Cutaneous Diphtheria by Nontoxigenic Corynebacterium Diphtheriae in Diabetic Patient: A Case Report
Pooja Singla1, Pratibha Mane2, Prashant Singh3
1 Assistant Professor, Department of Microbiology, SHKM GMC, Nalhar, Nuh, Haryana, India.
2 Professor and Head, Department of Microbiology, SHKM GMC, Nalhar, Nuh, Haryana, India.
3 Postgraduate (IIIrd Year), Department of Microbiology, SHKM GMC, Nalhar, Nuh, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Pooja Singla, Assistant Professor, Department of Microbiology, SHKM GMC, Nalhar, Nuh-122107, Haryana, India.
E-mail: pjsingla3@gmail.com
Chronic diabetes mellitus is a significant risk factor for skin and soft tissue infections. Corynebacterium diphtheriae is a rare cause of wound infection in chronic diabetic patients. Here, a rare case of wound infection by non-toxigenic Corynebacterium diphtheriae in a chronic diabetic 45-year-old female patient has been reported. She presented with multiple discharging punched out ulcers on lower back. Diagnosis was confirmed by conventional PCR detecting rpoB gene and toxigenicity testing by Elek’s gel precipitation test. Patient was treated with IV benzylpenicillin and regular dressing. Isolation of single opportunistic microorganism creates a characteristic feature in the present case.
Chronic diabetes mellitus, Polymerase chain reaction, Skin ulcers
Case Report
A 45-year-old female presented to the Dermatology Outpatient Department with complaints of multiple discharging painful ulcers on left side of lower back for last one month. As per history of the patient, the lesions started with multiple vesicles and ruptured to form ulcers, which increased gradually. She applied some home made remedies but no improvement was seen. Patient was a known case of diabetes from last seven years and was taking hypoglycaemics irregularly. No travel history was revealed by patient in last six months.
