The Chronic Subdural Haemorrhage (CSDH) is a common neurosurgical condition that very often affects elderly. Often trivial trauma and sometimes blunt trauma to the head predisposes its development. Brain atrophy in elderly leads to stretching of bridging veins that traverses the potential subdural space to drain the venous sinuses. These fragile veins are more susceptible to tear after trivial trauma and there after slow oozing into the space and subsequent osmotic expansion leads to increase volume of the subdural collection causing mass effect and clinical deterioration [1]. Most commonly the patient presents like CVA, but of subacute onset, for which they get admitted to general medicine ward. Majority of patients have recent cognitive impairment and some patients present with focal neurological deficit. Rarely, some patients present with temporal or tonsillar coning. Overall, the prognosis is good if managed promptly. Delaying the diagnosis and treatment may lead to irreversible damage and incomplete recovery or death.
Apart from old age certain other conditions predispose to the development of chronic subdural haematoma like chronic alcoholism, oral anticoagulant therapy, following shunt surgery and following head injury [Table/Fig-1,2 and 3]. Whatever may be the aetiology, so far the treatment is concerned, it is mostly surgical. Some patients do improve with conservative treatment. So, the aim of the present study is to evaluate the incidence of various mode of clinical presentation and to throw some light on different modes of managing this clinical entity in different situations and analysing the overall outcome.
Materials and Methods
This was a retrospective observational study conducted at Veer Surendra Sai Institute of Medical Science and Research (VIMSAR), Burla, Sambalpur, Odisha between September 2018 to September 2020. Total 100 patients who were admitted to Department of Neurosurgery with the diagnosis of subacute or chronic subdural haematoma were included in the study.
Inclusion criteria: Irrespective of GCS, all patients with radiological subacute and chronic subdural collection with midline shift more than 5 mm and effacement of ventricles were included in the study.
Exclusion criteria: Patients having minimal subdural collection without causing mass effect and patients who presented with bilateral puppilary failure at admission were excluded from the study.
Data were retrieved from the medical record section and critically analysed regarding patient profile, symptomatology, diagnostic method used and procedure performed along with treatment outcome. Since it is a retrospective study, the treatment end point was time of discharge but at places few long term follow-up data were collected through telephonic conversation and utilising electronic media.
Statistical Analysis
The results of the study were analysed by Statistical Package for the Social Science (SPSS) version 12.0 software. Analysis included measure of central location (mean), measure of dispersion-standard deviation. The quantitative variables were expressed as mean±SD. Qualitative variables were expressed as percentages.
Results
In the present study, left to right ratio was 1.5:1 (where left side included 50 patients and right side 34 patients). Bilateral involvement was found in 16 patients. Males were affected more commonly than females (64% versus 36%). History of acute trauma was found in 35%, trivial trauma in 57% [Table/Fig-4].
| Variables | Total number of patients, n=100 |
|---|
| Mean age in years | 57.39 (SD±16.276) |
| Male to female ratio | 1.7:1 |
| Mean GCS | 11.31 (SD±2.571) |
| Left to right ratio | 1.5:1 |
| Bilateral | 16 |
| Aetiology |
| Trauma | 35 |
| Trivial trauma | 57 |
| Idiopathic | Nil |
| After CSF diversion | 2 |
| Following coagulopathy | 6 |
| Co-morbidity |
| Chronic alcoholism | 31% |
| Hypertension | 37% |
| CKD | 10% |
| Diabetes mellitus | 6% |
| No co-morbidity | 16% |
GCS: Glasgow coma scale; CSF: Cerebrospinal fluid; CKD: Chronic kidney disease
Age range was 18 to 85 years. Highest incidence was seen in 5th to 6th decade [Table/Fig-5].
| Age group (in years) | Number of patients |
|---|
| 0 to 10 | 0 |
| 11 to 20 | 3 |
| 21 to 30 | 7 |
| 31 to 40 | 4 |
| 41 to 50 | 16 |
| 51 to 60 | 33 |
| 61 to 70 | 18 |
| 71 to 80 | 12 |
| 81 to 90 | 7 |
Headache was the most common presentation (86%). A 74% presented with subacute CVA with hemiparesis and altered sensorium. Aphasia was the only presentation in 5% patients and overall association in 15% of patients. Memory impairment and incontinence was found to be associated with 67% and 65% patients respectively. Severe dementia was present in two patients who were incontinent and totally bed ridden. About 11% of patients presented in low condition with features of either temporal or tonsillar coning with overall bad outcome [Table/Fig-6].
