Ureteral stent placement is an established method for the drainage of the upper urinary tract, the DJ ureteral stent has been widely used in the endourology surgery [1,2]. Once inserted ureteral stents are rapidly colonised by infectious organisms. Several studies have demonstrated an increased risk for postoperative sepsis in patients with pre-existing stent [3,4]. Several studies have demonstrated poor correlation between urine and SC results, complicating the selection of appropriate antibiotics even when bacteria are identified in Urine Culture (UC). This discrepancy is the result of polymicrobial biofilm formation on the surface of the ureteral stents. Bacteria released from biofilms can be cultured from urine but may not accurately reflect the full bacterial population growing within the urinary tract [5].
Stent Culture (SC) may provide additional information regarding the true bacterial pathogens causing postendourological intervention Urinary Tract Infection (UTI) and dictate the proper antibiotic treatment for septic patients. Clinical implications of SC in patients undergoing endourological intervention have been studied in the past by only two groups [6,7]. Both these studies revealed results of stent colonisation contradictory to literature, showing stent colonisation predominantly by gram positive bacteria and thus challenging routine prophylaxis for gram negative bacteria during endourological procedures [8,9].
Hence, the present study was undertaken with the aim to determine the ability of UC to predict SC status and identify associated infectious pathogens with their antibiotic sensitivity patterns and to evaluate the association between SC and postendourological intervention sepsis. Identification of patterns of colonisation from cranial and caudal tip of DJ stents were also done.
Materials and Methods
This prospective single centre observational cohort study was conducted in the Department of Urology, Army Hospital Research and Referral, New Delhi, India, from August 2017 to March 2019, after approval of the Ethical and Research Committees with Institutional registration number IEC Regn No-107/2017. Informed written consent was taken from all participants before enrollment.
Sample size calculation: The sample size was calculated on the basis of parameter of interest, which was the percentage of identical bacteria identified by UC and SC. In a study by Nevo A et al., 48 patients had both positve UC and SC, but only 24/48 (50%) had identical bacteria in both cultures [6]. With the assumption of 50% and 95% confidence interval, the minimum sample size required was 100.
Inclusion criteria: Patients undergoing endourological intervention who had a ureteral stent before the operation were included in study.
Exclusion criteria: The patients who did not have a ureteral stent prior to endourological intervention or in whom the stent was placed preoperatively for infective indications were excluded from the study.
Preoperative UC was obtained from voided midstream urine from all patients. Patients with a positive UC were treated with a one-week oral or intravenous antibiotic course as per the UC results followed by a second UC to check urine sterilisation, and a single preoperative dose of 2 gram cefoperazone and sulbactam was given prior to DJ stenting. Definitive surgery was scheduled as soon as possible, and not less than two weeks after stent insertion to allow ureteral dilatation and resolution of oedema. All surgeries started with cystoscopy and DJ stent removal. During this time, intraoperative urine samples for culture were obtained by draining urine from cystoscope sheath at the beginning of procedure.
The ureteral stent was drawn through cystoscope sheath; its caudal and cranial tip were cut with scissors and were collected directly in two sterile containers separately with each containing 10 mL sterile normal saline. These containers were immediately sealed and were sent to the microbiology laboratory for culture and antibiotic sensitivity testing. The antibiotic susceptibility testing was done using BioMerieux VITEK2 method. Perioperative antibiotics were given routinely as per institutional protocol (one preoperative dose of cefoperazone and sulbactam 2 grams and 2 doses postoperatively at 8 hours interval). Serial monitoring of all patients was done and routine UC was taken only in patients developing features of urosepsis. If patients developed features of sepsis, they were started on empirical Intravenous (IV) antibiotics (cefoperazone and sulbactam 2 grams 8th hourly which were later switched to culture specific antibiotics (considering intraoperative urine and SC) and other supportive measures as required. The follow-up period for assessing postoperative sepsis was 48 hours.
