Identification of the growth on culture is important more so where antifungal susceptibility facilities are not available as some agents. Syncephalastrum, Lichtheimia and Rhizomucor show susceptibility also to itraconazole and terbenafine. Mucor, Rhizopus and Cunninghamella have high Minimum Inhibitory Concentration (MIC) for posaconazole, itraconazole and amphotericin B. Terbenafine MIC values are high for Mucor and Rhizopus but low for Cunninghamella [14]. This information will help in choice of antifungal therapy after the isolate has been identified.
Conclusion(s)
Syncephalastrum racemosum, an agent with low virulence is regarded mostly as a contaminant can be an important agent of invasive mycoses. Establishing the agent in invasive infections like rhino-orbital mucormycosis is important in the timely management of the patient.
NA: Not available; ALL: Acute lymphoblastic leukemia; G-CSF: Granulocyte colony stimulating factor
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 12, 2020
Manual Googling: Feb 08, 2021
iThenticate Software: Mar 09, 2021 (16%)
[1]. Gorjón SP, Pérez BP, Caletrío BA, Munoz Herrera AMM, González FS, Cañibano RF, Rhino-orbito-cerebral mucormycosis, a retrospective study of 7 casesActa Otorrinolaringol Esp 2010 61(1):48-53.10.1016/S2173-5735(10)70008-9 [Google Scholar] [CrossRef]
[2]. Amatya R, Khanal B, Rijal A, Syncephalastrum species producing mycetoma-like lesionsIndian J Dermatol Venereol Leprol 2010 76(3):284-86.10.4103/0378-6323.6297720445304 [Google Scholar] [CrossRef] [PubMed]
[3]. Gomes MZR, Lewis RE, Kontoyiannis DP, Mucormycosis caused by unusual mucormycetes, non-rhizopus, -mucor, and -lichtheimia speciesClin Microbiol Rev 2011 24(2):411-45.10.1128/CMR.00056-1021482731 [Google Scholar] [CrossRef] [PubMed]
[4]. Kirkpatrick MB, Pollock HM, Wimberley NE, Bass JB, Davidson JR, Boyd BW, An intracavitary fungus ball composed of SyncephalastrumAm Rev Respir Dis 1979 120(4):943-47. [Google Scholar]
[5]. Kamalam A, Thambiah AS, Cutaneous infection by SyncephalastrumSabouraudia 1980 18(1):19-20.10.1080/003621780853800517368041 [Google Scholar] [CrossRef] [PubMed]
[6]. Schlebusch S, Looke DFM, Intraabdominal zygomycosis caused by Syncephalastrum racemosum infection successfully treated with partial surgical debridement and high-dose amphotericin b lipid complexJ Clin Microbiol 2005 43(11):5825-27.10.1128/JCM.43.11.5825-5827.200516272533 [Google Scholar] [CrossRef] [PubMed]
[7]. Pavlovic MD, Bulajic N, Great toenail onychomycosis caused by Syncephalastrum racemosumDermatol Online J 2006 12(1):710.5070/D3794644T616638375 [Google Scholar] [CrossRef] [PubMed]
[8]. Baradkar VP, Mathur M, Panda M, Kumar S, Sino-orbital infection by Syncephalastrum racemosum in chronic hepatorenal diseaseJ Oral Maxillofac Pathol 2008 12(1):45-47.10.4103/0973-029X.42199 [Google Scholar] [CrossRef]
[9]. Ramesh V, Ramam M, Capoor MR, Sugandhan S, Dhawan J, Khanna G, Subcutaneous zygomycosis: Report of 10 cases from two institutions in North IndiaJ Eur Acad Dermatol Venereol 2010 24(10):1220-25.10.1111/j.1468-3083.2010.03606.x20202057 [Google Scholar] [CrossRef] [PubMed]
[10]. Mathuram AJ, Mohanraj P, Mathews MS, Rhino-orbital-cerebral infection by Syncephalastrum racemosusmJ Assoc Physicians India 2013 61(5):339-40. [Google Scholar]
[11]. Mangaraj S, Sethy G, Patro MK, Padhi S, A rare case of subcutaneous mucormycosis due to Syncephalastrum racemosum: Case report and review of literatureIndian J Med Microbiol 2014 32(4):448-51.10.4103/0255-0857.14225225297037 [Google Scholar] [CrossRef] [PubMed]
[12]. Baby S, Ramya TG, Geetha RK, Onychomycosis by Syncephalastrum racemosum: case report from Kerala, IndiaDermatol Reports 2015 7(1):552710.4081/dr.2015.552725918616 [Google Scholar] [CrossRef] [PubMed]
[13]. Ribes JA, Vanover-Sams CL, Baker DJ, Zygomycetes in human diseaseClin Microbiol Rev 2000 13(2):236-301.10.1128/CMR.13.2.23610756000 [Google Scholar] [CrossRef] [PubMed]
[14]. Vitale RG, de Hoog GS, Schwarz P, Dannaoui E, Deng S, Machouart M, Antifungal susceptibility and phylogeny of opportunistic members of the order mucoralesJ Clin Microbiol 2012 50(1):66-75.10.1128/JCM.06133-1122075600 [Google Scholar] [CrossRef] [PubMed]