Spectrum of clinical presentation with incidences.
| Clinical presentation | No. of patients | Clinical presentation | No. of patients |
|---|
| Headache | 62 | Mild headache | 24 |
| Hemiparesis | 74 | Reeling/hiccough | 14 |
| Disorientation | 67 | Psychosis | 10 |
| Low condition | 11 | Severe dementia | 2 |
| Aphasia only | 5 | Aphasia | 15 |
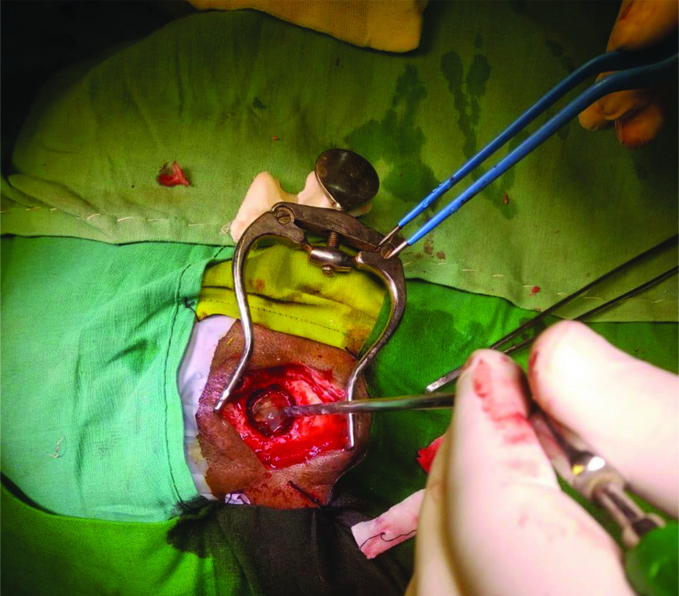
Patients were categorised into three main groups for treatment purpose. Computed Tomography (CT) scan was the main diagnostic tool (95%) and was supplemented with Magnetic Resonance Imaging (MRI) (15%) when required. The most common category of patients fall into BHD [Table/Fig-7]. Most of the subacute and chronic haematoma was drained by this method adopting the standard technique of burr hole and drainage. Absence of septation and membrane formation as evident by radiological investigation precludes any more aggressive procedure. The standard burr hole size was 1.5-2 cm [Table/Fig-8]. Majority of time single parietal burr hole was sufficient. Rarely, did it required additional frontal/occipital burr hole to facilitate drainage of the distant clots located more anteriorly or posteriorly. Routinely, closed minivac drainage was given in all elderly subjects where the brain atrophy was found substantial but in post-traumatic subacute subdural collection was done in relatively younger subject, the drain was deferred because of immediate surfacing of brain parenchyma after drainage. It was found that membrane formation was unusual in patients with subacute subdural haematoma in this series. The headache was the predominant symptoms in this subgroup of patients which subsided immediately after prompt drainage saving the patient timely from impending herniation. In BHD group residual collection was a common finding associated with pneumocephalus as seen in postoperative scan. About five patients required re-exploration for persistence of mass effect and symptoms. It was found that the focal neurological deficit took atleast 4 to 5 days to improve but aphasia took little more time i.e., more than a week for recovery.
Surgical procedure, indication and outcome.
| Treatment procedure | 100 | Indication | Outcome |
|---|
| Burr hole drainage | 94 | Usual | 5 deaths |
| Primary craniotomy | 5 | Preop Subdural membrane-4 | Good |
| Periop conversion-1 | Good |
| Secondary craniotomy | 01 | Recurrence | Good |
| Total | 100 |
Burr hole drainage, a standard technique in the management of Chronic Subdural Haemorrhage (CSDH).
It was observed that irritability remained a very significant problem in elderly individuals particularly in those who were habituated to Bhang (20%), or alcohol (31%) which took little more time to settle whereas mild irritability in postoperative period subsided within short time. One more important complication frequently encountered in immediate postoperative period particularly in chronic alcoholics was uncontrolled seizure (9%) in form of status epilepticus and infact, 3 patients out of 9 were lost due to these complications. The possible aetiology of deterioration was thought to be due to aspiration, hypoxia and arrhythmia. About six patients were revived to complete control with administration of combination of drugs like Fosphenytoin, Leviteracetam, Lacosamide, Lorazepam, Chlrodiazepoxide, Inj. Magnesium Sulfate (MgSO4) and Inj.Thiamine. Focal status (9) was more common than Generalised Tonic Clonic Seizure (2) in this series.