Statistical Analysis
The analysis included profiling of patients on different demographic, clinical and laboratory parameters. Quantitative data were presented in terms of means and Standard Deviation (SD). Qualitative/categorical data were presented as absolute numbers and percentage. Independent Student’s t-test was used for comparison of quantitative parameters. Cross tables were generated, and Chi-square test was used for testing of associations. The sensitivity, specificity, PPV, NPV and accuracy of UC for detecting stent colonisation were calculated. The association between SC and additional preoperative characteristics were evaluated with univariate and multivariate logistic regression. The p-value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS software.
Results
A total of 100 patients who underwent endourological intervention after prior DJ stenting were recruited in the study. Amongst study participants there were 79 males and 21 females. The mean age in the study population was 41.8±15 years. A total of 19 participants were suffering from DM and two patients were immunocompromised.
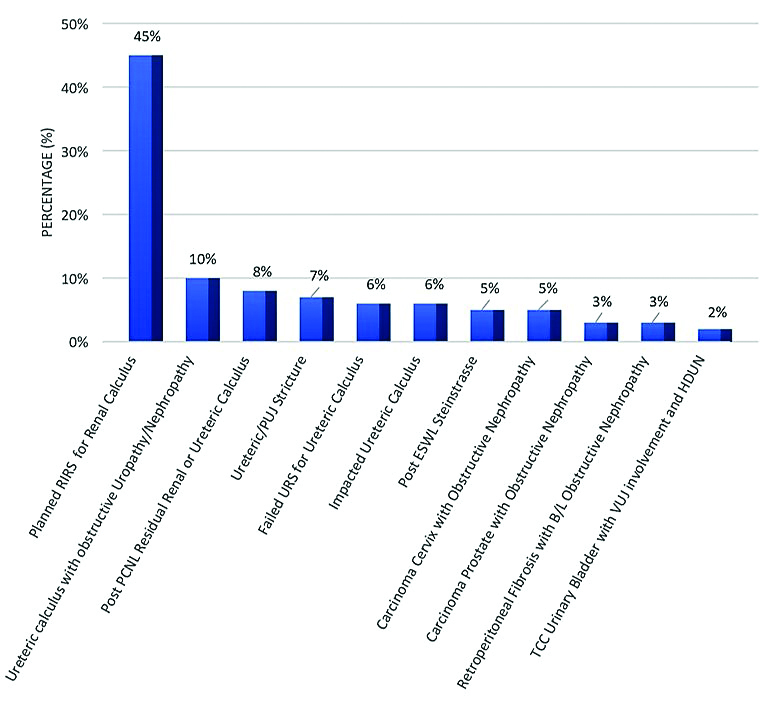
The most common indications for preoperative DJ stenting was for passive dilatation of ureter prior to Retrograde Intra Renal Surgery (RIRS) for renal calculus, Ureteric calculus causing obstructive nephropathy, ureteric stricture and post Percutaneous Nephrolithotomy (PCNL) residual calculus [Table/Fig-1].
Indication of DJ stenting preoperatively.