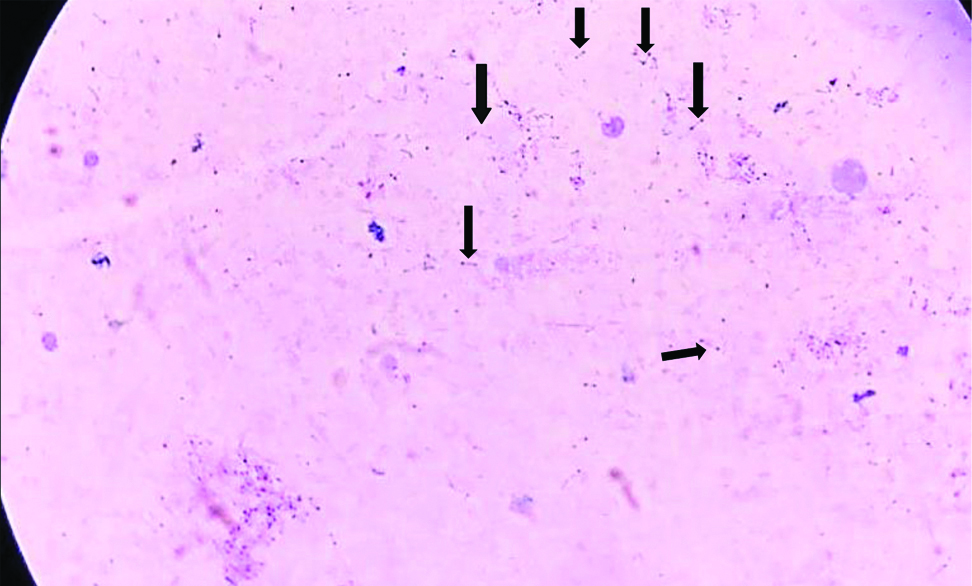
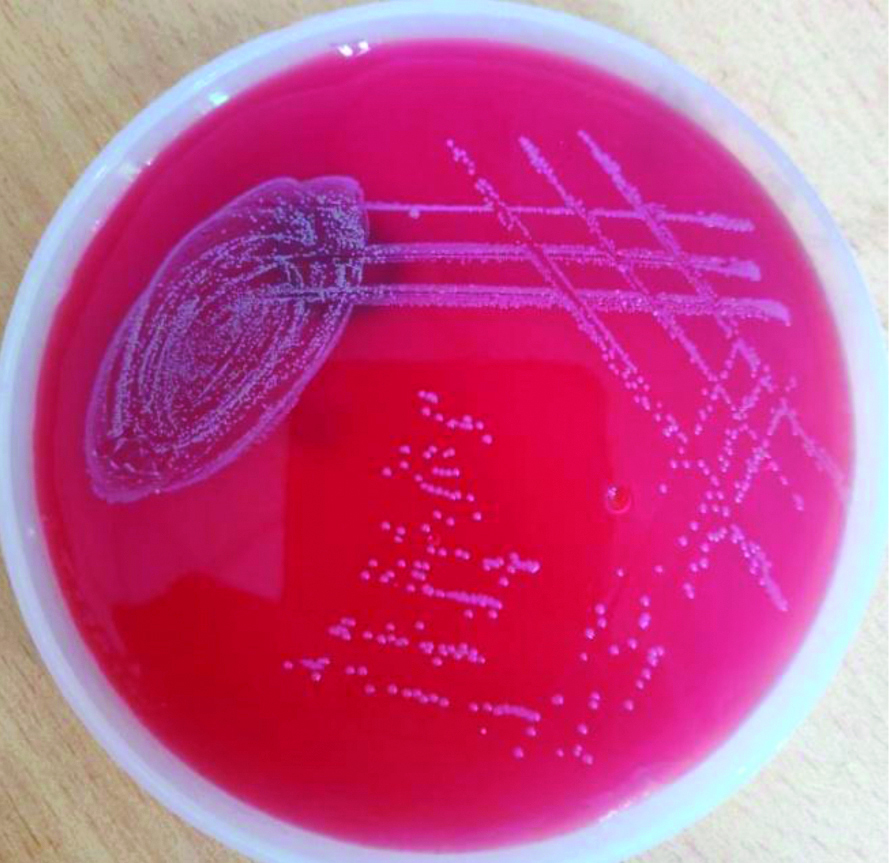
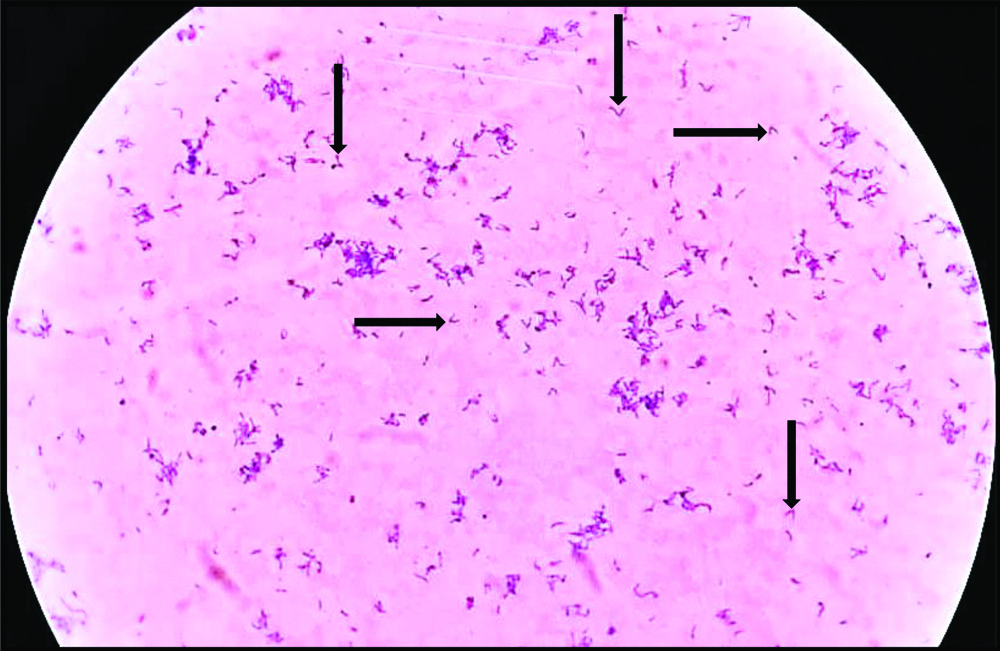
On examination, the patient was conscious, well-oriented to time, place and person, her vitals were stable and body temperature was normal. There were two well-defined punched out ulcers of size approximately 10×10 cm on left side of lower back, covered by brownish crust and surrounded by small satellite ulcers [Table/Fig-1]. Patient’s consent was taken prior to treatment. Purulent and blood stained discharge was oozing out from ulcers. No lymphadenopathy was present. No history of trauma was present. There was no history of contact with any suspected diphtheria case. Her immunisation status was unknown. All routine investigations were normal except fasting blood sugar levels which were raised to 300 mg/dL. Two pus swabs were collected from the lesions and sent to Microbiology Department. Gram staining and Albert’s staining was performed. Gram staining showed many club shaped gram positive bacilli arranged in Chinese letter pattern. Albert staining showed many green colour bacilli with bluish black metachromatic granules arranged in V or L form [Table/Fig-2]. Culture was put on Loeffler’s Serum Slope (LSS), blood agar, blood tellurite agar and MacConkey agar from another swab. Small, glistening, creamy white colonies were present on Loffler’s serum slope after six hours of incubation at 35°C. Blood agar showed small, circular, greyish white, non-haemolytic colonies [Table/Fig-3]. Black colonies were present on blood tellurite agar [Table/Fig-4]. No growth was obtained on MacConkey agar. Preliminary identification was done by making secondary smears for Gram staining and Albert staining from culture growths on LSS and blood agar [Table/Fig-5].