No disease is free from its inherent complication. Time always matters. A 11% of patients in this series presented/turned sick during their hospital stay. Glasgow Coma Scale (GCS) rapidly lowered down to 5/15, out of which five patients developed immediate bilateral pupillary failure and abnormal breathing. All subjected to surgery within no time but out of five, two patients succumbed to death and three patients revived. On long term follow-up after six months, of all patients with pupillary failure, those who recovered were doing well (GOS-3 to 5) except significant problem in vision with little defect in ambulation and cognitive aspect of higher mental function.
Two patients in the present series were admitted with severe dementia. One was very elderly and completely bed ridden. Due to multiple co-morbidities patient underwent BHD under local anaesthesia and to our surprise both the patients recovered as per long term follow-up data collected.
Two other modality of treatment options that were practiced were primary and secondary craniotomy in the management of CSDH but their incidence was low [2,3]. The decision for primary craniotomy was taken mostly intraoperatively after encountering thick outer membrane through the burr hole. The incision was extended to make a flap and a craniotomy of 8×6 cm size was of sufficient size to deal with the maximum part of the membrane [Table/Fig-9]. Sometimes gentle scooping out of residual membrane helps clearing out of soft part of the membrane without much oozing. However, routine administration of generous luke warm saline into the subdural space was found to control oozing as well as to reduce postoperative infection. In few cases, authors have administered routine oral enzyme formulations in form of Trypsin and Chymotrypsin to facilitate natural resorption of membrane with good result though we do not have any logical proof of it to recommend routine administration in all cases.
Thick, red, angry looking membrane (SDM).
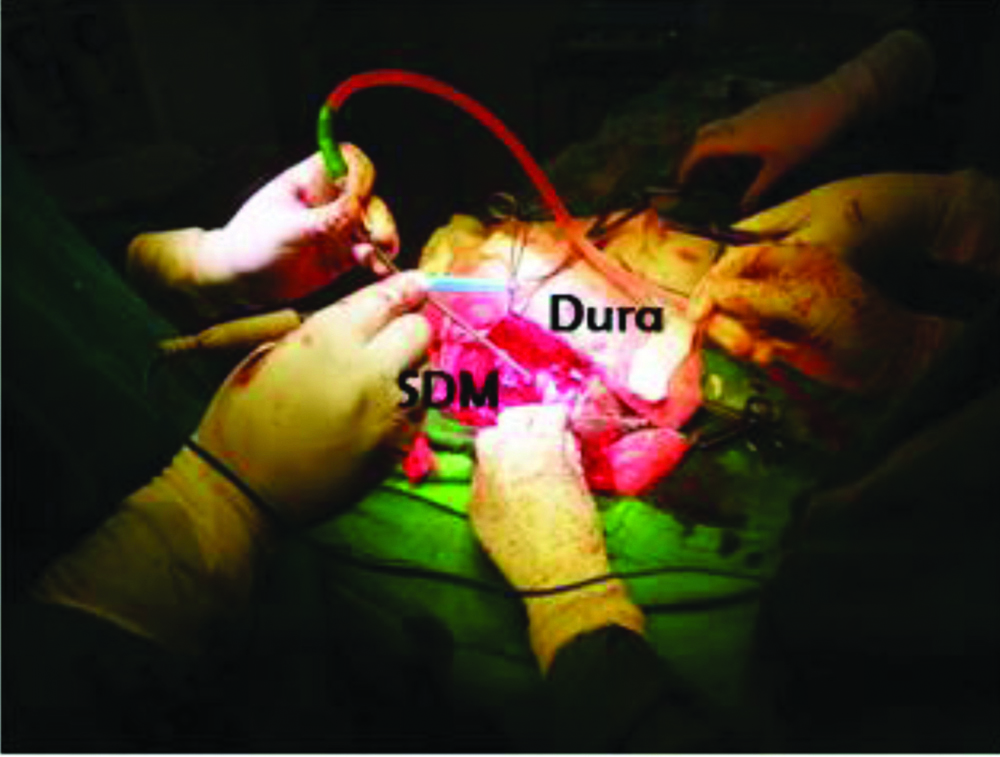
Post BHD, craniotomy as second procedure was required in only one patient. The patient had undergone BHD on left side one year back and was doing well. But re-admitted for opposite site collection with headache and disorientation. CT scan was not suggestive of any thick membrane formation however, after initial drainage there occurred rapid re-accumulation for which craniotomy was planned after supplemental MR imaging showing thick membrane. Intraoperatively, the membrane was found double the thickness of dura, red and angry looking, highly vascular and tightly covering the brain [Table/Fig-9]. Near total excision was carried out and total procedure took five hours for completion [Table/Fig-10].