RIRS: Retrograde intra-renal surgery; PCNL: Percutaneous nephrolithotomy; PUJ: PelviUreteric junction; ESWL: Extracorporeal shockwave lithotripsy; TCC: Transitional cell carcinoma; VUJ: VesicoUreteric junction; HDUN: Hydroureteronephrosis
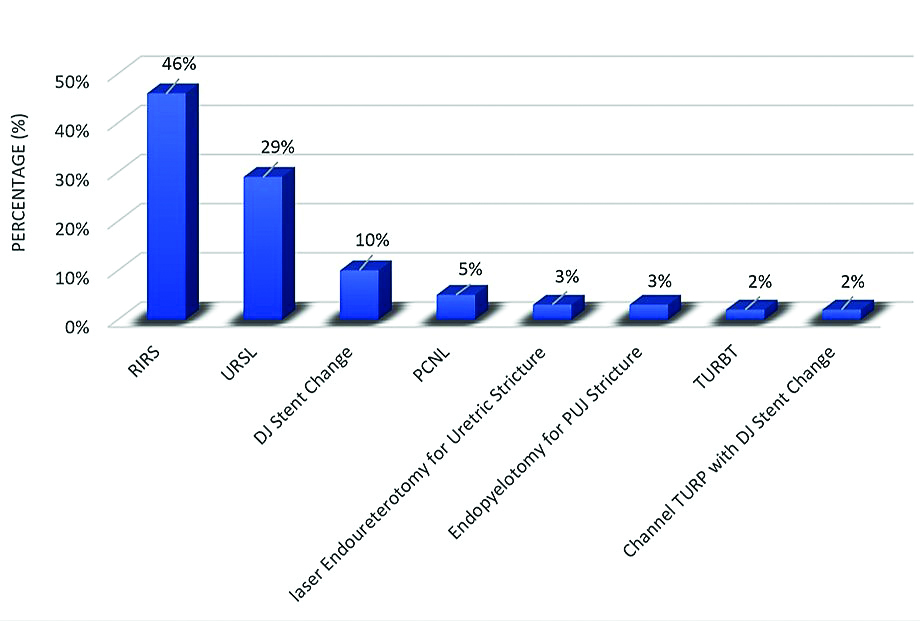
Following DJ stenting patients underwent endourological interventions after a median stented duration of 25 days. These interventions included RIRS, Ureteroscopic Lithotripsy (URSL), DJ stent change, PCNL, endopyelotomy, laser endoureterotomy, Transurethral Resection of Bladder Tumour (TURBT) and Channel Transurethral Resection of Prostate (TURP) [Table/Fig-2]. The mean operative time was 90.4±33.6 minutes.
Details of endourological interventions poststenting.
RIRS: Retrograde intra-renal surgery; URSL: Ureteroscopic lithotripsy; PCNL: Percutaneous nephrolithotomy; PUJ: PelviUreteric junction; TURBT: Transurethral resection of bladder tumour; TURP: Transurethral resection of prostate
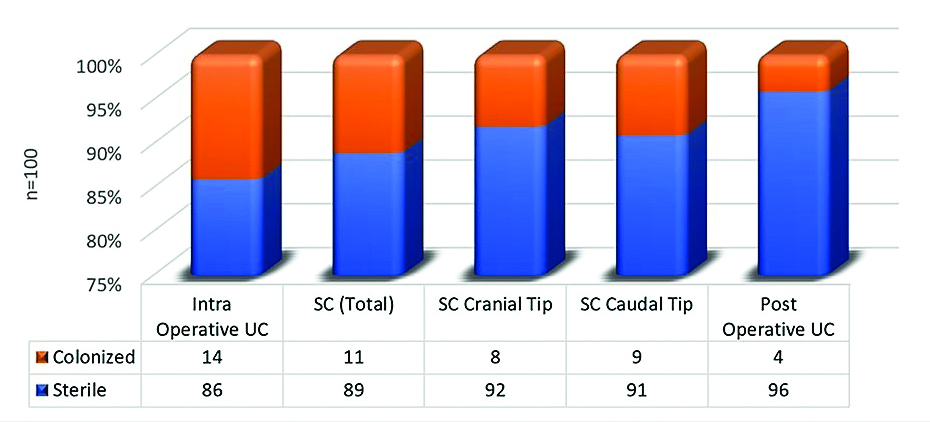
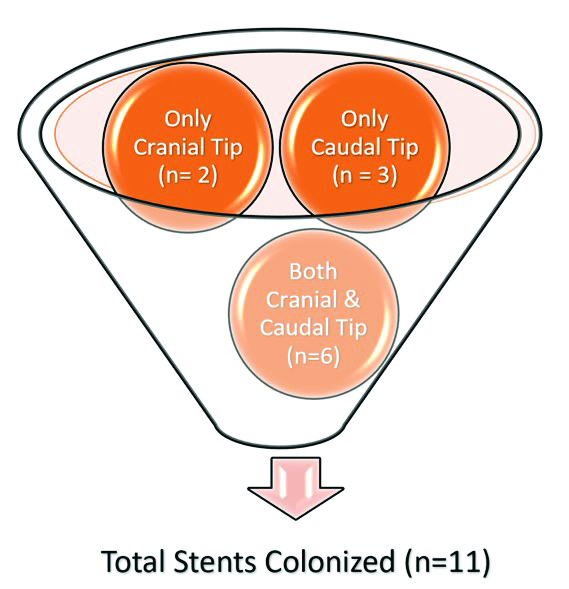
Intraoperative UC of 14 patients were colonised with pathogens while others were sterile. DJ stent Cranial tip was colonised with pathogens in eight patients. DJ stent caudal tip was colonised with pathogens in nine patients. Postoperative UC was colonised with pathogens in four patients [Table/Fig-3,4].