Punched out cutaneous ulcers.

Albert staining direct smear seen under 100X objective (Arrows showing bacilli with metachromatic granules in V and L forms).
Colonies on 5% sheep blood agar.
Black coloured colonies on potassium tellurite agar.

Gram staining secondary smear seen under 100X objective (gram positive bacilli with granules seen).
For confirmation and for toxigenicity testing, isolate was sent to National Centre for Disease Control (NCDC) Delhi, where it was confirmed as C.diphtheriae by detection of rpoB gene by conventional Polymerase Chain Reaction (PCR). Molecular identification of C.diphtheria is recommended in clinical settings by using rpoB gene sequences as these are more specific and have high ability to distinguish between genetically closely related species of Corynebacterium [1]. The strain was non-toxigenic by Elek’s gel precipitation test. Patient was admitted in isolation ward. On the basis of clinical suspicion and preliminary findings of staining and culture, empirical treatment was started with benzylpenicillin 150000 U/Kg per day in four divided doses intravenously. Daily dressing was done with soframycin and patient was counselled to take hypogycaemics regularly. Signs of improvement in the form of reduced discharge and redness were noticed after four days of therapy. After 10 days of therapy, culture from wound swab was negative. Patient was discharged after 14 days when two consecutive cultures were negative.
Discussion
Diphtheria is a re-emerging disease in certain parts of the world including India either due to low immunisation coverage or incomplete immunisation [2]. Cutaneous diphtheria is a skin manifestation of diphtheria caused by both toxigenic and non-toxigenic strains of Corynebacterium diphtheria [3]. Clinically, it is characterised by formation of chronic, non-healing, necrotic ulcers occurring mainly on the extremities. Many risk factors are associated with the disease such as travel to endemic areas, poor socio-economic condition, overcrowding, skin trauma, pre-existing skin lesions, imunocompromised state and contact with cattles etc., [2,3]. Immunocompromised state due to chronic diabetes mellitus was a significant risk factor in this case which leads to infection by opportunistic pathogen like C.diphtheriae.
Cutaneous diphtheria is a highly contagious infection and rarely develops into an invasive disease. The ulcers are slowly progressive thus, prolonged shedding of the organism from the skin lesions can contaminate the environment leading to respiratory and cutaneous infections in susceptible individuals. Clinical suspicion and microbiological confirmation of the organism is needed to start appropriate antibiotic therapy and to prevent further spread of the organism to susceptible contacts [2-4].
Cutaneous diphtheria is endemic in tropical countries. Sporadic cases have been reported from all over the world particularly in travellers who had returned from endemic countries. In the present case, there was no history of travel given by the patient. Imported cases of cutaneous diphtheria have been reported from France, Australia, USA, UK, and from many other European countries [5-8]. Few case reports are also available from India depicting both toxigenic and non-toxigenic strains of C.diphtheriae as aetiological agent of cutaneous diphtheria [9-11].