After excision of the membrane.

Postoperative recovery was fine and uneventful with six month follow-up data revealed no recurrence of the lesion. In our observation, authors noted that the inner membrane was thin and flimsy in most of the cases and does not required excision. It is the parietal membrane that is responsible for micro bleeding, haematoma expansion and mass effect that needs excision. Lastly, we observed that during practice sometimes confusion arises when subdural clot is drained and another tense bluish membrane may bulge out immediately after initial drainage which suggests a second pocket of collection and should not be confused with bulging arachnoid membrane. It is to be noted that arachnoid layer and membrane layer can easily be differentiated by its characteristic appearance and needs a little confidence to puncture by young residents.
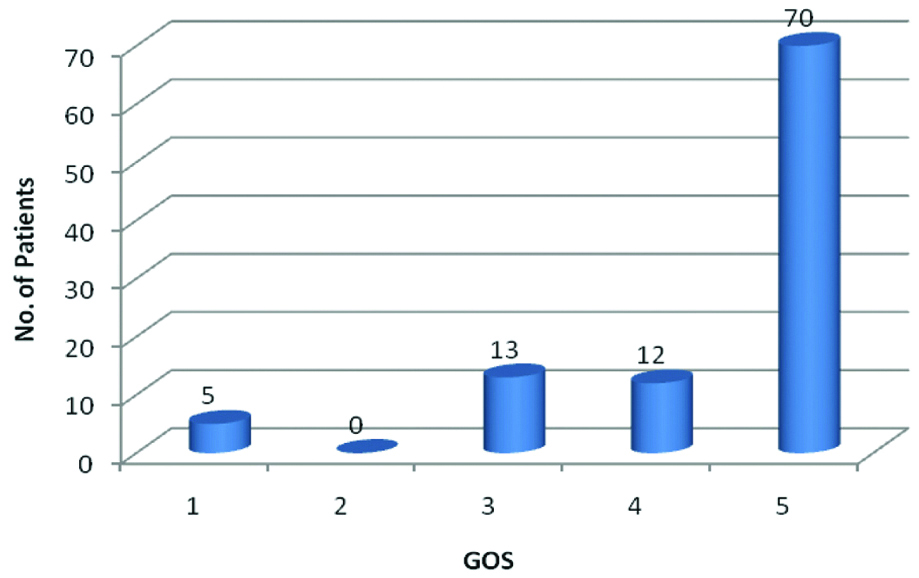
The incidence of various postoperative complications has been summarised in [Table/Fig-11]. The outcome was assessed using Glasgow Outcome Scale (GOS) [Table/Fig-12]. The overall mortality was found to be 5% in the present series.
| Postoperative complications | Percentage (%) |
|---|
| Wound infection | 0 |
| Tension pneumocephalus | 1 |
| Catheter penetration | 0 |
| Recurrence | 5 |
| Seizure (status) | 9 |
| Chest complications | 5 |
| Deep vein thrombosis | 2 |
| Mortality | 5 |
Surgical outcome using GOS scale.
(1=Death, 2=Persistence vegetative state, 3=Severe disability, 4=Moderate disability, 5=good recovery)
Discussion
Chronic Subdural Haematomas (CSDH) are so far an apparently simple to manage benign neurosurgical condition with an overall excellent prognosis. It is often joked that it is the bread and butter for many neuro-practitioners. Treatment gives an early satisfaction to surgeon as well as to the patient. It also helps in a rapid development of rapport because of early recovery point of view. However, it is not totally free of complications, infact it is to be remembered that no surgery is minor or free of controversies and complications [4]. As far as patho-physiology is concerned, inflammation takes a leading role but it is unclear why membrane formation is less apparent in very young as well as very elderly [5]. It was mostly observed in middle aged adult in our small series. The mean age group was 57.39 years compared to one study by Kitya D et al., which shows it was 60.2 years [6].
Among the clinical scenario apart from subacute CVA like presentation, many patient present with early dementia. No other study was found to have pure dementia as a presentation of chronic subdural haematoma. It is well known that chronic subdural haematomas are among the reversible causes of dementia. So, prompt investigation with slightest suspicion and earliest management is albeit essential for speedy recovery. Headache was the most common presenting symptoms in the present study which agree with other previous studies from India, Nigeria and Ghana [7]. One comparative study of clinical presentation has been summarised in [Table/Fig-13].