Urine and stent culture results.
Postoperatively Urosepsis was diagnosed clinically in six patients, these were treated with empirical antibiotics and were switched over to culture specific antibiotics. Sepsis occurred commonly in males (9.5%) as compared to females (5.1%) (p-value=0.444). A 15.8% of diabetic patients developed urosepsis, while there were two patients who were immunocompromised out of which one developed Urosepsis and both these findings were statistically significant (p-value=0.046).
Patients with sterile intraoperative UC, SC Cranial tip, SC Caudal tip and postoperative UC had very low sepsis rate 2.3%, 2.2%, 2.2% and 2.1%, respectively as compared to 28.6%, 50%, 44.4% and 100% rates of urosepsis when these cultures were positive respectively. These findings were statistically significant (p-value=0.0001).
A total of 14 patients had colonised intraoperative UC, while 11 patients had colonised DJ stent tip culture and seven patients had both their urine and DJ stent caudal tips colonisation. There was a positive correlation between these cultures statistically (p-value=0.0001).
The sensitivity, specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of intraoperative UC for detecting stent colonisation with identical pathogen were 63.64% (95% CI: 30.79% to 89.07%), 92.13 (95% CI: 84.46% to 96.78%), 50% (95% CI: 30.16% to 69.84%) and 95.35% (95% CI: 90.35% to 97.82%), respectively. On stratifying patients by their intraoperative UC and SC, seven patients had both their cultures colonised and three of these developed sepsis (42.9%). While 1 out of 7 and 2 out of 4 patients developed sepsis in whom isolated UC and isolated SC were colonised, respectively [Table/Fig-5].
Pathogens isolated from urine and DJ stent culture.
| S. No. | Intra operative UC | SC cranial tip | SC caudal tip | Post-operative UC | Same organism on UC and SC | Same organism on cranial and caudal Tip SC | Single culture positive | Post-operative Sepsis |
|---|
| 1. | Sterile | E. coli | E. coli | E. coli | | Yes | | Yes |
| 2. | E. coli | Sterile | Sterile | Sterile | | | Yes | Yes |
| 3. | Sterile | Sterile | Klebsiella pneumoniae | Klebsiella pneumoniae | Yes | | | Yes |
| 4. | E. coli | Sterile | Sterile | Sterile | | | Yes | |