One unique finding observed in the present case was isolation of only diphtheria bacilli from the ulcers without co-isolation of any other microorganism. Some have reported polymicrobial aetiology of cutaneous diphtheria. Co-isolation of Staphylococcus aureus, Streptococcus pyogenes, Arcanobacterium has been reported showing that diphtheria bacilli can be secondary invaders or primary infection by Corynebacterium can be superseded by other pathogenic bacteria [1,11]. Cutaneous diphtheria caused by non-toxigenic strains is on rise and have been reported from many countries [5-7]. Authors from UK in 2015 reported a case of cutaneous diphtheria caused by penicillin resistant non-toxigenic C.diphtheriae [5]. From India Shah SR et al., also reported non-toxigenic diphtheria bacilli causing wound infection [12]. Also, the causative agent in this case was non-toxigenic strain of C.diphtheriae.
Conclusion(s)
This case report emphasises the importance of early diagnosis and treatment of cutaneous diphtheria to prevent systemic complications and further spread of infectious agent.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 28, 2020
Manual Googling: Feb 04, 2021
iThenticate Software: Mar 09, 2021 (5%)
[1]. Khamis A, Raoult D, Scola BL, rpoB gene sequencing for identification of Corynebacterium speciesJ Clin Microbiol 2004 42(9):3925-31.10.1128/JCM.42.9.3925-3931.200415364970 [Google Scholar] [CrossRef] [PubMed]
[2]. Clarke KEN, MacNeil A, Hadler S, Scott C, Tiwari TSP, Cherian T, Global epidemiology of diphtheria, 2000-2017Emerg Infect Dis 2019 25(10):1834-42.10.3201/eid2510.19027131538559 [Google Scholar] [CrossRef] [PubMed]
[3]. Surveillance Manual|Diphtheria|Vaccine Preventable Diseases|CDC [Internet]. 2019. https://www.cdc.gov/vaccines/pubs/surv-manual/chpt01-dip.html. Accessed 11 Sep. 2019 [Google Scholar]
[4]. Murhekar MV, Resurgence of diphtheria in IndiaJ Infect 2020 80(2):232-54.10.1016/j.jinf.2019.10.01031629864 [Google Scholar] [CrossRef] [PubMed]
[5]. FitzGerald RP, Rosser AJ, Perera DN, Non toxigenic penicillin resistant cutaneous C. diphtheriae infection: A case report and review of the literatureJ Infect Public Health 2015 8(1):98-100.10.1016/j.jiph.2014.05.00625027172 [Google Scholar] [CrossRef] [PubMed]
[6]. Alberto C, Osdoit S, Villani AP, Bellec L, Belmonte O, Badell E, Cutaneous ulcers revealing diphtheria: A re-emerging disease imported from Indian Ocean countries?Ann Dermatol Venereol 2020 S0151-9638(20):30251-59. [Google Scholar]
[7]. Lim KHL, Boon M, Cutaneous diphtheria in a returned travellerJ Paediat Child Health 2019 55(3):358-61.10.1111/jpc.1424530288824 [Google Scholar] [CrossRef] [PubMed]
[8]. Berg L, Mechlin A, Schultz ES, Cutaneous diphtheria after a minor injury in SriLankaHautarzt 2016 67(2):169-72.10.1007/s00105-015-3718-626525966 [Google Scholar] [CrossRef] [PubMed]
[9]. Pandit N, Yeshwanth M, Cutaneous diphtheria in a childInt J Dermatol 1999 38(4):298-99.10.1046/j.1365-4362.1999.00658.x10321948 [Google Scholar] [CrossRef] [PubMed]
[10]. Vetrichevvel TP, Pise GA, Agrawal KK, Thappa DM, Cutaneous diphtheria masquerading as a sexually transmitted diseaseIndian J Dermatol Venereol Leprol 2008 74(2):18710.4103/0378-6323.3972818404803 [Google Scholar] [CrossRef] [PubMed]
[11]. Govindaswamy A, Trikha V, Gupta A, Mathur P, Mittal S, An unusual case of post trauma polymicrobial cutaneous diphtheriaInfection 2019 47(6):1055-57.10.1007/s15010-019-01300-x30953325 [Google Scholar] [CrossRef] [PubMed]
[12]. Shah SR, Das R, Lahiri KK, Cutaneous (wound) diphtheria by nontoxigenic Corynebacterium diphtheria var mitis- A case reportInt J Virol Infect Dis 2017 2(1):25-29. [Google Scholar]