Comparative study of clinical spectrum.
| Clinical presentation | Present study | Kitya D et al., [6] |
|---|
| Headache | 86% | 89.6% |
| Disorientation | 67% | 71.7% |
| Memory loss | 67% | 65.5% |
| Convulsion | 9% | 11.5% |
| Limb weaknesses | 74% | 70.5 |
| Incontinence | 65% | 65.6% |
Burr Hole Drainage (BHD) is adequate enough to deal with the problem for which it is the procedure of choice worldwide [Table/Fig-8]. However, conservative management does have a role in management of CSDH in certain situations [8]. Patients having minimal collection, bilateral small collection, radiological absence of mass effect and those who are neurologically stable can be subjected to conservative management but require a close follow-up and serial CT scan. A short course of glucocorticoids does help in resolution of minimal to moderate collection and the conversion rate towards surgical intervention is around less than 10% [6]. In the present study, 94% patients underwent BHD with mortality of 5% compared to 13% mortality by Kitya D et al., [6].
Craniotomy does play a share in the management of CSDH but to a lesser degree [1,9,10]. However, one should remain prepared prior to surgery by careful studying of the imaging. In one study, it has been found that CT scan is less sensitive in identifying membranes as compared to contrast enhanced MRI. Membrane detection rate of CT is nearly 70% less as compared to MRI [7]. So accordingly, surgical site incision can be changed to make a flap if required to deal with the membrane intraoperatively [11]. In our practice, we do burr hole of a little bigger size to inspect the membrane and if it is not too thick, unlike the thickness of duramater, then mini-craniectomy does help in dealing with the problem and bigger craniotomy is avoided [6]. Internal septations are usually flimsy and require little forceful irrigation to break it.
Irrespective of the surgical techniques used, re-surgery is a possibility. In present study, it was 5% and Sah S and Rawal D, in their series reported 7.9% re-operation rate [1]. Kim JH et al., reported 18.18% patients requiring re-exploration for various regions [12]. The reported incidence of re-surgery ranges from 3-37% in a case series [1]. Authors personally do not have any experience of radial cuts in the inner layer of membrane to make decompression effect wider as narrated by Sah S and Rawal D [1].
Finally, it must be emphasised that surgery of this apparently benign entity is not without complication. Many factors ultimately affect the outcome. Age of the patient, timing of presentation, associated co-morbidity, general condition of the patient, promptness in management without further delay all affects the ultimate outcome. Importance of nursing care cannot be overemphasised in any neurosurgical patient especially in elderly [13]. Managing fluid and electrolytes and respiratory care plays a vital role in preventing untimely deterioration and complications. In our series, the patients who were lost and the patients who showed delayed recovery were mostly due to cerebral herniation which was majority of the time, central in nature causing bilateral Posterior Cerebral Artery (PCA) territory infarction. The ultimate outcome in unilateral PCA Infarction was definitely better than bilateral infarct. There is no ambiguity in opinion regarding outcome of tonsillar coning which is always harassing whatever, and however early, attempts are made towards rescue [12].
Limitation(s)
As far as the limitations are considered, it is a retrospective study. The sample size considered small and there is no control group for comparison of the result. It has been conducted in a single centre reducing its clinical significance. The study population was also heterogeneous. The study did not keep a follow-up of patients after their discharge to evaluate a long term neurological outcome.
Conclusion(s)
To conclude Chronic Subdural Haematomas (CSBH) are one of the most rewarding among neurosurgical procedures. BHD is the procedure of choice and craniotomy has a small share in its management. It is one of the reversible causes of dementia in elderly and carries an overall good prognosis.
The study highlighted three important observations i.e., one should be over vigilant in young patients with post-traumatic subacute subdural haematoma having severe thunderclap headache for they deteriorate rapidly. Secondly, alcoholic should be taken care of with atleast two antiepileptic medications for their large propencity to develop seizure and thirdly, the importance of supplemental MRI to detect the subdural membrane in doubtful and recurrent cases for proper planning of the surgical procedure. So, this study strongly recommends detail meta-analysis on above points in forth coming studies for overall better management and outcome in these groups of patients.
GCS: Glasgow coma scale; CSF: Cerebrospinal fluid; CKD: Chronic kidney disease