| 5. | E. coli | Sterile | Sterile | Sterile | | | Yes | |
| 6. | Enterococcus faecium | Sterile | Candida albicans | Sterile | | | | |
| 7. | E. coli | Sterile | E. coli | Sterile | Yes | | | |
| 8. | E. coli | Staphylococcus aureus | Sterile | Sterile | | | | Yes |
| 9. | Staphylococcus epidermidis | Sterile | Sterile | Sterile | | | Yes | |
| 10. | Sterile | Pseudomonas aeruginosa | Pseudomonas aeruginosa | Sterile | | Yes | | |
| 11. | Klebsiella pneumoniae | Klebsiella pneumoniae | Klebsiella pneumoniae | Klebsiella pneumoniae | Yes | Yes | | Yes |
| 12. | E. coli | E. coli | E. coli | Sterile | Yes | Yes | | |
| 13. | Pseudomonas aeruginosa | Pseudomonas aeruginosa | Pseudomonas aeruginosa | Pseudomonas aeruginosa | Yes | Yes | | Yes |
| 14. | Klebsiella pneumoniae | Sterile | Sterile | Sterile | | | Yes | |
| 15. | E. coli | Sterile | Sterile | Sterile | | | Yes | |
| 16. | Sterile | Klebsiella pneumoniae | Klebsiella pneumoniae | Sterile | | Yes | | |
| 17. | E. coli | Sterile | Sterile | Sterile | | | Yes | |
| 18. | Enterococcus faecalis | E. coli | Sterile | Sterile | | | | |
| Total | 14 | 8 | 9 | 4 | 5 | 6 | 7 | 6 |
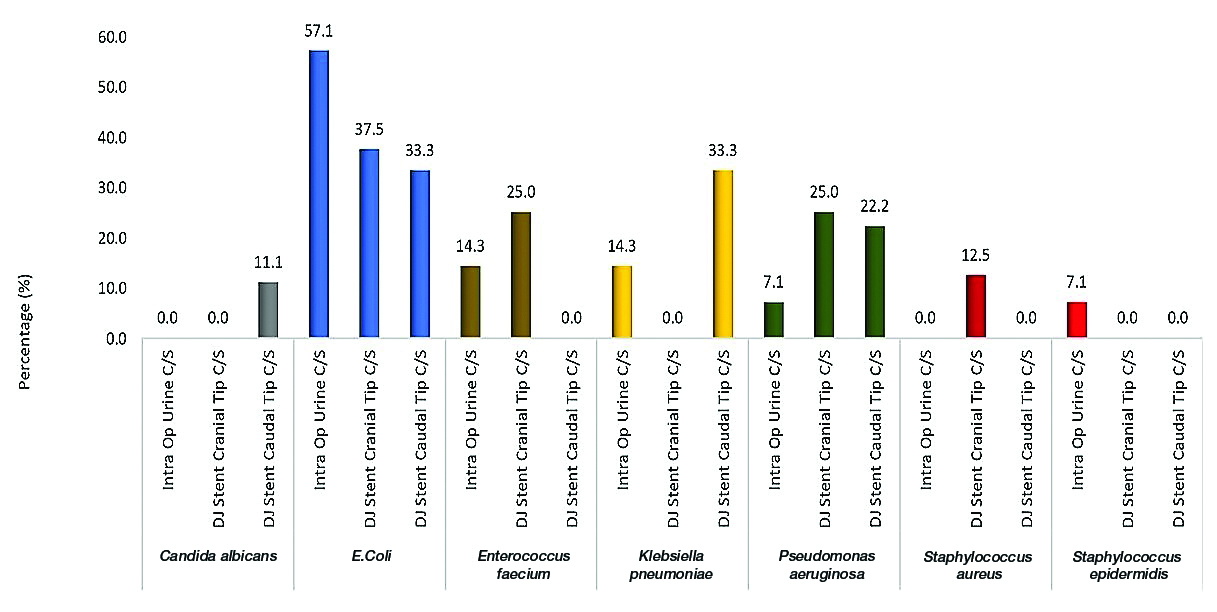
E.coli was the most commonly isolated pathogen from UC (57.1%), DJ stent cranial tip culture (37.5%) and DJ stent caudal tip culture (33.3%). Five patients had positive UC as well as DJ Stent cranial and caudal tip culture findings, 3/5 (60.0%) patients had identical bacteria in both UC and DJ stent cranial tip cultures whereas 4/5 (80.0%) patients had identical bacteria in both UC and DJ stent caudal tip culture findings. Six patients had both DJ stent cranial and caudal tips colonised, and all had the same pathogens isolated on their respective cultures. Only one patient had DJ stent cranial tip colonised by Gram positive bacteria, one had Candida albicans isolated from DJ stent caudal tip culture, while all other DJ stent pathogens were Gram negative [Table/Fig-6]. There was no difference in antibiotic sensitivity pattern for pathogens isolated from intraoperative UC of DJ SC where both these cultures were colonised by similar pathogens.
Pathogens isolated from intraoperative urine culture and stent culture.
The sensitivity and positive predictive value of SC in predicting postoperative sepsis were low at 83.33% and 45.45%, respectively, whereas the specificity and negative predictive value were high at 93.6% and 98.8%. On univariate logistic regression analysis, Operative Time (OR=1.04, 95% CI: 1.01-1.07), positive Intraoperative UC (OR=16.8, 95% CI: 2.7-103.6), positive DJ stent cranial tip culture (OR=45.0, 95% CI: 6.3-322.9) and positive DJ stent caudal tip culture (OR=35.6, 95% CI: 5.2-243.2) were associated with postendourological intervention sepsis. While on multivariate analysis none of these factors were associated with postendourological intervention sepsis [Table/Fig-7].
Univariate and multivariate analysis of factors predisposing to postendourological intervention sepsis.
| Univariate analysis | Multivariate analysis |
|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value |
|---|
| Age | 1.0 (0.95-1.06) | 0.865 | 1.0 | 0.815 |
| Gender |
| Male | 1 | | 1 | |
| Female | 1.97 (0.34-11.59) | 0.452 | 3.7 | 0.534 |
| Diabetes Mellitus (DM) |
| No | 1 | | 1 | |
| Yes | 4.87 (0.90-26.37) | 0.066 | 8.4 | 0.339 |
| Operative time | 1.04 (1.01-1.07) | 0.012* | 0.96 | 0.153 |
| Intraoperative UC |
| Negative | 1 | | 1 | |
| Positive | 16.8 (2.7-103.6) | 0.002* | 4.5 | 0.328 |
| SC (Cranial) |
| Negative | 1 | | 1 | |
| Positive | 45.0 (6.3-322.9) | 0.0001* | 19.4 | 0.090 |
| SC (Caudal) |
| Negative | 1 | | 1 | |
| Positive | 35.6 (5.2-243.2) | 0.0001* | 7.7 | 0.257 |
*significant
Discussion
The main purpose of ureter stents is to maintain patency of ureter and to ensure adequate urine drainage, however the colonisation of stent and biofilm formation by various microorganisms adds to the stent related morbidity. The process of stent colonisation and its relation to the development of Urinary Tract Infection (UTI) is a poorly understood phenomenon. This study sought to determine the clinical role that the SC might play in clinical practice. Nevo A et al., and Kozyrakis D et al., have conducted similar studies in the past [6,7]. Demographics of present study patient cohort were comparable to both these study groups.
A 26.6% of patients included in the Kozyrakis D et al., group were stented for obstructive pyelonephritis [7]. Present study participants included only those stented preoperatively for non-infectious indications. The mean duration for preoperative stenting was 40.8±38.3 days and included patients with both upper and lower tracts endourological interventions [Table/Fig-2]. All patients in the study group of Kozyrakis D et al., and Nevo A et al., underwent upper urinary tract interventions [6,7].
In literature, most of the authors have commented upon only on either cranial or caudal tips of DJ SC and stent colonisation rates have varied considerably amongst various study populations. There are only few studies mentioning the role of both the tips and see the difference in colonisation rates [10]; thus present study cohort wanted to highlight the importance of different tips culture and their relation to urosepsis.
Nevo A et al., and Kozyrakis D et al., have reported stent colonisation rate of 24.4% and 78%, respectively with predominantly gram positive bacteria being isolated from up to 50% of SC as compared to 24.2% of UC [6,7]. Both these studies reported SC results contradictory to literature [8,9]. In present study group, intraoperative UC of 14 patients were colonised with pathogens, SC cranial tip was colonised in eight patients and SC Caudal tip was colonised in nine patients. Lower rate of stent colonisation in present study population was likely due to shorter time for which stent was retained preoperatively and only non-infectious indications of preoperative stenting cases included in present study.
In present study cohort, both urine and stents were predominantly colonised by gram negative pathogens. E.coli was isolated from UC 57.1% of UC, 37.5% of SC cranial tip and 33.3% SC caudal tip. Only one patient had SC cranial tip colonised by gram positive bacteria and one had Candida albicans isolated from SC caudal tip. Colonised UC was found in 14.0% patients, SC cranial tip and caudal tip culture were colonised in 8.0% and 9.0% patients, respectively. A 5% patients had both positive UC and SC (including cranial or caudal tip cultures). In all these patients, positive UC predicted positive stent cranial and caudal tip culture in 60.0% and 80.0%, respectively. Six patients had both DJ stent cranial and caudal tips colonised, and all had similar pathogens isolated on their respective cultures. In present study, the specificity and negative predictive value of intraoperative UC for detecting stent colonisation with identical pathogens was found to be relatively higher than those reported by Nevo A et al., [6].
In the present study, postoperative urosepsis was diagnosed clinically in 6% of cases which is comparable to literature. Postoperative UC was colonised with pathogens in four patients. Patients with sterile intraoperative UC had very low sepsis rate (2.3%) as compared to patients who had colonisation of their UC (28.6%). Nevo A et al., reported postoperative sepsis in 4.9% patients, patients with negative SC having very low sepsis rates (0% and 1.1%) regardless of UC results, while patients with positive SC had a sepsis rate of 12.5% which was doubled if UC was also positive [6].
Seven patients had both their intraoperative UC and SC colonised and three of these developed sepsis (42.9%). While one out of seven (14%) and two out of four (50%) patients developed sepsis in whom isolated UC and isolated DJ stent caudal tip cultures were colonised respectively. In Kozyrakis D et al., study group 18% experienced a febrile UTI and in 63.6% of these cases stents were colonised, only one patient with colonised stent did not develop fever after surgery. Authors reported that SC and the susceptibility tests were able to shift the treatment from an empirical to an evidenced based one with a favourable outcome [7].
Routine postoperative antibiotics were given as per institutional protocol while those who developed sepsis were given empirical antibiotics and were switched over to culture specific antibiotics. The organisms grown on SC in patients with sepsis, were usually found to be resistant to commonly used uroselective antibiotics such as fluoroquinolones and aminoglycosides. These organisms showed sensitivity to piperacillin with tazobactum, tigecycline, teicoplanin and colistin. A similar finding was noted in a study cohort by Pal DK et al., which found sensitivity to newer generation antibiotics [11].
In present cohort, sepsis occurred postoperatively in 15.8% of diabetic patients and out of the 2 patients which were immunocompromised (HIV, steroid therapy), one patient developed urosepsis. Both these co-morbid conditions were significantly associated with postendourological intervention sepsis (p-value=0.046). On univariate logistic regression analysis of present study group, positive intraoperative UC, positive SC cranial tip and positive SC caudal tip were significantly associated with postendourological intervention sepsis (p<0.05). Authors additionally found operative time was also significantly associated with postoperative sepsis on univariate logistic regression analysis, while on multivariate analysis none of these factors were associated with postendourological intervention sepsis.
The strength of present study was SC in various endourological procedures, performing SC in both cranial and caudal tip of DJ stent. The knowledge of the bacteriologic flora encountered in the stents of an institution could be helpful for an evidence based prophylactic and therapeutic practice. Stent examination could be recommended in cases at higher risk of developing UTI after a urologic intervention such as those with DM or other immune compromised patients and those suspected to take long operative time.
Limitation(s)
Firstly, the practice to perform a routine culture on all the stents may not be clearly recommended as it is not considered cost-effective and increases the workload to the microbiology laboratory. Secondly, the sample size was not too large to draw any definitive statistical conclusion. Thirdly, no correlation with sepsis rate were made with various stone parameters such as size or site and those who had positive preoperative culture. Thus, larger studies involving various subgroups are needed to address these limitations.
Conclusion(s)
The colonisation of UC can predict colonisation of DJ SC and identify associated infectious pathogens. Colonisation of DJ SC is significantly associated with postendourological intervention sepsis. There can be a slight difference in pattern of colonisation from intraoperative urine, cranial and caudal tip of DJ stents but mostly these are colonised by gram negative bacteria. However, periodically performed SC might be useful in detecting the prevailing bacterial species and determining their antibiotic sensitivity.
*significant